Abstract
Previous reports of percutaneous coronary intervention versus coronary artery bypass graft outcomes in coronary artery disease patients with chronic kidney disease (CKD) were inconsistent. We evaluated the optimal revascularization strategy for CKD patients. We searched Pub Med, EMBASE, and the Cochrane Central Register of Controlled Trials and scanned the references of relevant articles and reviews. All studies that compared relevant clinical outcomes between percutaneous coronary intervention and coronary artery bypass graft in CKD patients were selected. We defined short-term and long-term all-cause mortality as primary outcome, and long-term incidences of myocardial infarction and revascularization as secondary outcomes. A total of 2235 citations were retrieved, and 31 studies involving 99,054 patients, with 55,383 receiving percutaneous coronary intervention and 43,671 receiving coronary artery bypass graft, were included. In subgroup analyses of dialysis patients receiving percutaneous coronary intervention with stents versus coronary artery bypass graft, CKD patients with multivessel coronary disease, and CKD patients receiving drug-eluting stent versus coronary artery bypass graft, the pooled outcomes revealed that percutaneous coronary intervention possessed lower short-term mortality, but higher late revascularization risk. No significant differences in long-term mortality were observed between the two strategies in these subgroup analyses. In conclusion, in some specific clinical circumstances, CKD patients receiving percutaneous coronary intervention possessed lower short-term all-cause mortality, but higher long-term revascularization risk, than coronary artery bypass graft; long-term all-cause mortality was not different between the two strategies.
Introduction
Ischemic heart disease is the leading contributor to the global burden of disease.Citation1 Chronic kidney disease (CKD) is considered to be a high-risk factor for coronary artery disease (CAD).Citation2–4 Approximately, 40–50% patients with severe CKD simultaneously have CAD,Citation5 some of whom have multivessel coronary disease,Citation6–8 dialysis dependence,Citation7,Citation9,Citation10 or other complicated clinical circumstances. These patients have a worse prognosis than non-CKD patients with CAD,Citation2,Citation3,Citation6–9,Citation11,Citation12 but finding the optimal treatment is a crucial clinical challenge.
Coronary artery bypass graft (CABG) and percutaneous coronary intervention (PCI) are both candidate revascularization strategies for patients with CAD. Both techniques have been improved in the last two decades: CABG has been modified from an on-pump to an off-pump surgery, and PCI has changed from balloon angioplasty to bare-metal stent (BMS) and, later, to drug-eluting stent (DES) implantation. Simultaneously, the debate on which strategy is optimal continues.
A number of randomized controlled trials (RCTs) have compared the efficiencies and benefits of CABG and PCI, but excluded CKD patients or did not reported relevant details.Citation13–16 A few trials observed and compared the results in CKD patients;Citation6–9,Citation11,Citation17–21 however, the conclusions were undefined, particularly in some specific circumstances. Therefore, we conducted a meta-analysis, focusing on the different revascularization strategies in CAD patients with CKD, to evaluate which is the optimal choice for these specific populations.
Methods
We considered all types of previous studies that compared the clinical outcomes between PCI and CABG in CAD patients with CKD. We searched Pub Med, EMBASE (both up to 1st week of February 2014), and the Cochrane Central Register of Controlled Trials (up to January 2014), using the following words as MeSH or text words in a combined model: (“chronic kidney disease” OR “chronic renal failure” OR “chronic renal dysfunction” OR “chronic renal insufficient”) AND (“percutaneous coronary intervention” OR “percutaneous transluminal coronary angioplasty” OR “coronary artery bypass”). No language or date restriction was placed on the literature search. Additionally, we scanned the references of relevant articles and reviews.
