Abstract
Objectives: To evaluate whether the outcomes of renal grafts from living related donors more than 60 years old are acceptable, in terms of renal function and patient/graft survival. Material and Methods: Twenty-one patients who received kidneys from donors older than 60 years constituted the study group (Group 1). The control group (Group 2) consisted of 110 patients who received renal transplants from ideal donors, aged 18 to 45 years. The recipients were analyzed for posttransplantation serum creatinine, the number of acute rejection episodes and delayed graft function, and patient/graft survival. Results: The mean age of donors was 62.6 ± 2.2 years in Group 1 and 32.8 ± 7.0 years in Group 2. Recipient serum creatinine was higher on postoperative day 1, year 1, year 5 in Group 1 than that in Group 2 (536.8 ± 203.3 vs. 409.8 ± 213.8, 142.4 ± 38.2 vs. 100.3 ± 22.9, 152.6 ± 42.7 vs. 107.1 ± 22.1, respectively; all p < 0.05). Acute rejection was seen in 4 cases in Group 1 (19.0%) and in 15 cases in Group 2 (13.6%; p = 0.759). Delayed graft function was seen in two cases in Group 1 (9.5%) and in four cases in Group 2 (3.6%; p = 0.540). One-, 3- and 5-year patient survival was 100%, 100% and 100% for Group 1, and 97%, 97% and 97% for Group 2. Corresponding death-censored graft survival was 100%, 100% and 100% for Group 1, and 98%, 98% and 96% for Group 2. No significant difference was observed in terms of patient/graft survival. Conclusions: Although compromising renal function, donor age did not affect patient and graft survival in the 5-year follow-up in our study. Age alone seems not to be an exclusion criterion to living kidney donation.
Introduction
Kidney transplantation is the optimal therapeutic option for patients with end-stage renal disease (ESRD).Citation1 The waiting list for kidney transplant recipients continues to grow while the number of available organs levels off. Duration of waiting for a graft is an independent determinant of long-term posttransplant prognosis.Citation2 In China, the reduction in organ supply from the prison system and the limited organ supply from donation after cardiac death have resulted in a rapid increase in the number of organ transplantation from living related donors (LRDs), even those who are elderly. It is a matter of concern that the elderly donor renal grafts may have poor outcomes due to age-related structural and functional changes.Citation3 In this retrospective study, we evaluated the outcomes of kidney transplants from LRDs ≥60 years, compared with those from ideal ones, aged 18 to 45 year.
Patients and methods
Study subjects
Between May 2007 and December 2011, 231 living related kidney transplants were performed in our center. Donation was approved by the local ethics committee. Twenty-one patients received kidneys from donors who were ≥60 years old, and constituted the study group (Group 1). The control group (Group 2, n = 110) was composed of patients who received renal transplants from ideal donors, aged 18 to 45 years. Excluded from the study were patients who were younger than 18 years or who underwent repeat transplantation. The date of the study was chosen to ensure a minimum follow-up of 1 year. This study was approved by the institutional review board, and was in accordance with the 1975 Helsinki Declaration. Written informed consent was obtained from all patients.
Preoperative evaluation of donors
All potential donors underwent a thorough history inquiry and a rigorous examination. Preoperative evaluation included hematological and biochemical screening, urine microscopy, chest X-ray, electrocardiogram, renal sonogram, HLA typing and matching, 99mTc DTPA renal scan and computerized tomography angiography with 3D reconstruction of the renal hilum. Potential donors with diabetes, proteinuria or severe heart or liver diseases were excluded. Mild hypertension was not regarded as an exclusion criterion.
Operative procedures and immunosuppressive protocols
All donors underwent open nephrectomy through a retroperitoneal flank incision. The left kidney was the first choice unless with multiple arteries. Transplant procedures were performed using the usual technique in the right or left iliac fossa with vascular anastomoses to the external iliac artery and vein. Ureteroneocystostomy was performed using the extravesical technique with a double-J ureteral catheter.
Immunosuppression consisted of induction therapy with methylprednisolone (500 mg/d for 3 days) and basiliximab (20 mg pretransplant and on posttransplant day 4)/thymoglobulin (50 mg/d for 3 days), and sequential triple maintenance therapy. All patients were treated with cyclosporine- or tacrolimus-based immunosuppression (trough concentrations 150–200 ng/mL or 6–10 ng/mL, respectively), including mycophenolate mofetil (2 g/day)/mycophenolate sodium (1.44 g/day) and prednisone (30 mg/day). The dosage of immunosuppression tapered along with the elapse of time. Acute rejection episodes were initially treated using methylprednisolone pulsed therapy (500 mg × 3 d). Thymoglobulin was administered in instances of corticosteroid-resistant rejection.
