Abstract
Objective: To evaluate the association between acute kidney injury (AKI) and long-term survival in lung transplant patients. Methods: Clinical data of 88 patients who underwent lung transplantation (LTx) were retrospectively analyzed at our institution from September 2002 to December 2011. Postoperative AKI was defined and divided into three groups based on creatinine criteria from the Acute Kidney Injury Net (AKIN) classification. A multivariable logistic regression model evaluated risk factors for AKI. Primary outcome was 5-year mortality. Risk adjusted multivariable COX proportional hazards regression examined the association of AKI with mortality. Results: A total of 47 (53.40%) patients developed AKI (27 with AKIN1, 20 with AKIN2-3) in the first week after LTx. Multivariate analysis showed pre-LT (pre-lung transplant) hypertension (OR 1.37 [0.06–2.68], p = 0.041) and mechanical ventilation (OR 0.05 [0.01–0.09], p = 0.022) were risk factors for postoperative AKI. Five-year survival rates in the non-AKI, AKIN1, and AKIN2-3 groups were 48.8%, 37.0%, 30.0%, respectively (p = 0.041). Adjusted for age, sex, type and cause of LT, hypertension and diabetes, the hazard ratio for death was 1.481 ([1.040–2.107]) for AKI. Conclusions: The occurrence of AKI after LTx is common. Severe AKI would increase long-term mortality risk. Several variables, including pre-LT hypertension and mechanical ventilation, are associated with AKI after LTx.
Introduction
The postoperative period after lung transplantation (LTx) remains critical due to several complications,Citation1 and acute kidney injury (AKI) is an increasingly important problem among them.Citation2–4 Regardless of the underlying cause, AKI is associated with increased long-term mortality.Citation5 Recent data in non-transplant patients have demonstrated that even mild and self-limited AKI events predict worse outcomes.Citation6
However, data on the prevalence of AKI after LTx and its effect on mortality are scarce and contradictory. Rocha et al. reported that AKI (defined as postoperative doubling of serum creatinine (SCr)) occurred in 56% of patients after LTx, and the long-term mortality increased in patients who required dialysis.Citation7 Conversely, the review by Jacques et al. found that AKI (the RIFLE criteria) occurred in 39% of patients, and there was no association between AKI and mortality.Citation8 Different definitions for AKI might be the reason of this divergence and even obstruct comparisons among studies. To unify the standard, a new international definition for AKI, known as the Acute Kidney Injury Network (AKIN) criteria, is set forth.Citation9 According to this standard, AKI is stratified into three grades of increasing severity (AKIN1-3).
The objective of this study is to examine the incidence and predictive factors of AKI after LTx, and its effect on 5-year mortality according to the AKIN classification.
Materials and methods
Study population
From September 2002 to December 2011, we performed a retrospective cohort study of 113 patients who underwent LTx at the Wuxi People’s Hospital, Jiangsu, China. All transplantations were approved by the ethics committee of Wuxi People’s Hospital. Patients’ demographics, laboratory data, and outcomes were obtained from electronic medical records and paper records. All patients were included except for 25 patients: 2 had intra-operative death, 1 had heart- LTx, 2 had prior liver transplant, 11 had missing data, and 9 were lost to follow-up.
Baseline demographic and intra-operative data of the patients are shown in . Baseline creatinine level was obtained before LTx. After LTx, SCr was recorded daily for the first week, then at 6 months, and every year subsequently. The Modification of Diet in Renal Disease (MDRD) equation was used to calculate the estimate glomerular filtration rate (eGFR). Cardiopulmonary bypass (CPB) was mainly used before 2006, and it was replaced by extracorporeal membrane oxygenation (ECMO) after that. CPB or ECMO was used selectively in patients with severe pulmonary hypertension, in patients intolerant of single lung ventilation, and in patients who had severe primary graft dysfunction after one-side LTx.
Table 1. Characteristics of recipients of lung transplant by acute kidney injury statusa.
AKI was defined by an increase in creatinine of ≥0.3 mg/dL (26.5 µmol/L), or >1.5-fold rise in SCr within 48 h from baseline in the first week after surgery. Patients were classified into stage1 (AKIN1), stage2 (AKIN2) and stage3 (AKIN3) according to the AKIN classification.Citation9 AKIN2 and AKIN3 were combined into one group (AKIN2-3) as severe AKI. The urine output criterion was not used because diuretic could influence urinary volume. The primary endpoint was 5-year mortality.