Study selection and quality assessment
All citations were assessed for eligibility using the following criteria: (1) all types of studies were considered; (2) patients with CAD and CKD received PCI (balloon angioplasty or stent implantation) or CABG (on-pump or off-pump; arterial graft or venous graft); (3) CKD was defined as the estimated glomerular filtration rate (eGFR)<60 mL/min/1.73 m2 according to the KDIGO CKD guidelines;Citation4 and CKD patients with or without dialysis were considered. Studies were excluded for the following reasons: (1) a prior renal transplant had been performed; (2) samples included fewer than 20 patients in total, or less than 10 in either group; (3) no relevant answers regarding our research concerns were provided.
We assessed the methodological quality of the RCTs using the modified Jadad scale. The assessments involved a thorough process of randomization, concealment of allocation, and details of dropouts and withdrawals. The quality assessment of non-RCTs used was the Newcastle-Ottawa scale. The assessed items included: selections (representativeness and definition of cases), comparability (basis of analysis), exposures (ascertainment, detailed description of the methods), and outcomes (assessment, adequate and integral follow-up).
Data extraction
Data were independently extracted by two reviewers, and discrepancies were resolved by a third reviewer. We extracted the following data: type of study, interventions, sample size, gender (male), age, recruited year, follow-up time, duration of dialysis, and short-term and/or long-term outcomes, if available.
Overall analyses and subgroups analyses
All of the included studies compared the clinical outcomes between PCI and CABG in patients with CAD and CKD.
We defined short-term and long-term all-cause mortality as the primary outcome, and long-term incidences of myocardial infarction (MI) and revascularization as secondary outcomes. Some studies combined these outcomes as composite endpoints, but we analyzed them separately. The short-term outcomes were recorded within 30 days after revascularization procedures or within the in-hospital durations. The long-term events were followed-up for at least 1 year.
We performed some subgroups analyses: (1) Dialysis-dependent patients. The CKD patients receiving regular dialysis, hemodialysis, or peritoneal dialysis, at least 1 month before PCI or CABG, were analyzed. We also analyzed the subgroup outcomes of PCI with stent versus CABG in this subgroup. (2) Multivessel coronary disease patients. We performed pool analyses specifically for the studies that enrolled CKD patients with 2 or 3 diseased coronary arteries. (3) DES versus CABG. We analyzed the trials that compared the clinical outcomes of PCI with DES versus CABG in CKD patients.
Statistical analysis
We used the Stata software version 12.0 (StataCorp, College Station, TX) for the analyses. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to compare the outcomes between PCI and CABG. The statistical heterogeneity was quantified by the χ2 test with p value, and the I2 statistic. The p value for significance was set at 0.10 for the heterogeneity test. However, the non-significance of heterogeneity does not guarantee good consistency between studies. Therefore, we applied a random effect model (DerSimonian-Laird method). All other p values for significance were set at 0.05, and were 2-tailed.
This meta-analysis was conducted and reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)Citation22 and MOOSE (Meta-analysis of Observational Studies in Epidemiology) statements.Citation23
Results
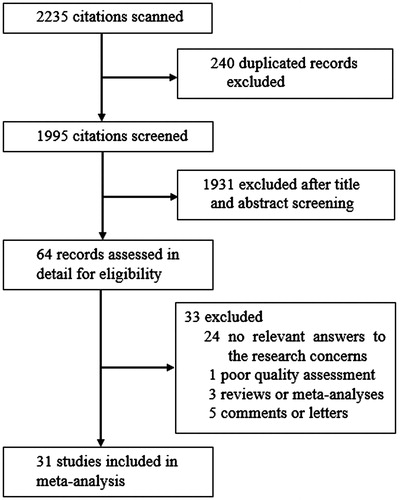
In total, 2235 citations were screened and assessed. After removing duplicates, and screening titles and abstracts, 64 records were assessed in detail. Eight records were excluded as reviews, comments, or letters. We excluded another 24 records for having no relevant answers to our research concerns. We excluded 1 study after full-text review, because we considered it to be of poor quality due to its small sample size (N = 17) and considerably high short-term mortality. Finally, 31 studies with accessed full texts were included in the meta-analysis ().Citation6–11,Citation17–21,Citation24–43
We pooled 99,054 patients in all, of whom 55,383 were treated with PCI, versus 43,671 who were treated with CABG. The patients were recruited from 1977 to 2009. The detailed characteristics and clinical outcomes are shown in and .