Follow-up of recipients
Recipient serum creatinine at 1 day, 7 days, 1 month, 3 months, 6 months, 1 year and every year thereafter following transplantation was recorded. Corresponding glomerular filtration rate (GFR) was estimated using the Cockcroft--Gault formulation. The number of acute rejection (AR) episodes and delayed graft function (DGF) was recorded. Graft and patient survivals at 1, 3 and 5 years after transplantation were calculated. AR was either clinically diagnosed or biopsy-proven. DGF was defined as the requirement of dialysis within 1 week post transplantation.
Statistical analysis
Statistical analysis was performed with SPSS 13.0 software (Chicago, IL). Data were expressed as mean ± SD for continuous variables and as n (%) for categorical ones by default. Continuous variables were compared using student’s t-test. Categorical variables were compared using χ2 test. Patient and graft survival were assessed with Kaplan–Meier curves and compared with the log-rank test. A p-value <0.05 was considered statistically significant.
Results
Baseline characteristics
Donor and recipient characteristics at the time of transplant are shown in . Mean donor age was 62.6 ± 2.2 (60 to 66) years in Group 1 and 32.8 ± 7.0 (21 to 44) years in Group 2. There were no differences between the groups according to donor gender, body weight, GFR of the kidney graft and serum creatinine. There were no differences between the groups according to recipient age, gender, body weight, serum creatinine, duration on dialysis and donor–recipient HLA mismatches. Both warm ischemic time and cold ischemic time are comparable between the two groups. The relationships of the donor to the recipient were parent (n = 20) and spouse (n = 1), in Group 1, and parent (n = 10), child (n = 2), sibling (n = 47), spouse (n = 3) and other related (48), in Group 2. The median follow-up was 49 months (range 12–67 months) and 55 months (range 12–67 months), respectively.
Table 1. Baseline characteristics of study population grouped according to donor age.
Graft function
Mean serum creatinine between the two groups during the follow-up period is compared in . It was significantly higher in Group 1 at all the time points we selected, while eGFR was consistently lower (). AR was seen in 4 cases in Group 1 (19.0%) and in 15 cases in Group 2 (13.6%; p = 0.759). DGF was seen in two cases in Group 1 (9.5%) and in four cases in Group 2 (3.6%; p = 0.540).
Figure 1. Differences in postoperative eGFR by donor age difference. Data were expressed as means – SD for Group 1 and means + SD for Group 2. eGFR was significantly lower at all the eight time points in Group 1. eGFR: estimated glomerular filtration rate, measured by Cockcroft--Gault formulation.
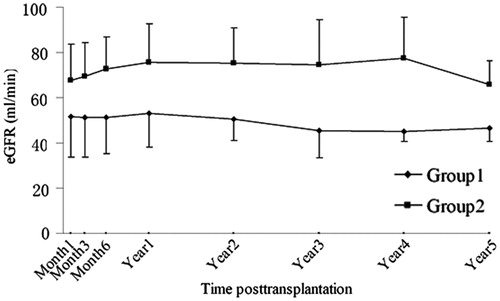
Table 2. Differences in postoperative creatinine by donor age difference (μmol/L).
Patient and death-censored graft survival
One-, 3- and 5-year patient survival was 100%, 100% and 100% for Group 1, and 97%, 97% and 97% for Group 2. No significant difference was observed in terms of patient survival (p = 0.447). Corresponding death-censored graft survival was 100%, 100% and 100% for Group 1, and 98%, 98% and 96% for Group 2. It did not significantly differ in the two groups (p = 0.473).
Discussion
Kidney transplantation remains the best option for treating ESRD, because of prolongation of survival and improved quality of life. As the number of individuals with ESRD grows, the discrepancy between available donor organs and patients waiting for transplantation widens. As a result, many transplant centers are increasingly utilizing donors that would have not been considered in the past.Citation4–6
The role of elderly LRDs remains controversial. Many transplant programs reported that they do not have an upper age limit for living donors any more.Citation7 Others are reluctant about elderly donors because of age-related decline in glomerular filtration rate.Citation8 We had previously confirmed that donating a kidney is safe to elderly donor.Citation9 In this study, we focused on the outcome of recipients. Although GFR of the graft-to-be was comparable between the two groups, it was lower in Group 1 at all the posttransplantation time points selected, which is in accordance with results of the majority of previous studies.Citation10–12 However, it was stable in the 5-year follow-up.
