Abstract
Background: The pathological patterns underlying PNS in adult are poorly studied in Central China. Methods: This is a retrospective analysis of the clinical and pathologic data involving 627 adult patients with PNS who have been finished the renal biopsies from January 2009 to September 2012 in XiangYa 2nd Hospital of Central South University. Patients enrolled in our study were all from Central China. Results: There were 379 males and 248 females, formed the ratio of 1.53:1. There existed three main sorts of pathological patterns underlying PNS: membranous nephropathy (MN) 26.63%, minimal change disease (MCD) 23.60%, IgA nephropathy (IgAN) 23.39%. Among all biopsies, the proportion of FSGS underlying PNS increased from 5.8% during the period from 2009 to 2010 to 14.7% during the period from 2011 to 2012. The most common complication of PNS was infectious diseases, and MCD underlying PNS ran a higher risk of encountering acute renal injury. IgAN had the highest incidence of hematuresis. The common pathological patterns of PNS differed in age-brackets: IgAN and MCD were the main pathological lesions in patients aged from 16 to 30 years; MN mostly occurs in patients over 30. MCD was the dominating pathological lesions underlying IgAN which expressed as PNS. Conclusions: (1) MN was the most frequent pathological pattern underlying PNS, the proportion of FSGS underlying PNS increased during the last 2 years. (2) The common pathological patterns of PNS differed in age-brackets and pathological patterns correlated to the complications or comorbidities of PNS to some extent.
Introduction
It has been more than 60 years of history since Iversen et al.Citation1 successfully implemented renal biopsy in 1951. With the development of the technology of renal biopsy and advance of people’s health awareness in China, renal biopsy plays an increasingly important role in the diagnosis of kidney diseases. And renal biopsy is the most valuable inspection method of pathological diagnosis of kidney disease. It can provide objective facts for confirming diagnosis and therapeutic schedule, judging curative effect and prognosis. It is the “golden standard” of kidney diseases.
Most data around the word reported that NS was the most frequent clinical presentation of glomerular diseases.Citation2–8 However, a few counties such as Japan and Italy reported a higher frequency of asymptomatic urinary abnormalities (AUA).Citation9,Citation10 The pathogenesis of PNS is complex and explicit diagnosis depends on combining clinical, laboratory data and pathologic examination. The pathological patterns of PNS almost cover all the pathological patterns of primary glomerular diseases. The underlying etiology of NS is variable across the word. In adults, membranous nephropathy (MN) traditionally has been considered the most common cause of nephrotic syndrome (NS). However, throughout the pathological studies in the past three decades, FSGS of PNS had received increasing attention. A number of published reports suggesting a significant increase in the proportion FSGS among both white, black and Hispanic patients in the last three decades.Citation11–15 Furthermore, data from Pakistan, Brazil, India, USA and South AfricaCitation5,Citation13,Citation16–18 indicated FSGS as the most common reason for PNS.
However, in Northern China, Taiwan province of China, Japan, SpainCitation10,Citation19–22 and so on, MN was still the most frequent diagnosis. And in Korea, Denmark and Northeast China,Citation23–25 MCD was the commonest cause of primary nephrotic syndrome. The pathological patterns of PNS in adult are poorly studied in Central China. In order to get a better understanding of its spectrum of pathological patterns in the Central China, we had a retrospective analysis of clinical and pathological data from the patients involved in our study as follows.
Materials and methods
Objects and standards of research
We collected the data of 627 inpatients that have been finished the renal biopsies from January 2009 to September 2012 in our hospital. All the patients met with the following criteria: (1) heavy proteinuria (>3.5 g/24 h), (2) Hypoalbuminemia (<30 g/L), (3) hyperlipidemia and (or) generalized edema, (4) having been excluded lupus nephritis, systemic-vasculitis kidney injury, hepatitis B associated glomerulonephritis, diabetic nephropathy, tumor associated glomerulonephritis and other secondary nephritic syndromes and (5) all the patients have signed a piece of informed consent form.