Table 1. Characteristics of the studies included in the meta-analysis.
Table 2. Clinical outcomes of the studies included in the meta-analysis.
Overall analyses
Nineteen studies reported the short-term all-cause mortality. The heterogeneity among the studies was considerably high (I2 = 69.9%, p < 0.001). The pooled findings suggested that PCI possessed lower short-term mortality than CABG (OR = 0.51; 95% CI 0.42 to 0.62. All results presented as PCI compared with CABG).
In the 29 studies from which the available data for long-term all-cause mortality were extracted, the heterogeneity was notable (I2 = 76.5%, p < 0.001). The PCI group showed higher long-term all-cause mortality than CABG (OR = 1.12; 95% CI 1.01 to 1.24).
Data for long-term MI events were available from 16 studies, and the heterogeneity was notable (I2 = 73.8%, p < 0.001). The overall outcome revealed that PCI led to higher long-term MI risk than CABG (OR = 1.77; 95% CI 1.44 to 2.17).
There were 18 studies with notable heterogeneity (I2 = 73.7%, p < 0.001) in the pooled analysis of long-term repeat revascularization. The PCI group had a higher revascularization risk compared with the CABG group (OR = 4.87; 95% CI 3.53 to 6.74).
All of the overall analyses showed considerable heterogeneity; therefore, we performed the following subgroup analyses.
Subgroup analyses: dialysis-dependent patients
In total, 23 studies observed the dialysis-dependent patients.Citation7,Citation9,Citation10,Citation17–19,Citation21,Citation24,Citation27,Citation29,Citation30,Citation32–43
Short-term all-cause mortality
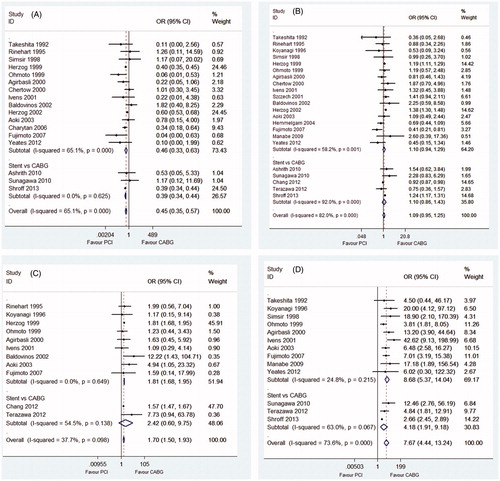
In the analysis of short-term all-cause mortality in dialysis-dependent patients, the heterogeneity was notable (I2 = 65.1%, p < 0.001). The pooled outcome showed that the risk of short-term all-cause mortality after PCI was significantly lower compared with CABG in dialysis patients (OR = 0.45; 95% CI 0.35 to 0.57). However, for the subgroup of “Stent versus CABG” in dialysis patients, three pooled studies showed low heterogeneity (I2 = 0.00%, p = 0.625). The outcome showed an advantage for the PCI group in lower short-term all-cause mortality (OR = 0.39; 95% CI 0.34 to 0.44) ().
Figure 2. (A) Short-term all-cause mortality in dependent dialysis patients. (B) Long-term all-cause mortality in dependent dialysis patients. (C) Long-term incidence of myocardial infarction in dependent dialysis patients. (D) Long-term incidence of revascularization in dependent dialysis patients.
Long-term all-cause mortality
We extracted the available data for long-term all-cause mortality from 22 citations for this subgroup analysis. The heterogeneity was considerable (I2 = 82.0%, p < 0.001). The overall outcome did not show a significant difference between the two treatments (OR = 1.09; 95% CI 0.95 to 1.25). In the subgroup of “Stent versus CABG”, the pooled outcome of 5 studies revealed a similar trend (OR = 1.10; 95% CI 0.86 to 1.43) ().
