ABSTRACT
Background: Research focused on identifying vulnerable populations and revealing specific risk factors for barriers along the pathway from ESRD to kidney transplantation has been mostly descriptive and the causes of existing disparities remain unclear. However, several socio-economic factors that are associated with the access to and the outcome of the kidney transplantation have been identified. Summary: While the presence of racial, gender, and geographic disparities is noted, we were interested mostly to describe potential socio-economic factors associated with and possibly responsible for the presence of such disparities. In this review we focused on five factors: education level, employment status, income, presence of substance addiction or abuse, and marital status. We describe the new method to quantify patients' socio-economic status and identify the group of high risk in terms of the transplant outcome, easily calculated social adaptability index, previously associated with clinical outcome in several patient populations including those with kidney transplant. At the end, based on literature analyzed we offer potential interventions that potentially can be used in order to reduce the degree of disparities. Conclusion: Based on review of literature socio-economic factors are associated with and possibly responsible for healthcare disparities. Social adaptability index allows quantifying the degree of socio-economic status and identifying the group of high risk for inferior transplant outcome.
Existing disparities in kidney transplantation
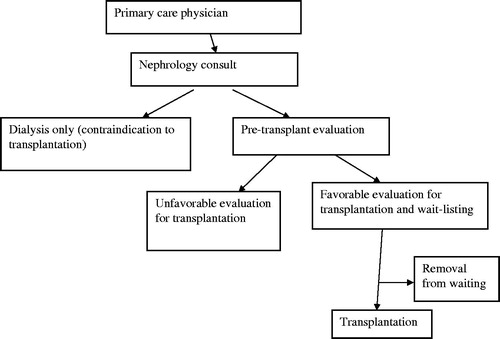
The presence of disparities in organ transplantation has been extensively reportedCitation1 and primarily involves racial, gender, and geographic disparities. The outcome of existing studies is measured as either graft or recipient survival or in terms of access to transplantation (i.e. time between ESRD onset and listing, and between listing and organ transplantation). The latter outcome is important since graft and patient survival are inversely related to time on dialysis.Citation2–4 While Blacks have lower accessCitation5 and poorer outcome of the transplantation, Whites are far more likely to receive a preemptive kidney transplant and less likely to be exposed to greater than 3 years of dialysis before transplantation.Citation6 To recognize the source of disparities it is helpful to have a clear understanding of the pathway from ESRD to transplantation, which is somewhat complex (). It seems that at every stage of the process black patients are disadvantaged.Citation5,Citation7–10 Specifically, a substantial number of ESRD patients are not presented with kidney transplantation as an alternative to dialysis by their physicians. In the population of patients considered to be appropriate for transplantation Blacks are less likely to be referred for evaluation, found acceptable candidates and placed on the waiting list, or undergo transplantation. Furthermore, patients might be declined by the transplant program after initial evaluation and those candidates that are placed on the list may be later removed or become “temporarily unavailable” because of comorbid conditions or medical events.Citation5,Citation11,Citation12 That being said, at least some of the discrepancy seems to be caused by differences in clinical characteristics between the patient groups.Citation5 On the other hand, recent study suggested that racial disparities in access to transplantation are driven by differences in the socio-economic status.Citation11 However, it does not seem that in this report the adjustment has been done for the health status of the patients. In a similar study, with adjustment done for comorbidity index, Blacks still had lower access to transplantationCitation13 and worse transplant outcome.Citation14 Aside from health status and socio-economic factors there are other potential reasons for disparities: the rate of donation might vary in different communities,Citation15 lower level of health literacyCitation16 and lesser adherence to medical regimens in BlacksCitation17 (the latter point being disputed by other authorsCitation18).