Although it has been noted that recipients of kidneys from older donors had poorer recipient and graft survival than recipients of kidneys from younger ones,Citation10,Citation11,Citation13,Citation14 this trend has not been confirmed in our study. When analyzing the impact of donor age on graft outcomes, several other confounding variables should be taken into account after adjusting for recipient factors. It is reported that donor GFR, cholesterol levels and systolic blood pressure are important and independent correlates of recipient allograft function, and the presence of multiple individual factors associated with poor outcome seemed to have a cumulative effect.Citation15 Furthermore, some studies did not specify whether graft survival was censored for death. Uncensored graft survival considers death with a functioning graft to be graft loss and would underestimate survival in older recipients.
Our study did not show a significant difference between the two groups in AR rates. The powerful quadruple immunosuppressive therapy used in all recipients probably was responsible for a relative lower incidence of rejection episodes. Lee et al. reported that although the acute rejection rate within the first year post transplantation was greater among donor–recipient age difference ≥20 years, it did not affect graft or patient survivals. They did not affirm the absolute effect of donor age.Citation16
We acknowledge a few limitations of our study. Stratification of confounding factors has not been performed because of the few number of enrolled recipients of elderly donor graft. The follow-up period was relatively short.
Conclusions
Although compromising renal function, donor age did not affect patient and graft survival in the 5-year follow-up in our study. In the current shortage of renal graft, age alone seems not to be an exclusion criterion to living kidney donation. Other donor predicting factors of allograft success should be established and evaluated synthetically in donor assessment and selection.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Wolf RA, Asbby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation and recipients of a first cadaver transplant. N Engl J Med. 1999;341(23):1725–1730
- Meier-Kriesche H, Port FK, Ojo AO, et al. Deleterious effect of waiting time on renal transplant outcome. Transplant Proc. 2001;33:1204–1206
- Zhou XJ, Rakheja D, Yu X, et al. The aging kidney. Kidney Int. 2008;74:710–720
- Yolanda TB, Glen EL, Anthony MD, et al. Diabetic kidneys can safely expand the donor pool. Transplantation. 2002;74:141–145
- Navarro AP, Sohrabi S, Wilson C, et al. Renal transplants from category III non-heart-beating donors with evidence of pre-arrest acute renal failure. Transplant Proc. 2006;38:2635–2636
- Stefan GT, Peter N. The marginal kidney donor. Curr Opin Urol. 2002;12:101–107
- Mandelbrot DA, Pavlakis M, Danovitch GM, et al. The medical evaluation of living kidney donors: a survey of US transplant centers. Am J Transpl. 2007;7:2333–2343
- Iordanous Y, Seymour N, Young A, et al. Recipient outcomes for expanded criteria living kidney donors: the disconnect between current evidence and practice. Am J Transpl. 2009;9:1558–1573
- Qiu J, Cheng LZ, Li J, et al. Efficacy and safety of elder donor in living kidney transplantation. CNDT. 2009;18:343–347
- Naumovic R, Djukanovic L, Marinkovic J, et al. Effect of donor age on the outcome of living-related kidney transplantation. Transplant Int. 2005;18:1266–1274
- Neipp M, Jackobs S, Jaeger M, et al. Living kidney donors >60 years of age: is it acceptable for the donor and the recipient? Transplant Int. 2006;19:213–217
- Sahin S, Manga SG, Turkmen A, et al. Utilization of elderly donors in living related kidney transplantation. Transplant Proc. 2006;38:385–387
- Giessing M, Slowinski T, Deger S, et al. 20-year experience with elderly donors in living renal transplantation. Transplant Proc. 2003;35:2855–2857
- Lim WH, Clayton P, Wong G, et al. Outcomes of kidney transplantation from older living donors. Transplantation. 2013;95:106–113
- Issa N, Stephay B, Fatica R, et al. Donor factors influencing graft outcomes in live donor kidney transplantation. Transplantation. 2007;83:593–599
- Lee YJ, Chang JH, Choi HN, et al. Donor-recipient age difference and graft survival in living donor kidney transplantation. Transplant Proc. 2012;44:270–272