Methods
We collected the data from all the adult patients including: (1) clinical information: whether they had edema, gross hematuria, elevation of blood pressure, arthralgia, canker sore, symptoms of complications or not. (2) Laboratory findings: results of urinary sediment, 24-h urinary protein quantity, serum albumin, serum triglyceride, serum cholesterol, hematuric Bence–Jone protein, a full set of hepatitis, a full set of lupus, antiglomerular basement membrane antibody (AGBM), anti-MPO antibody, anti-PR3 antibody and so on. (3) Pathologic data: all the renal biopsies were taken under the guidance of B ultrasound and 1–2 items of specimens were gathered. The specimens of each patient were stained by hematoxylin and eosin (H&E), Jones methenamine silver, periodic acid Schiff (PAS), Masson trichrome and analyzed by light microscopy (LM). Immunofluorescence (IF) used polyclonal antisera against human IgG, IgM, IgA, C3, C1q, kappa and lambda light chains, and then visualized under the epifluorescence microscope in the dark. Patients over 40 years are routinely stained by Congo red. About 72.9% patients were observed by electronic microscopy. The classification of pathologic patterns is based on the WHO criteria of histological classification of glomerular disease (issued in 1982, modified in 1995) and the diagnostic standards made at the national seminar (China) on the diagnosis of the pathology of the renal biopsy in 2001.
Patients were divided into six groups according to different ages at the time of renal biopsy: 16–20, 21–30, 31–40, 41–50, 51–60 and >60 years. Further analysis was performed by grouping patients into two periods according to a 2-year interval, 2009–2010 (period 1) and 2011–2012 (period 2).
Data analysis
The measurement data were shown as mean ± SD, and the enumeration data were expressed by percentages. The Fisher’s exact and χCitation2 test were used to compare qualitative variables. p Values of <0.05 are considered to be statistically significant.
Results
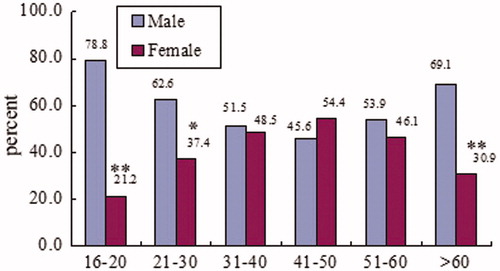
In this study, 379 patients were males, the rest were females, forming the ratio of 1.53:1, and the age of them ranged from 16 to 70 years with the average of 34.51 ± 12.5 years, with ages between 16 and 50 years dominating 72.41%. A male predominance was observed at any age except 41–50 years, however, only 16–20, 21–30 and >60 years age groups showed statistically significant difference. Among the male adult patients, 16–30 years was the dominating age group, whereas 41–50 years was the foremost age group among female. The combined age and sex distribution pattern is shown in .
Pathological patterns underlying primary nephrotic syndrome are shown in .
Table 1. Frequency distribution of different pathological patterns in 627 primary nephrotic syndrome.
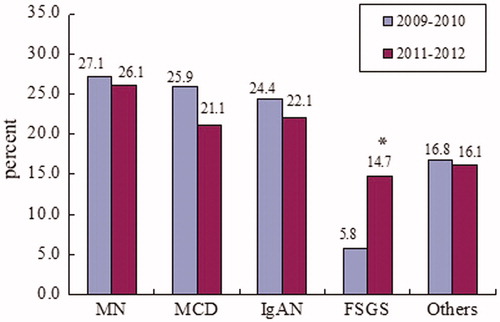
In our study, 2009 and 2010 had a similar spectrum of pathological patterns underlying PNS and this condition also existed in 2011 and 2012 (data not shown). However, comparing findings during the period from 2009 to 2010 to the period from 2011 to 2012, a significant difference in the distribution of diagnoses was detected. As shown in , the relative frequency of FSGS was increased from 5.8% during the 2009–2010 period to 14.7% during the 2011–2012 period (p < 0.005). In contrast, we found the relative frequencies of MN, MCD, IgAN slightly decreased.
Figure 2. Changing spectrums of the four main pathological patterns underlying PNS from 2009 to 2012. *p < 0.005. MN, membranous nephtopathy; MCD, minimal change disease; IgAN, IgA nephropathy; FSGS, focal segmental glomerulosclerosis; Others, pathologic types mentioned before except MN, MCD, IgAN and FSGS.
The common pathologic types of PNS differed in age groups: In our study, IgAN and MCD were both common pathological lesions for primary nephrotic syndrome patients aged from 16 to 30 years and MN was the most common pathological lesion for patients over 30 years. Furthermore, as the growth of their age, the percentage of MN increased. The relationship between ages and pathological patterns of PNS is shown in .
Table 2. The relationship between ages and pathological patterns of PNS.