The presence of gender disparities is also debated in literature. Women seem to have less access to deceasedCitation19 and livingCitation20 donor kidney transplantation, but as in the case with racial differences, the degree to which comorbidities contribute to this association is not completely clear. In the study by Segev et al., while gender disparities have been demonstrated, age and comorbidities have been shown to be strong effect-modifying factors.Citation21
Regarding geographic disparities, Axelrod et al. suggested that patients living farther from the transplant center had reduced access to deceased donor kidney transplantation and increased risk of post-transplant death.Citation22 Other authors suggest that living in impoverished areas, rather than the distance to transplant center may be the basis for geographic disparities.Citation9 Geographic differences in perceptions of nephrologists regarding patient candidacy for kidney transplant, perceived barriers to kidney transplant, and proposed strategies to increase rates of kidney transplantCitation23 as well as differences in perceptions among rural and urban patients about aspects of transplantCitation24 may contribute to geographic disparities in transplant. On a scale of the entire country, the waiting time is dramatically different between different regions of the US, with unadjusted median wait time for deceased donor kidney being the longest in New York, California, Washington (>4 years) and shortest in Utah, Nebraska, Arkansas, Kentucky (1.4 years).Citation25
As it has been discussed above, disparities in time to transplantation and in the transplant outcome had been described in literature mostly in relation to race, gender and geographic location. While the mechanism of disparities in access to healthcare and in clinical outcome might be unclear (e.g. patient insurance status, education level, social support, availability of the organ for transplant, etc.); socio-economic characteristics probably make a significant contribution (the fact which might be underappreciated in a some of the studiesCitation26). In that context it is important to make a distinction between several terms sometimes used interchangeably but not necessarily synonymous: disparities, differences, and barriers.Citation1 The differences (e.g. differences in outcome between Black and White patients based on patient health status) refer to a broader concept than disparities, latter having a social injustice implications and mostly pointing to social disadvantage or discrimination of a particular group.Citation27 Barriers also are not equal to disparities, as the presence of barriers implies objective reasons for limited access to health care or for inferior outcome; while in case of disparities the differences are avoidable. As opposed to “differences” that may be explained by biologic as well as socio-economic factors, “disparities” are based on unequal distribution of socio-economic factors. Disparities therefore are likely to be explained by the association between socio-economic factors and access to care as well as the outcome. We will try to examine this concept in details below.
For the purpose of this review we decided to focus specifically on the role of socioeconomic factors that have been recently examined in relation to kidney transplant outcome. These characteristics are distributed unequally in the racial groupsCitation28 and they found to be associated with the clinical outcome (e.g. employment status,Citation29 health insurance type,Citation30 education level,Citation30 marital status,Citation31 substance abuseCitation32), may affect the outcome of kidney transplantation.
Association of socio-economic factors with kidney transplant outcome
Education level
Below we will discuss the association between education level with both access to transplantation and transplantation outcome (i.e. graft and recipient survival). Since education is one of a very few modifiable socio-economic factors, it makes an attractive target for intervention. Indeed, it has been demonstrated that the racial disparities in access to transplantationCitation13 and transplant outcomeCitation14 may be alleviated in patients with higher levels of education.
Access to transplantation
It has been shown that college graduates were three times as likely to be wait-listed or receive a kidney transplant when compared to patients with less than 12 yr of education.Citation33 Furthermore, we previously demonstrated an incremental increase in odds of being listed and then transplanted with increased education level.Citation13 Several potential mechanisms may explain this association. Better educated individuals may seek the transplant organ through the means that are not available to less educated patients, or they might not be aware of. Better education may be associated with improved health literacy, which improves odds of being listed.Citation34 In addition, education had modifying effect on racial differences in access to transplantation. Black patients were less likely to be wait-listed/transplanted in three less educated groups (i.e. those never completed high school, high school graduates and those with partial college education). However, the difference in likelihood and time to listing lost statistical significance in those who completed college education. Interestingly in patients who were already listed, significant racial disparity in time from listing to transplantation persisted across all levels of education.Citation13 It is possible that the listing process where human decision is involved to a large extent () is more prone to communication barriers between patients and health care professionals and to potential bias and disparities. The decision of the primary nephrologist to refer a patient to a transplant program and the decision of the transplant program to consider a particular patient as a candidate may both be biased. In contrast, a patient's position on the list is less prone to human bias and discrimination but may be more affected by biologic factors, such as comorbidity.