Immunosuppressive regimen
Basiliximab was used as induction therapy on postoperative days 1 and 4, except for cystic fibrosis, bronchiectasis, and severe infection. Maintenance immunosuppressive therapy was initiated in the early postoperative period and consisted of methylprednisone, calcineurin-inhibitor, and mycophenolate mofetil. Patients received either Cyclosporine or Tacrolimus. Trough whole blood levels for cyclosporine of 300–400 ng/mL were targeted in the first 3 months, postoperatively, 200–300 ng/mL between 3 and 6 months, and 100–200 ng/mL beyond 6 months. Since 2009, tacrolimus has been used instead of cyclosporine. For tacrolimus, trough whole blood levels of 10–15 ng/mL were targeted in the first 3 months, postoperatively, and 8–12 ng/mL beyond 3 months. Azathioprine or mycophenolate mofetil dosages were adjusted to maintain a WBC count over 4000 µl-1.
Statistical analysis
The results are presented as mean with standard deviation or median with inter-quartile range for continuous variables depending on variable distribution. Categorical variables are presented as frequencies with percentages. In univariate analysis, comparisons among groups were analyzed using one-way analysis of variance for normally distributed continuous variables, and chi-square test for categorical variables. Multivariable logistic regression analyses were used to identify covariates associated with AKI. In addition to variables associated with each outcome on exploratory univariate analysis (p < 0.2), those with biological plausibility were incorporated in a backwards stepwise fashion into the multivariable model. Risk adjusted multivariable COX proportional hazards regression examined the association between AKI and mortality.
Five-year mortality was estimated through the Kaplan–Meier method, and survival curves were compared by long-rank test. The cases lost to follow-up were censored at their last observation. All statistical tests were two-sided, and differences were considered statistically significant with p value less than 0.05. Results were analyzed via SPSS software (version 17.0; SPSS-IBM Inc., Chicago, IL).
Results
The incidence of AKI
Eighty-eight lung transplant recipients at our institution were analyzed. summarized the characteristics of these recipients with a mean follow-up 2.10 ± 2.04 years after LTx. The mean age was 53.29 ± 13.37 years, and 76.1% were men. The frequencies of hypertension and diabetes were 21.6% and 15.9%. The mean pre-operative SCr was 60.65 ± 19.31 µmol/L. The most common diagnoses of LTx were idiopathic pulmonary and chronic obstructive disease.
Forty-seven patients (53.40%) developed post-operative AKI within 1 week: 27 had AKIN1 (30.7%), 11 had AKIN2 (12.5%), and 9 had AKIN3 (10.2%). AKI occurred at 2.4 ± 3.2 post-operative days. Three patients with AKIN3 had been treated with continuous renal replacement treatment and died of multiple organ failure finally.
As shown in , the frequency of preoperative hypertension in AKI2-3 group is the highest among groups (p = 0.048), but the level of perioperative MBP was the lowest (pAKIN2-3 VS non-AKI <0.001; pAKIN2-3 VS AKIN1 = 0.024). More than a half (n = 45, 51.1%) of patients were in need of ECMO, especially those with non-AKI (pECMO = 0.002). Compared with these of patients with non-AKI, the durations of mechanical ventilation for those with AKI were significantly longer (pMV < 0.001). Additionally, there was a significant increase in the incidence of sepsis with the increasing severity of AKI (p = 0.027).
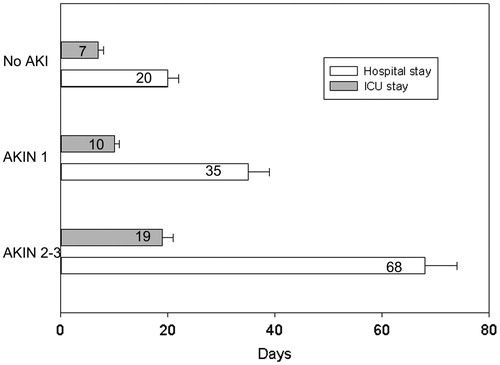
Of the total cohort, the median hospital stay was 30 (inter-quartile range 15, 80) days, and the median ICU stay was 11 (inter-quartile range 8, 20) days. The median length of hospital stay and ICU stay shown a significant difference with the increasing severity of AKI ().
Assessment of predictive factors
Eight factors including gender, hypertension, perioperative MBP, inotropic support, use of aprotinin, mechanical ventilation, ECMO support, and sepsis were involved in multivariate analysis. Pre-LT hypertension (OR 1.37; p = 0.041) and Duration of mechanical ventilation (OR 0.05; p = 0.022) predicted higher risk of any AKI occurring after LTx, whereas perioperative MBP (OR −0.06; p < 0.001) and ECMO support (OR −1.26; p = 0.037) were protective factors for it.