The relationship between clinical features and pathological patterns are shown in : Every patient in this group all had a history of significant edema. The infectious diseases were the most common complication: 156 patients (24.9%) had evidence of infection and comprised 83 patients with respiratory infections, 65 ones with urinary system infection and others. About 25 (4.0%) patients met with acute kidney injury. Among the various pathological patterns, MCD combined with acute kidney injury was regularly detected. The infrequent complications inquired were pulmonary embolism in 8 patients and deep vein thromphlebitis in three patients. There were 228 patients (36.4%) amalgamated hematuria, and a vast majority of them were microscopic hematuria. Various pathologic types differed in the occurrence rates of hematuria, with the highest frequency of IgAN, dominating 93.05% in the groups. About 85 cases (13.6%) experienced high blood pressure (which excluded essential hypertension), MN combining with renal hypertension was more frequent than other pathological types.
Table 3. The clinicopathological correlations of FINS.
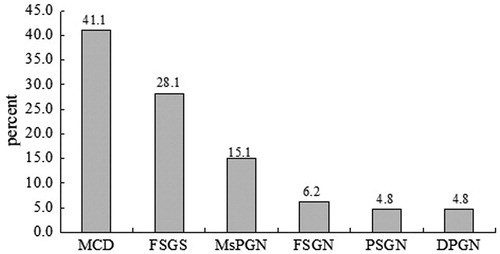
Pathological patterns underlying IgAN with primary nephrotic syndrome are shown in and turned for 60 patients (41.1) of MCD type, 41 patients (28.1%) of FSGS type, 22 patients (15.1%) of MsPGN type, 9 patients (6.2%) of FSGN type, 7 patients (4.8%) of PSGN and DPGN types.
Figure 3. Frequenct distribution of different pathological patterns underlying IgAN with primary nephritic syndrome. MCD, minimal change disease; FSGS, focal segmental glomerulosclerosis; MsPGN, mesangioproliferative glomerulonephritis; FSGN, focal segmental glomerulonephritis; PSGN, proliferative segmental glomerulonephritis; DPGN, diffuse proliferative glomerulonephritis.
Discussion
In the current study, we investigated the clinical and pathological data of 627 cases of adult PNS from January 2009 to September 2012 in a single renal centre. Light microscopy (LM) and immunofluorescence (IF) was performed on all the biopsy specimens. There existed a shortcoming in our center that Electron microscopy was performed only on 72.9% biopsy specimens. These would exert an impact on the correct diagnosis, for example, difficult to distinguish lupus membranous nephropathy from idiopathic membranous nephropathy. However, we considered the vast majority of our diagnoses consisted with the facts. For the explicit, diagnosis depends on combining clinical, laboratory data and pathologic examination rather than electron microscopic observation only.
In our study, there were 379 males and 248 females, forming the ratio of 1.53:1. About 16–50 age-brackets comprised 72.41% of the overall population. About 16–20, 21–30 and >60 years age groups showed statistically significant in the spectrum of sex. These findings were in concert with several reports by other regions of China.Citation26,Citation27 This points out that primary nephrotic syndrome occurs frequently among males of young adults. The threat posed by PNS to youth male needs our serious attention.
Our investigation showed that MN was the most common cause of PNS in the adult population of Central China, accounting for 26.63% of cases: 167/627. This finding is similar to reports from Northern ChinaCitation19 and Taiwan province of China.Citation20 However, a data from Northeastern ChinaCitation25 reported that their most common cause of PNS was MCD (49.1%), followed by MsPGN (23.5%), MN (10.6%), and IgAN (9.1%), which spectrum was significantly different from ours. The main reasons for this difference included the following: (1) demographic differences may affect this difference. The main population of Northern, Central and Northeastern China are Han nationality, however, a considerable number of ethnic minorities reside in Northeastern China. (2) Northeastern China is an area with unique geographical features and climate conditions, which is totally different from ours. (3) The diagnostic level of pathologists of different areas may have an impact on the spectrum. Some other countries including Japan,Citation10,Citation21 Spain,Citation22 ItalyCitation9 and SerbiaCitation28 also reported MN as the most common diagnosis of PNS.
MCD was found to be the second common cause of PNS, accounting for 23.60%. The frequency of MCD in primary nephrotic syndrome was very similar to that of India, with an incidence of 23.9%. In countries such as KoreaCitation23, DenmarkCitation24, MCD is the commonest cause of primary nephrotic syndrome.