Secondary outcomes
In the subgroup analysis of long-term MI events in dialysis patients, the heterogeneity was moderate among 11 studies (I2 = 37.7%, p = 0.098). Dialysis patients in the PCI group had higher long-term MI risk than those in the CABG group (OR = 1.70; 95% CI 1.50 to 1.93) ().
In the 13 studies that provided long-term revascularization data in dialysis-dependent patients, 11 trials showed the superiority of CABG in causing fewer late revascularization events. After the pooled analysis, the overall outcome suggested that the higher late revascularization risk after PCI was considerable (OR = 7.67; 95% CI 4.44 to 13.24). With stents, the subgroup outcome of 3 studies also showed that PCI possessed higher long-term revascularization risk (OR = 4.18; 95% CI 1.91 to 9.18) ().
Subgroup analyses: multivessel coronary disease patients
Seven studies specifically compared the outcomes of the two strategies in multivessel CAD patients with CKD.Citation6–8,Citation18,Citation20,Citation25,Citation28
Only one trialCitation18 provided data for short-term all-cause mortality (OR = 0.48; 95% CI 0.22 to 1.05).
Long-term all-cause mortality
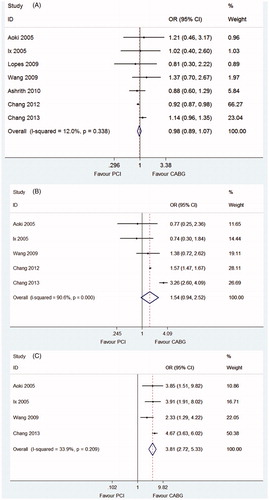
For this subgroup analysis, the heterogeneity of all seven studies was low (I2 = 12.0%, p = 0.338). No significant difference between the two groups was shown after pooled analysis (OR = 0.98; 95% CI 0.89 to 1.07) ().
Figure 3. (A) Long-term all-cause mortality in CKD patients with multivessel coronary disease. (B) Long-term incidence of myocardial infarction in CKD patients with multivessel coronary disease. (C) Long-term incidence of revascularization in CKD patients with multivessel coronary disease. CKD: chronic kidney disease.
Secondary outcomes
There was a considerably high level of heterogeneity among the five studies that provided the relevant data for long-term MI events in CKD patients with multivessel coronary disease (I2 = 90.6%, p < 0.001). The pooled outcome did not reveal significant difference in long-term MI incidence between PCI and CABG (OR = 1.54; 95% CI 0.94 to 2.52) ().
Four trials were pooled in the analysis of long-term revascularization in CKD patients with multivessel coronary disease, all of which showed the benefits of CABG over PCI, with mild heterogeneity (I2 = 33.9%, p = 0.209). After pooled analysis, PCI still showed obviously higher long-term revascularization risk than CABG (OR = 3.81; 95% CI 2.72 to 5.33) ().
Subgroup analyses: DES versus CABG
Six studies compared the outcomes between DES and CABG.Citation9,Citation10,Citation17,Citation18,Citation25,Citation26 Two trials used both DES and BMS, but they specifically reported the details of DES.Citation10,Citation26
Short-term all-cause mortality
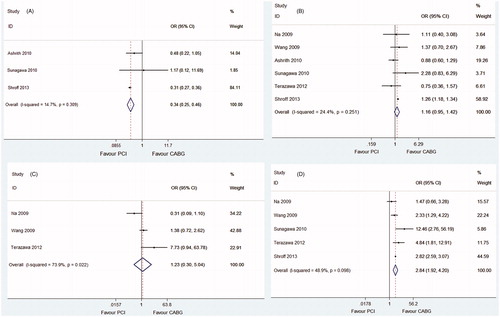
We pooled three studies that reported the available data for short-term all-cause mortality for this subgroup analysis. The heterogeneity was low (I2 = 14.7%, p = 0.309). The DES group showed a remarkable benefit in short-term mortality over CABG (OR = 0.34; 95% CI 0.25 to 0.46) ().