Long-term renal function and survival
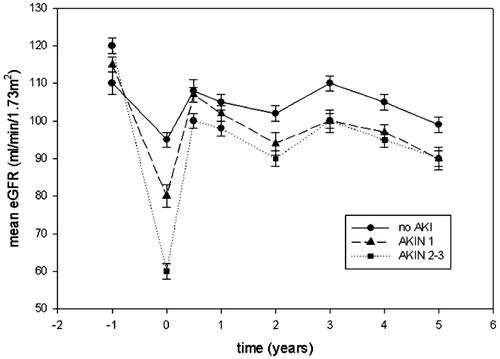
No patients developed chronic kidney injury (CKD) in the follow-up. Wehbe et al.Citation16 described development of CKD after LTx with a cumulative incidence of 25%. The reason for the lack of CKD in our study may be insufficient cases. The evolution of renal function was examined by observing 36 patients who had survived over 5 years (20 for no AKI group, 10 for AKIN1 group, and 6 for AKIN2-3). There was a similar evolution of estimate GFR levels among all groups (). At 5 years, patients with any AKI showed a non-significant decrease in eGFR when compared to those with non-AKI (non-AKI: 99 ± 11.8 mL/min·1.73 m2, AKIN1: 90 ± 5.1 mL/min·1.73 m2, AKIN2-3: 90 ± 4.7 mL/min·1.73 m2; p = 0.783).
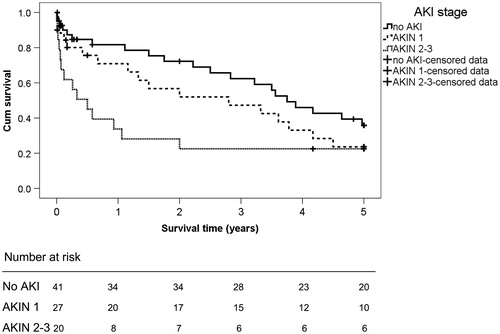
The overall 5-year survival rate after LTx was 40.9% (48.8% for non-AKI, 37.0% for AKIN1, 30.0% for AKIN2-3). showed that 5-year survival rates were gradually reduced with increasing severity of AKI (AKIN1 vs. no AKI, long-rank p = 0.231; AKIN2-3 vs. no AKI, long-rank p = 0.014; AKIN2-3 vs. AKIN1, long-rank p = 0.169). From the Cox proportional hazard model (adjusting for age, sex, type and cause of LT, hypertension and diabetes), any AKI event was independently predictive of death (HR 1.481; 95% CI, 1.040–2.107).
Discussion
In this study, we evaluated the incidence and long-term outcomes of AKI after LTx. Our results revealed that AKI is a common complication after LTx, and severe form of AKI after transplant is predictive of higher long-term mortality.
AKI is a common occurrence after LTx.Citation2–4 In our study, the incidence of post-operative AKI after LTx was 53.40%, which is lower than findings of other studies.Citation3,Citation10 This is potentially due to differences in the study population, and the definition of AKI. Compared with historical definitions of AKI, the AKIN criteria is a more contemporary classification that specifies the window time of diagnosis in 48 h.Citation9
There are several potential mechanisms partly explaining high rates of the development of AKI after LTx. First of all, our study found that perioperative MBP was a protective factor of AKI (). Hemodynamic instability due to surgical intervention and massive hemorrhage leads to renal hypoperfusion and ischemia reperfusion injury. Second, patients accompanied with pre-LTx hypertension exhibited a higher risk of AKI. It is noteworthy that the blood pressure levels before operation were similar among all groups (). These results suggest that patients with hypertension have less renal reserve function and are easy to be injured. Third, duration of mechanical ventilation was a risk factor for AKI (). In a previous study, prolonged mechanical ventilation increased the development of AKI in critically ill patients.Citation11 There may be three proposed mechanisms: long blood gas disturbances leading to hypoxemia, and subsequent neurohumoral-mediated effects on renal blood flow during mechanical ventilation; redistribution of intra-renal blood flow and stimulation of hormonal and sympathetic pathways could influence renal hemodynamic, thus decreasing renal blood flow; inflammatory reaction to mechanical ventilation with pulmonary mediators release into systemic circulation.Citation12 The last factor identified as predictive for development of AKI after LTx was ECMO (). Previous studies have demonstrated that lung injury can have distant effect on the kidney by releasing inflammation mediators, such as IL-6.Citation13,Citation14 It is suggested that ECMO support can improve lung transplant recipients’ oxygenation, and alleviate inflammatory reaction, thereby protecting renal function.Citation15
Table 2. Predictive factors associated with AKI in LTx patients.