IgAN is the most common glomerular disease worldwideCitation10,Citation23,Citation29,Citation30 and this condition also existed in China.Citation7 It is reported that there were ∼10–20% of IgAN presented clinically with nephrotic syndrome. In our study, it was the third common cause of primary nephrotic syndrome, accounting for 23.39%. This is extraordinarily different from countries such as Pakistan,Citation16 IndiaCitation17 and USA,Citation13 where there is a lower frequency of IgAN underlying PNS, generally <10%. The lower relative frequency of IgAN as a cause of the nephrotic syndrome has occurred in parallel with a lower frequency in the overall incidence of IgAN in Pakistan, India,Citation2,Citation8,Citation31,Citation32 accounting for 1.76–9.13%. However, this situation did not exist in USA, where the overall incidence of IgAN was 27.3%. The non-parallel appearance was explained by different policies in screening kidney diseases. Prevalence of IgAN may appear to be higher in USA than Pakistan and India for a low threshold for the performance of renal biopsy in patients with isolated asymptomatic hematuria. Nevertheless, the exact reason need further study.
FSGS was the forth common diagnosis of PNS in our investigation, accounting for 10.05%. This relative frequency is significantly lower than countries such as Pakistan,Citation16 Brazil,Citation5 India,Citation17 USACitation13 and South Africa,Citation18 in which FSGS has been reported as the commonest pathological lesion of PNS and accounting for 22.66–36%. The cause of this distinguish is not entirely clear. Two investigations together indicated race play a key role in this difference.Citation13,Citation14 As early as 1997, Haas et al. reported racial difference in the incidences of adult PNS. They found that the fraction of nephrotic adults with FSGS was two to three times higher among black patients than white patients during both the 1976–1979 and the 1995–1997 study periods. Dragovic et al. further reported a significant different incidence of FSGS between black and Hispanic patients (33.3–79.2%) and white patients (12.5–51.5%). However, racial difference does not explain all the problems. Based on the same racial inheritance in China, the fraction of nephrotic adults with FSGS in our study (10.5%) was different from that in North China (4.1%)Citation19 as well as Taiwan province (12.9%).Citation20 Hence, genetic and environmental factors, life style, diagnostic level of pathologists and so on should also be taken into consideration as the causes of epidemiologic difference. The comparison of pathological lesions in our study with others is shown in . In conclusion, epidemiologic difference is evident in various parts of the world.
Table 4. The comparison of pathological lesions in our study with North China [19]: Taiwan province of China [20], United Stated [13], Pakistan [16], Spain [22], Korea [23], Brazil [5], and South Africa [18].
Interesting, we found the relative frequency of FSGS was increased from 5.8% during the 2009–2010 period to 14.7% during the 2011–2012 period (p < 0.005). None article in China had reported a similar variation. The exact cause of this change is uncertain, we may explain it as following: (1) the diagnostic level of pathologists and technology of renal biopsy in our department improved gradually. (2) The relative frequency of FSGS as a cause of the nephrotic syndrome was increased indeed. It is a pity that we did not investigate all the patients who have been finished the renal biopsies in our center during the same period. So, we were uncertain whether the overall incidence of FSGS in our center increased as well.
The leading pathological lesion underlying PNS of each age group was distinct. In our study, MCD was the most common pathological lesions for primary nephrotic syndrome patients aged from 16 to 30 years, followed by IgAN and MN was the most common pathological lesion for patients over 30 years. And, the percentage of MN underlying primary nephrotic syndrome increased as long as the growth of age. This finding is similar to some international reports.Citation10,Citation17,Citation22 In the latest study from India,Citation17 MCD (28.96%), MN (24%), and MN (40.74%) were the most common lesions in the age groups of 16–29, 30–59, and ≥60 years, respectively. However, our report do not perfectly match with the study of North China,Citation19 which confirmed that MCD and MN were the main causes of nephrotic syndrome among younger patients. They reported MN was the main cause of nephrotic syndrome among older patients, which is in concert with ours.