Transplant outcome
Education level is associated with kidney transplant outcome, and there is a trend of incremental lowering of the hazards for both graft failure and recipient mortality with advanced education level.Citation30 Similar to the access to transplantation, the degree of disparities in graft and recipient survival between African Americans and whites gradually decreased with increasing level of education.Citation14 Theoretically, higher education levels may improve health literacy, leading to a better medication adherence and potentially to a better outcome. Indeed, the confounding effect of education makes sense as it is unequally distributed in races,Citation28 and it has an association with transplant outcomeCitation30 and access to transplantation.Citation33 These alleviating effects of education could be explained in a number of ways. Poor education level might serve as a communication barrier between patients and health care professionals. Also, there is an evidence to suggest that higher educational level is associated with better compliance.Citation35
Income level
Individuals with lower income are less likely to be interested in transplantation, found medically suitable, and to complete the pre-transplant workup.Citation36 While income information is not always available for analyses, receiving benefits from the government programs (e.g. Medicaid or Medicare) has been used as an indicator for low-income status in some studies. Specifically, having private insurance is beneficial compared to Medicaid or Medicare to graft and recipient survival, even when the analysis was stratified by the racial groups.Citation30 Several potential mechanisms might contribute to this association, in particular, cost related non-compliance with medication regimen has been postulated.Citation37 Extension of Medicare immunosuppression benefits from 3 years to lifetime among kidney transplant recipients aged ≥65 years or disabled attenuated income-associated differences in long-term renal graft survival (difference in 5 year graft survival between low vs. high income groups of 5.4% almost disappeared under the new policy).Citation38 While it is tempting to explain the association between income and transplant outcome by direct association due to inability to afford care, it does not seem to be the only mechanism. Lower income was found to be a significant and independent predictor of graft survival in an analysis of 621, mostly White renal transplant recipients from United Kingdom, where patients receive free medical care. Acute rejection was significantly more frequent for patients with low income compared with the high-income group (36% vs. 27%).Citation39
There is an interaction between racial disparities and income, so that low-income may accentuate racial disparities. Patzer et al. observed in an analysis of 35,346 subjects that the degree of racial disparities differs as neighborhood poverty increases. In this study, Black patients were less likely to be wait-listed than Whites in all neighborhoods but this disparity was most striking in the poorest communities where Blacks were 57% less likely to be listed than Whites.Citation9 A similar association between poverty and disparity was described in other publications.Citation40 However, despite its strong association with outcome the income level does not fully explain the presence of racial disparities. The racial disparity in graft survival between Black and non Black patient group eligible for the lifetime benefit was still present.Citation41 Still, it seems reasonable to suggest that focusing on poor communities may be an effective way to improve fair allocation of kidney allografts.
Employment status
Employment rates after solid organ transplantation have been reported as low as 45–55%Citation42–46 driven by poor health, acute rejection episodes, and fear of loss of health insurance or disability benefits.Citation42,Citation45,Citation47 On the other hand, transplant recipients who worked prior to transplantation and have higher pre-transplant incomes and levels of education, as well as those without diabetes and receiving the kidney from the living donor are more likely to return to work.Citation42,Citation46 It has been reported that solid organ transplant recipients who return to work differ in several aspects from those who do not, including shorter periods of pre-transplant disability and unemployment (age 35–50 years), higher educational level, retention of health insurance, and a professional job.Citation43
Furthermore, post-transplant employment is associated with better transplant outcome. Specifically, working full time at the time of transplantation and at 12 months post transplantation is beneficial to graft and recipient survival. In addition, working part time by choice and not working by choice at the time of transplantation or a short time after transplantation was associated with inferior outcome compare to those working full time.Citation29 Of course, in the complex relationship between socio-economic factors and outcome the association may be explained by direct effect of employment on clinical outcome (e.g. better health insurance coverage associated with employment,Citation30 higher income and ability to pay for medicationCitation30), or by confounding effect of other factors (e.g. employment could reflect the patient's general well being). Employment may be associated with higher level of physical activity, better glycemia control,Citation48 lower prevalence of cardio-vascular diseaseCitation49 and depression.Citation50
Interestingly, working full-time at 5 years post-transplant was associated with worse outcome.Citation29 The potential explanation for this phenomenon might be the fact that transplant recipients are covered by Medicare during their first three post-transplant years; therefore, at 5 years post-transplant those not working are either on disability or use some other resources to pay for medical services. In other words, the recipients who do not work are frequently supported through government agencies, while those who chose to seek employment often lose government benefits.Citation43,Citation45 Therefore, it is possible that healthier individuals who elect to work might have a high enough income to disqualify them from government benefits, yet have insufficient resources to cover all their medical expenses.Citation47 Other explanations are possible, but are less convincing (e.g. full-time employment has been demonstrated to be associated with lower levels of self-reported medication adherenceCitation18).