We herein evaluated the effect of AKI on long-term mortality. Survival rates were gradually reduced by increasing severity of AKI (). However, only severe AKI group (AKIN2-3) had a statistically decrease of survival rate when compared with non-AKI group. In further analysis, the hazard ratio for death was 1.481 for AKI. These results shed light on the fact that patients with AKI are more critical than non-AKI ones and AKI could serve as a prognostic marker of increased long-term mortality risk. Animal models also confirmed that AKI could induce tissue injury in other organs by activating inflammation and apoptosis. In spite of serum creatinine down to baseline after the episode, AKI may result in permanent injury to other vital organs and influence future survival.
Mounting studies indicated that some lung transplant patients developed end-stage renal disease on long-term follow-up.Citation16,Citation17 In our study, all groups of patients experienced decreased renal function in the immediate post-operative period; however, resumed their renal function in the months after LTx (). None of our survivors’ progress to CKD might be due to limited number of survival patients and some loss to follow-up. So a large, multicentre, and well-characterized research is needed.
To our knowledge, this is the first study about mortality of lung transplant patients from Asian. There are some limitations existing in our study, including retrospective single-center design and limited number of patients. Furthermore, the use of the MDRD formula to predict renal function may overestimate the real GFR because of the secreted portion of serum creatinine. However, pre-operative, post-operative, and long-term GFR were obtained using the same calculation.
In conclusion, severe AKI after LTx is significantly associated with high long-term mortality. Pre-LT hypertension and mechanical ventilation were risk factors for AKI after LTx, while perioperative MBP and ECMO support were protective factors for it. These predictive factors should be considered synthetically to avoid renal risks as much as possible and prolong lung transplant recipients’ life span.
Declaration of interest
The authors declare no conflicts of interests. The authors alone are responsible for the content and writing of this article.
Acknowledgements
Partial results will be presented at the World Congress of Nephrology, Hong Kong, China, 2013.
References
- Arango TE, Quero RMI, Robles AJC, et al. Postoperative complications in the intensive care unit following lung transplantation in adults: results in university hospital reina sofia. Transplant Proc. 2012;44(9):2663–2665
- George TJ, Arnaoutakis GJ, Beaty CA, et al. Acute kidney injury increases mortality after lung transplantation. Ann Thorac Surg. 2012;94(1):185–192
- Arnaoutakis GJ, George TJ, Robinson CW, et al. Severe acute kidney injury according to the RIFLE (risk, injury, failure, loss, end stage) criteria affects mortality in lung transplantation. J Heart Lung Transplant. 2011;30(10):1161–1168
- Arnaoutakis GJ, George TJ, Robinson CW, et al. Severe acute kidney injury according to the RIFLE criteria affects mortality in lung transplantation. J Heart Lung Transplant. 2011;30(10):1161–1168
- Lafrance JP, Miller DR. Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol. 2010;21(2):345–352
- Coca SG, Yusuf B, Shlipak MG, et al. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;53(6):961–973
- Rocha PN, Rocha AT, Palmer SM, et al. Acute renal failure after lung transplantation: incidence, predictors and impact on perioperative morbidity and mortality. Am J Transplant. 2005;5:1469–1476
- Jacques F, EI-Hamamsy I, Fortier A, et al. Acute renal failure following lung transplantation: risk factors, morality, and long-term consequences. Eur J Cardiothorac Surg. 2012;41(1):193–199
- Mehta RL, Kellum JA, Shah SV, et al. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31 . doi: 10.1186/cc5713
- Gonzalez CA, Llorca J, Suberviola CB, et al. Acute renal failure in lung transplantation: incidence, correlation with subsequent kidney disease, and prognostic value. Arch Bronconeumol. 2008;44(7):353–359
- Paudel MS, Wig N, Mahajan S, et al. A study of incidence of AKI in mechanical ventilation ill patients. Ren Fail. 2012;34(10):1217–1222
- Kuiper JW, Vaschetto R, Della Corte F, et al. Bench-to-bedside review: ventilation-induced renal injury through systemic mediator release-just theory or a causal relationship? Crit Care. 2011;15(4):228
- Ahuja N, Andres-Hernnando A, Altmann C, et al. Circulating IL-6 mediates lung injury via CXCL1 production after acute kidney injury in mice. Am J Physiol Renal Physiol. 2012;303(6):F864–F872
- White LE, Hassoun HT. Inflammatory mechanisms of organ crosstalk during ischemic acute kidney injury. Int J Nephrol. 2012; 2012, Article ID 505197
- Javidfar J, Brodie D, Iribarne A, et al. Extracorporeal membrane oxygenation as a bridge to lung transplantation and recovery. J Thorac Cardiovasc Surg. 2012;144(3):716--721
- Wehbe E, Brock R, Budev M, et al. Short-term and long-term outcomes of acute kidney injury after lung transplantation. J Heart Lung Transplant. 2012;31(3):244–251
- Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report-2012. J Heart Lung Transplant. 2012;31(10):1073–1086