Figure 4. (A) Short-term all-cause mortality in CKD patients comparing PCI with DES versus CABG. (B) Long-term all-cause mortality in CKD patients comparing PCI with DES versus CABG. (C) Long-term incidence of myocardial infarction in CKD patients comparing PCI with DES versus CABG. (D) Long-term incidence of revascularization in CKD patients comparing PCI with DES versus CABG. CKD: chronic kidney disease; PCI: percutaneous coronary intervention; DES: drug-eluting stent; CABG: coronary artery bypass graft.
Long-term all-cause mortality
For long-term all-cause mortality analysis in this subgroup, the heterogeneity of six studies was mild (I2 = 24.4%, p = 0.251). There was also no significant difference in long-term all-cause mortality between patients who received PCI compared with CABG (OR = 1.16; 95% CI 0.95 to 1.42) ().
Secondary outcomes
Three studies provided the data for long-term MI for this subgroup analysis, and the pooled outcome showed no difference between the two procedures (OR = 1.23; 95% CI 0.30 to 5.04) ().
Five studies were pooled in the analysis of long-term revascularization events between DES and CABG in CKD patients. The heterogeneity was high (I2 = 48.9%, p = 0.098). The DES group had a notably higher incidence of late revascularization compared with CABG (OR = 2.84, 95% CI 1.92 to 4.20) ().
Discussion
In our meta-analysis, which incorporated 31 studies, we pooled the available data to compare the clinical outcomes between PCI and CABG using all-cause mortality, and incidences of long-term MI and revascularization. In the overall analyses, PCI was superior for short-term all-cause mortality in CKD patients, and CABG showed superiority for long-term benefits. All the overall analyses had high heterogeneity, thus, the pooled outcomes had little value. We considered whether different types of intervention procedures and varied clinical circumstances among the studies contributed to the high heterogeneity. Hence, we performed some subgroup analyses, with relevant clinical topics, to explore the sources of this high heterogeneity. In the subgroup of dialysis-dependent patients receiving PCI with stents versus CABG, the subgroups of CKD patients with multivessel coronary disease and CKD patients receiving PCI with DES versus CABG, the pooled studies demonstrated good consistency in some analyses. From the pooled outcomes, PCI still showed lower short-term all-cause mortality, but higher late revascularization risk, compared with CABG. However, long-term all-cause mortality was not different between CKD patients who received PCI and CABG.
From the short-term outcome, the superiority of PCI for lower all-cause mortality was observed. This improvement might be mainly ascribed to the high non-cardiac mortality after CABG, especially for CKD patients with complicated clinical circumstances. Potentially fatal non-cardiac complications, such as severe infection, stroke, major bleeding, and respiratory dysfunction,Citation37,Citation38,Citation44 were more common after CABG than after PCI. All these adverse effects put the CKD patients at higher risk after CABG, although the postoperative complications were reduced by the newer off-pump procedure.Citation45 Contrast-induced acute kidney injury (AKI)Citation46 and the bleeding risk associated with multiple anticoagulation and antiplatelet drugs must be considered for PCI. However, due to the lower impact of PCI on other organs or systems, the non-cardiac risk was much lower with PCI than with CABG.