Marital status
The positive impact of marital status on clinical outcome has been demonstrated.Citation51–53 In the transplant recipients being married is associated with greater odds of being transplanted and also with better outcome of transplantation itself. Specifically, compared to patients between the ages 40 and 65 who have never been married, those who have been married had higher access to renal transplantation both in terms of shorter time from ESRD onset to listing, and from listing to being transplanted.Citation54 Furthermore, being married had positive effect for the graft (but not recipient) survival. Interestingly, when males and females were analyzed separately, the same positive association between being married and graft survival was observed in male recipients, but not in females.Citation31
As with other socio-economic factors, the effect may be confounded by other variables. In particular, compared to those that have not been married, the recipients who have been married had higher percent of Whites and lower percent of Blacks, shorter duration of ESRD, lower percent of patients with prior kidney transplant but higher percent of diabetics.Citation31,Citation54 While multivariate models have been adjusted for these variables, residual confounding is still possible. Alternatively, the effect of being married on the transplant access and outcome may be mediated by lower income and inferior health insurance, reduced access to healthcare and living donors, less developed social network, depression, lower quality of life, and negative health behaviors in terms of alcohol and drug abuse. In addition married people might also benefit from somebody else monitoring their health status.
Substance abuse
Due to concern that a recipient's substance abuse might lead to accelerated graft loss many transplant programs exclude patients with active substance abuse (tobacco, alcohol or drugs). Analysis of 1,077,699 patients has demonstrated that patients with ESRD who are abusing or dependent on tobacco, alcohol, or illicit drugs are less likely to be placed on the waiting list for kidney transplant, and once on the list are less likely to be transplanted.Citation55 Indeed, substance abuse has been associated with inferior clinical outcome and with poor compliance;Citation56 in addition intravenous drug use is a risk factor for hepatitis C.Citation57 Active substance abuse has been linked to inferior transplant outcome. Specifically, it has been demonstrated that a history of recipient alcohol dependency at the time of ESRD onset has a negative effect on graft and recipient survival.Citation32 It seems reasonable that the decisions to exclude patients with substance abuse should be based on severity, type of substance abuse and assessment of compliance as well as psychological evaluation of the patient. In donors with substance abuse, only tobacco smoking, but not alcohol or drug abuse have been associated with inferior transplant outcomeCitation58 and therefore there is no evidence to support avoiding the kidneys from donors with IV drug use or alcohol dependency in transplantation.
Quantification of socio-economic status: social adaptability index (SAI)
As it has been discussed above, socially disadvantaged individuals may be prone to have inferior medical outcomes, in particular Blacks,Citation59,Citation60 women,Citation61 and residents of rural (as opposed to urban) regions.Citation62 Disparities (as opposed to broader term “differences”) in relation to the disadvantaged populations are likely to be based on socio-economic factors unequally distributed in groups based on race, gender, or geographic location. However, defining disadvantaged population based on rigid criteria of skin color, gender, or geographic location may be prone to errors lacking specificity and sensitivity. The better approach is to quantify the degree of disadvantaged status, which would be important for both clinical practice and research. Strong evidence suggests that lower socio-economic status is a health risk factor independent of genetic and many clinical indicators.Citation29–32,Citation63–67 A measure proposed an index based on employment, accommodation and living situation was proposed in the past and was only weakly associated with symptoms, quality of life, global functioning and disability.Citation68 More recently a Social Adaptability Index (SAI) has been proposed. SAI is a composite indicator based on employment, education level, income, marital status, and substance abuse. Each of these factors has been demonstrated to have strong association with clinical outcome.Citation29–32 SAI is calculated based on these factors (each graded on a scale of 0–3 as described in and contributing between 0 and 3 points to the SAI). SAI therefore ranges between 0 and 15 points. It seems to be a useful tool for clinicians and researchers to identify population at risk of inferior clinical outcome and also the disadvantaged groups prone to disparities. This index had strong and significant association with mortality in different groups of individuals, including general American population,Citation69 patients with diabetes,Citation70 those with chronic kidney disease,Citation71 dialysis patientsCitation72 and those with kidney transplant.Citation73 Specifically, SAI is associated with graft and recipient survival in renal transplant recipients. Higher SAI levels were associated with a significant reduction in risks for graft loss and recipient mortality. The mechanism of this association might be mediated by lower level of adherence, lower health literacy, possibly less developed social structure and greater degree of objective barriers to care in the recipients with lower SAI.Citation73 In addition to its association with clinical outcome the SAI predicts access to kidney transplantation (measured as time to being placed on the list and also as time to being transplanted among those who were listed).Citation74 Each increment of the SAI (which in this study ranged from 0 to 12 due to lack of data on some of the components of the SAI) increases the chances of being listed by 19% and the chances of being transplanted (among those already listed) by 6%.Citation74 ESRD patients with lower SAI may be at risk of lower referral rates, delays in work-up, less regular follow-up, lower rate of listing and inferior rate of transplantation even when already on the waiting list. Lower SAI in this study was also associated with racial minorities and female sex similarly to existing data demonstrating that racial minorities and women are at risk of disparities.Citation7,Citation9,Citation75,Citation76
Table 1. The socioeconomic status included in the SAI, each graded on a scale of 0–3.
