Abstract
Upper limb gangrene is uncommon compared to lower limb gangrene. But digital gangrene is seen occasionally in patients on maintenance hemodialysis. Of the various causes described, atherosclerosis, diabetic vascular disease, following AV fistula surgery were few of the causes. Herein, we report a case of development of early digital gangrene following AV fistula in a patient on maintenance hemodialysis.
Introduction
Digital gangrene is one of the potentially serious complications in patients on maintenance hemodialysis with permanent vascular access. Various vascular interventions are available for the salvage of the hand. In certain situations even the vascular interventions might not be useful wherein need for digital amputation arises.
We report one such case with bilateral upper limb digital gangrene in a patient on maintenance hemodialysis.
Case details
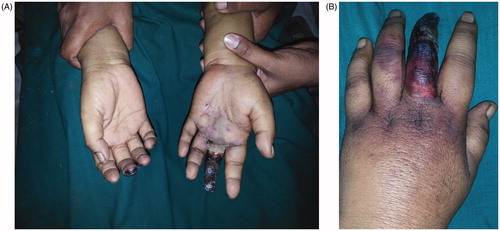
A 70-year-old woman, known diabetic, hypertensive, with chronic kidney disease stage 5 had history of coronary artery disease and moderate LV dysfunction underwent left brachiocephalic fistula. After the adequate maturation time, she was initiated on maintenance hemodialysis. One month after initiation, she developed paresthesia and bluish black discoloration in the tips of right and left middle () fingers. There was progressive increase in the gangrene in left finger. On examination, vitals were stable. There was edema of left upper limb in the distal forearm and palm. There was a clear demarcation line near the base of proximal phalanges. Bilateral radial pulses were equal and well felt. X ray of both upper limbs revealed calcification of radial and ulnar arteries along with digital arterial ( and ) calcification. Doppler of arterial system was normal. Serum calcium was 9.1 mg/dL, phosphorus was 3.8 mg/dL and iPTH was 167 pg/mL. The absence of involvement of major vessels, the diffuse medial artery calcification and the bilateral presentation deterred from performing an interventional vascular procedure. She was planned for digital amputation but could not be done as she succumbed to dialysis related complication.
Discussion
One of the grave complications of AVF is digital hand ischemia syndrome (DHIS).Though DHIS is common, digital gangrene is rare. Significant digital extremity ischemia was reportedCitation1 5–10% of all brachial access surgeries. Though definitive risk factors were not identified, the possible predisposing conditions include ESRD, diabetes mellitus, atherosclerosis, diffuse vascular disease, female gender, age >60 years, upper arm than the lower arm, use of grafts and multiple surgeries in the limb.
Pathophysiological mechanisms proposed for the development of DHIS include:
Pathological steal: physiological steal occurs in 80% after securing AVF, i.e. drop in the distal blood pressure along with formation of collaterals and venous dilatation. Failure of the compensatory mechanisms in the distal circulation due to proximal artery disease and reduced collaterals leads to pathological steal and development of DHIS
Micro emboli or fat or debris concluding the arterial inflow, which is more common in patients undergoing dialysis than in Patients not on dialysis thus suggesting the use if per filled dialyzers than the dry dialyzers.
Enhanced atherosclerosis due to plasma homocysteine, TGF beta and lipoprotein A.
Arterialization of venous system causing high venous pressure.
Increase in vessel elasticity due to increase in intimal mad medial thickness caused by vascular calcification.
In our case, digital gangrene was bilateral, left upper limb more severe than the right upper limb. The probable cause may be the diffuse atheromatous disease affecting the small vessels along with superimposed ischemia due to pathological steal in the left upper limb
Bilateral digital gangrene was reported by Yeager et al. in14 of 23 patients, primarily attributing to distal atherosclerosis rather than the hemodynamic alterations due to vascular access itself.Citation2
This case reiterates the need for a thorough history and examination in all the cases and evaluation in the form of arteriography in certain cases. According to NKF-DOQI guidelines for vascular access placement, history of diabetes mellitus, surgery in the arm/chest/neck, previous catheter placement, and presence of severe congestive heart failure, heart disease, prosthetic valves, and anticoagulant therapy should be noted. In addition a check for the patency of arterial system (Allens test), adequacy of the arterial system and the pressures in both the arms should be done before the placement of vascular access.
The points of interest in this case are two-fold:
Bilateral digital gangrene is not unusual in patients on maintenance hemodialysis.
Bilateral digital gangrene may be due to diffuse vascular disease rather than due to vascular access alone.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Malik J, Tuka V, Kasalova Z, et al. Understanding the dialysis access steal syndrome. A review of etiology es, diagnosis, prevention and treatment strategies. J Vasc Access. 2008;9:155–156
- Richard A, Gregory L, Edwards JM, et al. Relationship of hemodialysis access to finger gangrene in patients with endstage renal disease. J Vasc Surg. 2002;36:245–249