For the specific subgroup analyses, similar to previous reviews,Citation12,Citation47 our analyses did not reveal an advantage of CABG in lowering long-term all-cause mortality in CKD patients. Several possible reasons explain these findings. (1) In those CKD patients included in these studies, many coexisting factors, such as diabetes mellitus, elderly age, smoking, and peripheral artery disease, could potentially interfere with the final outcomes. (2) In many trials, the risk of death after the revascularization procedure was not proportional during follow-up, and this disproportion was obviously different between PCI and CABG. As shown in some trials, the relative risk of death declined over time, with a higher risk of perioperative death but a greater long-term reduction in death after CABG than after PCI.Citation11,Citation18 (3) The advantage of CABG over PCI was previously demonstrated in patients with coronary lesions with complex anatomical characteristics, especially left main and 3-vessel coronary disease with moderate and high SYNTAX scores.Citation16 However, in our multivessel coronary disease subgroup, the trials combined the results of both 2-vessel and 3-vessel diseases, and this combination likely minimized the benefits of CABG in 3-vessel disease patients.Citation18,Citation25 Therefore, 3-vessel disease CKD patients should be analyzed as an individual group. Additionally, whether the SYNTAX score or other anatomical scores are helpful in CKD patients with complex coronary lesions remains unclear.
Although CABG still revealed some benefits during long-term follow-up, especially a markedly lower late repeated revascularization risk, owing to insufficient evidence regarding the benefits on mortality after CABG, we agree with the cautious recommendation of the ACCF/AHA guidelines that CABG might be a reasonable choice for some selected end-stage renal disease patients despite the increased risk of postoperative morbidity and mortality.Citation48
Several limitations of the current meta-analysis should be considered. (1) Because no specialized RCTs have focused on this topic to date, we only extracted data from retrospective and prospective studies, cross-sectional studies, and subgroup data from RCTs that compared the clinical outcomes between PCI and CABG. This approach is the major limitation of this meta-analysis. (2) The discrepant clinical circumstances among the included trials could not be ruled out. To control the influence of the confounding factors, adjusted data should be analyzed if possible. However, most of the included studies only reported the non-adjusted data, or data adjusted by different variables. Lacking the primary data, we could not calculate the adjusted outcomes for pooled analyses to preclude the influence of confounding factors. (3) Two of the citations were generated from the ARTS trial,Citation8,Citation20 and another two trials used the database of the United States Renal Data System;Citation7,Citation10 although the research concerns, samples, and outcomes were different, some data may overlap. (4) We conducted some subgroup analyses that showed low heterogeneity; however, the heterogeneity tests still demonstrated poor consistencies among the pooled studies in some analyses. Hence, a number of rigorous RCTs will be needed to focus on this topic in the future.
In conclusion, in some specific clinical circumstances, CKD patients receiving PCI had lower short-term all-cause mortality, but higher long-term revascularization risk, than CKD patients undergoing CABG. However, long-term all-cause mortality was not different between the two strategies.
Declaration of interest
No relevant financial interests or any supports exist.
References
- Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369(5):448–457
- Tonelli M, Muntner P, Lloyd A, et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: A population-level cohort study. Lancet. 2012;380(9844):807–814
- Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351(13):1285–1295
- KDIGO. 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease; 2013. Available at: http://www.kidney-international.org