In our study, we found that complications or comorbidities of primary nephrotic syndrome have something to do with pathological lesions. Such as, PNS combining with acute kidney injury was most frequently caused by pathological lesion of MCD, this conclusion had been demonstrated by many other authors.Citation33,Citation34 Although the precise mechanism of primary renal failure had not well understood, it might be related to reduction in ultrafiltration coefficient of the glomeruli.Citation33 IgA nephropathy had the highest incidence rate of hematuresis in our investigation. IgAN is the main cause of glomerular hematuria, the mechanism of this appearance is slowly being elucidated. It may related to disimmunity of mucosa. PNS combining with renal hypertension was most frequently happened by pathological lesion of MN. This phenomenon may related to one of the characteristics of MN underlying PNS that it often happened among elder people. The confirmation of pathological lesion offers objective fact for anticipating complications or comorbidities and formulating specific therapy.
MCD was the dominating pathological lesions underlying IgAN with primary nephrotic syndrome in our study. This is different from the previous conclusion which suggested that IgAN with primary nephrotic syndrome was a signal of bad prognosis. Our finding is in concert with the results by Lie et al.Citation35 They have found that the group of slight pathological changes of IgAN with primary nephrotic syndrome had heavier proteinuria than severe group. We may explain this manifestation as follows: immunoglobulin A is not the pathogenic factors among slight pathological changes group but the pathogenic factors are the slight pathological changes themselves. Whereas among severe pathological changes group, immunoglobulin A is the pathogenic factors. But the exact cause will still need further study.
In conclusion, PNS occurs frequently among males of young adults. MN, MCD, IgAN, FSGS are the main causes of primary nephrotic syndrome in Central China. MCD is the dominating pathological lesions underlying IgAN with primary nephrotic syndrome. The complications or comorbidities of primary nephrotic syndrome have something to do with pathological patterns. And the spectrum of pathological lesions underlying primary nephrotic syndrome are influenced by region, race, genetic and environmental factors, life style, diagnostic level of pathologists and so on.
Declaration of interest
The authors report no conflicts of interest.
Acknowledgements
We are very grateful to Xuejing Zhu for her assistance in collecting pathological data of the patients.
References
- Iversen P, Brun C. Aspiration biopsy of the kidney. 1951. J Am Soc Nephrol. 1997;8(11):1778–1787; discussion 1778–1786
- Balakrishnan N, John GT, Korula A, et al. Spectrum of biopsy proven renal disease and changing trends at a tropical tertiary care centre 1990–2001. Indian J Nephrol. 2003;13(1):29–31
- Narasimhan B, Chacko B, John GT, et al. Characterization of kidney lesions in Indian adults: towards a renal biopsy registry. J Nephrol. 2006;19(2):205–210
- Rychlík I, Jancová E, Tesar V, et al. The Czech registry of renal biopsies. Occurrence of renal diseases in the years 1994–2000. Nephrol Dial Transplant. 2004;19(12):3040–3049
- Polito MG, de Moura LA, Kirsztajn GM. An overview on frequency of renal biopsy diagnosis in Brazil: clinical and pathological patterns based on 9,617 native kidney biopsies. Nephrol Dial Transplant. 2010;25(2):490–496
- Covic A, Schiller A, Volovat C, et al. Epidemiology of renal disease in Romania: a 10 year review of two regional renal biopsy databases. Nephrol Dial Transplant. 2006;21(2):419–424
- Li L, Liu Z. Epidemiologic data of renal diseases from a single unit in China: analysis based on 13,519 renal biopsies. Kidney Int. 2004;66(3):920–923
- Das U, Dakshinamurty KV, Prayaga A. Pattern of biopsy-proven renal disease in a single center of south India: 19 years experience. Indian J Nephrol. 2011;21(4):250–257
- Gesualdo L, Di Palma AM, Morrone LF, et al. The Italian experience of the national registry of renal biopsies. Kidney Int. 2004;66(3):890–894
- Sugiyama H, Yokoyama H, Sato H, et al. Japan Renal Biopsy Registry: the first nationwide, web-based, and prospective registry system of renal biopsies in Japan. Clin Exp Nephrol. 2011;15(4):493–503