- Kumar N, Baker CS, Chan K, et al. Cardiac survival after pre-emptive coronary angiography in transplant patients and those awaiting transplantation. Clin J Am Soc Nephrol. 2011;6(8):1912–1919
- Chang TI, Leong TK, Kazi DS, Lee HS, Hlatky MA, Go AS. Comparative effectiveness of coronary artery bypass grafting and percutaneous coronary intervention for multivessel coronary disease in a community-based population with chronic kidney disease. Am Heart J. 2013;165(5):800–808.e2
- Chang TI, Shilane D, Kazi DS, Montez-Rath ME, Hlatky MA, Winkelmayer WC. Multivessel coronary artery bypass grafting versus percutaneous coronary intervention in ESRD. J Am Soc Nephrol. 2012;23(12):2042–2049
- Aoki J, Ong AT, Hoye A, et al. Five year clinical effect of coronary stenting and coronary artery bypass grafting in renal insufficient patients with multivessel coronary artery disease: Insights from ARTS trial. Eur Heart J. 2005;26(15):1488–1493
- Terazawa S, Tajima K, Takami Y, et al. Early and late outcomes of coronary artery bypass surgery versus percutaneous coronary intervention with drug-eluting stents for dialysis patients. J Card Surg. 2012;27(3):281–287
- Shroff GR, Solid CA, Herzog CA. Long-term survival and repeat coronary revascularization in dialysis patients after surgical and percutaneous coronary revascularization with drug-eluting and bare metal stents in the United States. Circulation. 2013;127(18):1861–1869
- Charytan DM, Li S, Liu J, Herzog CA. Risks of death and end-stage renal disease after surgical compared with percutaneous coronary revascularization in elderly patients with chronic kidney disease. Circulation. 2012;126(11 Suppl 1):S164–S169
- Nevis IF, Mathew A, Novick RJ, et al. Optimal method of coronary revascularization in patients receiving dialysis: Systematic review. Clin J Am Soc Nephrol. 2009;4(2):369–378
- Kapur A, Hall RJ, Malik IS, et al. Randomized comparison of percutaneous coronary intervention with coronary artery bypass grafting in diabetic patients. 1-year results of the CARDia (Coronary Artery Revascularization in Diabetes) trial. J Am Coll Cardiol. 2010;55(5):432–440
- Booth J, Clayton T, Pepper J, et al. Randomized, controlled trial of coronary artery bypass surgery versus percutaneous coronary intervention in patients with multivessel coronary artery disease: Six-year follow-up from the Stent or Surgery Trial (SoS). Circulation. 2008;118(4):381–388
- Henderson RA, Pocock SJ, Sharp SJ, et al. Long-term results of RITA-1 trial: Clinical and cost comparisons of coronary angioplasty and coronary-artery bypass grafting. Lancet. 1998;352(9138):1419–1425
- Mohr FW, Morice M-C, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381(9867):629–638
- Sunagawa G, Komiya T, Tamura N, Sakaguchi G, Kobayashi T, Murashita T. Coronary artery bypass surgery is superior to percutaneous coronary intervention with drug-eluting stents for patients with chronic renal failure on hemodialysis. Ann Thorac Surg. 2010;89(6):1896–1900; discussion 1900
- Ashrith G, Lee VV, Elayda MA, Reul RM, Wilson JM. Short- and long-term outcomes of coronary artery bypass grafting or drug-eluting stent implantation for multivessel coronary artery disease in patients with chronic kidney disease. Am J Cardiol. 2010;106(3):348–353
- Charytan D, Mauri L, Agarwal A, Servoss S, Scirica B, Kuntz RE. The use of invasive cardiac procedures after acute myocardial infarction in long-term dialysis patients. Am Heart J. 2006;152(3):558–564
- Ix JH, Mercado N, Shlipak MG, et al. Association of chronic kidney disease with clinical outcomes after coronary revascularization: The Arterial Revascularization Therapies Study (ARTS). Am Heart J. 2005;149(3):512–519
- Hemmelgarn BR, Southern D, Culleton BF, et al. Survival after coronary revascularization among patients with kidney disease. Circulation. 2004;110(14):1890–1895
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151(4):264–269, W264
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012
- Yeates A, Hawley C, Mundy J, Pinto N, Haluska B, Shah P. Treatment outcomes for ischemic heart disease in dialysis-dependent patients. Asian Cardiovasc Thorac Ann. 2012;20(3):281–291
- Wang ZJ, Zhou YJ, Liu YY, et al. Comparison of drug-eluting stents and coronary artery bypass grafting for the treatment of multivessel coronary artery disease in patients with chronic kidney disease. Circ J. 2009;73(7):1228–1234
- Na KY, Kim CW, Song YR, Chin HJ, Chae DW. The association between kidney function, coronary artery disease, and clinical outcome in patients undergoing coronary angiography. J Korean Med Sci. 2009;24 Suppl:S87–S94
- Manabe S, Shimokawa T, Fukui T, et al. Coronary artery bypass surgery versus percutaneous coronary artery intervention in patients on chronic hemodialysis: Does a drug-eluting stent have an impact on clinical outcome? J Card Surg. 2009;24(3):234–239
- Lopes NH, da Silva Paulitsch F, Pereira A, et al. Mild chronic kidney dysfunction and treatment strategies for stable coronary artery disease. J Thorac Cardiovasc Surg. 2009;137(6):1443–1449
- Fujimoto Y, Ishiwata S, Dohi T, et al. Long-term prognosis after coronary revascularization in patients with end-stage renal disease on dialysis: Comparison of percutaneous coronary intervention and coronary artery bypass grafting. J Cardiol. 2007;50(1):11–20
- Aoki J, Ikari Y, Sugimoto T, Fukuda S, Hara K. Clinical outcome of percutaneous transluminal coronary rotational atherectomy in patients with end-stage renal disease. Circ J. 2003;67(7):617–621
- Szczech LA, Best PJ, Crowley E, et al. Outcomes of patients with chronic renal insufficiency in the bypass angioplasty revascularization investigation. Circulation. 2002;105(19):2253–2258
- Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation. 2002;106(17):2207–2211
- Baldovinos GPA, Larre Borges P, Alvarez A, et al. Ischemic cadiopathy in patients undergoing chronic hemodialysis. Nefrologia. 2002;22(1):60–65
- Szczech LA, Reddan DN, Owen WF, et al. Differential survival after coronary revascularization procedures among patients with renal insufficiency. Kidney Int. 2001;60(1):292–299
- Ivens K, Gradaus F, Heering P, et al. Myocardial revascularization in patients with end-stage renal disease: Comparison of percutaneous transluminal coronary angioplasty and coronary artery bypass grafting. Int Urol Nephrol. 2001;32(4):717–723
- Chertow GM, Normand SL, Silva LR, McNeil BJ. Survival after acute myocardial infarction in patients with end-stage renal disease: Results from the cooperative cardiovascular project. Am J Kidney Dis. 2000;35(6):1044–1051
- Agirbasli M, Weintraub WS, Chang GL, et al. Outcome of coronary revascularization in patients on renal dialysis. Am J Cardiol. 2000;86(4):395–399
- Ohmoto Y, Ayabe M, Hara K, et al. Long-term outcome of percutaneous transluminal coronary angioplasty and coronary artery bypass grafting in patients with end-stage renal disease. Jpn Circ J. 1999;63(12):981–987
- Herzog CA, Ma JZ, Collins AJ. Long-term outcome of dialysis patients in the United States with coronary revascularization procedures. Kidney Int. 1999;56(1):324–332
- Simsir SA, Kohlman-Trigoboff D, Flood R, Lindsay J, Smith BM. A comparison of coronary artery bypass grafting and percutaneous transluminal coronary angioplasty in patients on hemodialysis. Cardiovasc Surg. 1998;6(5):500–505
- Koyanagi T, Nishida H, Kitamura M, et al. Comparison of clinical outcomes of coronary artery bypass grafting and percutaneous transluminal coronary angioplasty in renal dialysis patients. Ann Thorac Surg. 1996;61(6):1793–1796
- Rinehart AL, Herzog CA, Collins AJ, Flack JM, Ma JZ, Opsahl JA. A comparison of coronary angioplasty and coronary artery bypass grafting outcomes in chronic dialysis patients. Am J Kidney Dis. 1995;25(2):281–290
- Takeshita S, Yamaguchi T, Isshiki T, et al. Percutaneous transluminal coronary angioplasty and coronary bypass grafting for refractory angina in chronic dialysis patients. J Cardiol. 1992;22(2-3):383–390
- Liu JY, Birkmeyer NJO, Sanders JH, et al. Risks of morbidity and mortality in dialysis patients undergoing coronary artery bypass surgery. Circulation. 2000;102(24):2973–2977
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med. 2012;366(16):1489–1497
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44–e122
- Hlatky MA, Boothroyd DB, Bravata DM, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: A collaborative analysis of individual patient data from ten randomised trials. Lancet. 2009;373(9670):1190–1197
- Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58(24):e123–e210