- D’Agati VD, Kaskel FJ, Falk RJ, et al. Focal segmental glomerulosclerosis. N Engl J Med. 2011;365(25):2398–2411
- Haas M, Spargo BH, Coventry S, et al. Increasing incidence of focal-segmental glomerulosclerosis among adult nephropathies: a 20-year renal biopsy study. Am J Kidney Dis. 1995;26:740–750
- Haas M, Meehan SM, Karrison TG, et al. Changing etiologies of unexplained adult nephrotic syndrome: a comparison of renal biopsy findings from 1976–1979 and 1995–1997. Am J Kidney Dis. 1997;30(5):621–631
- Dragovic D, Rosenstock JL, Wahl SJ, et al. Increasing incidence of focal segmental glomerulosclerosis and an examination of demographic patterns. Clin Nephrol. 2005;63(1):1–7
- Swaminathan S, Leung N, Lager DJ, et al. Changing incidence of glomerular disease in Olmsted County, Minnesota: a 30-year renal biopsy study. Clin J Am Soc Nephrol. 2006;1(3):483–487
- Kazi JI, Mubarak M, Ahmed E, et al. Spectrum of glomerulonephritides in adults with nephrotic syndrome in Pakistan. Clin Exp Nephrol. 2009;13(1):38–43
- Golay V, Trivedi M, Kurien AA, et al. Spectrum of nephrotic syndrome in adults: clinicopathological study from a single center in India. Ren Fail. 2013;35(4):487–491
- van Rensburg BW, van Staden AM, Rossouw GJ, et al. The profile of adult nephrology patients admitted to the Renal Unit of the Universitas Tertiary Hospital in Bloemfontein, South Africa from 1997 to 2006. Nephrol Dial Transplant. 2010;25(3):820–824
- Fude Zhou, Haiyan Shen, Min Chen, et al. The renal histopathological spectrum of patients with nephrotic syndrome: an analysis of 1523 patients in a single Chinese centre. Nephrol Dial Transplant. 2011;26(10):3993–3997
- Hsiao KC, Lian JD, Wu SW, et al. Ten-Year Registry of Native Kidney Biopsy from a Single Center in Taichung. Acta Nephrol. 2012;26(2):68–73
- Yokoyama H, Taguchi T, Sugiyama H, et al. Membranous nephropathy in Japan: analysis of the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol. 2012;16(4):557–563
- Rivera F, Lopez-Gomez JM, Perez-Garcia R, et al. Clinicopathologic correlations of renal pathology in Spain. Kidney Int. 2004;66(3):898–904
- Chang JH, Kim DK, Kim HW, et al. Changing prevalence of glomerular diseases in Korean adults: a review of 20 years of experience. Nephrol Dial Transplant. 2009;24(8):2406–2410
- Heaf J, Lokkegaard H, Larsen S, et al. The epidemiology and prognosis of glomerulonephritis in Denmark 1985–1997. Nephrol Dial Transplant. 1999;14(8):1889–1897
- Wu YQ, Wang Z, Xu HF, et al. Frequency of primary glomerular disease in northeastern China. Braz J Med Biol Res. 2011;44(8):810–813
- Shang Y, Yin A. Analysis on clinical pathological data of 5 000 cases undergoing renal biopsy in a hospital in Xi’an. Chin J Prev Contr Chron Dis. 2011;19(3):289–291
- Han Du, Feng Hu, Li Du, et al. A summary on the pathological data from 480 cases of renal biopsy. Pract J Med Pharm. 2010;27(5):390–392
- Naumovic R, Pavlovic S, Stojkovic D, et al. Renal biopsy registry from a single centre in Serbia: 20 years of experience. Nephrol Dial Transplant. 2009;24(3):877–885
- Cattran DC, Coppo R, Cook HT, et al. The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int. 2009;76(5):534–545
- Werner T, Brodersen HP, Janssen U. Analysis of the spectrum of nephropathies over 24 years in a West German center based on native kidney biopsies. Med Klin (Munich). 2009;104(10):753–759
- Golay V, Trivedi M, Abraham A, et al. The spectrum of glomerular diseases in a single center: a clinicopathological correlation. Indian J Nephrol. 2013;23(3):168–175
- Mubarak M, Kazi JI, Naqvi R, et al. Pattern of renal diseases observed in native renal biopsies in adults in a single centre in Pakistan. Nephrology (Carlton). 2011;16(1):87–92
- Smith JD, Hayslett JP. Reversible renal failure in the nephrotic syndrome. Am J Kidney Dis. 1992;19(3):201–213
- Larpparisuth N, Chanchairujira T, Chawanasuntorapoj R, et al. Acute kidney injury in primary nephrotic syndrome: report of nine cases in Siriraj Hospital. J Med Assoc Thai. 2011;94:125–133
- Lie C, Chen X, Xie Y, et al. Clinical and pathological analysis of IgA nephropathy patients with nephrotic syndrome. Chin J Integr Trad West Nephrol. 2008;9(4):321–324