SAI therefore seems to be a reasonable quantifiable indicator of belonging to a disadvantaged population, which is prone to experiencing disparities and associated with poor outcome and inferior access to healthcare.
Potential interventions
The mechanism of disparities is likely to be multifactorial and some underlying socioeconomic factors may in fact be modified. Specifically, we would like to underscore the significance of education which is associated with income,Citation77 insurance statusCitation30 and employment.Citation78 Based on the data presented above we think that few interventions might be beneficial in alleviating disparities. Specifically, education programs and improving health literacy may improve the outcome in those with lower SAI.Citation79 Patient navigation systems might streamline the process of pre-transplant evaluation and improve access to transplantation.Citation80 Reimbursement policies and benefit extensions might be considered.Citation38 In addition, one might consider integrating an employment specialist into the healthcare team to provide vocational support. Furthermore, minimization of substance abuse by increasing awareness of patients to factors associated with successful listing and transplantation might also improve the SAI and transplant outcome.
Conclusion
Based on current literature disparities do exist in access to kidney transplantation and its outcome. Socio-economic factors (i.e. education level, employment status, income level, marital status and substance abuse) being unequally distributed in disadvantaged groups are likely to play a significant role in the observed disparities. The intervention programs should be focused on sub-populations at higher risk determined by quantified indicator of disadvantaged social status such as social adaptability index.
Declaration of interest
The authors of this manuscript have no conflicts of interest to disclose.
References
- Ladin K, Rodrigue JR, Hanto DW. Framing disparities along the continuum of care from chronic kidney disease to transplantation: Barriers and interventions. Am J Transplant. 2009;9:669–674
- Goldfarb A-Rumyantzev, Hurdle JF, Scandling J, et al. Duration of end-stage renal disease and kidney transplant outcome. Nephrol Dial Transplant. 2005;20:167–175
- Meier HU-Kriesche, Port FK, Ojo AO, et al. Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58:1311–1317
- Becker BN, Rush SH, Dykstra DM, Becker YT, Port FK. Preemptive transplantation for patients with diabetes-related kidney disease. Arch Intern Med. 2006;166:44–48
- Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation -- clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343:1537–1544
- Fan PY, Ashby VB, Fuller DS, et al. Access and outcomes among minority transplant patients, 1999-2008, with a focus on determinants of kidney graft survival. Am J Transplant. 2010;10:1090–1107
- Dudley CR, Johnson RJ, Thomas HL, Ravanan R, Ansell D. Factors that influence access to the national renal transplant waiting list. Transplantation. 2009;88:96–102
- Wong LL, Kindle K, Limm B. Racial disparities in Pacific Islanders undergoing renal transplant evaluation. Hawaii Med J. 2009;68:30–33
- Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM. Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol. 2009;20:1333–1340
- Thamer M, Hwang W, Fink NE, et al. U. nephrologists S' attitudes towards renal transplantation: results from a national survey. Transplantation. 2001;71:281–288
- Joshi S, Gaynor JJ, Bayers S, et al. Disparities among blacks, hispanics, whites in time from starting dialysis to kidney transplant waitlisting. Transplantation. 2013;95:309–318
- Johansen KL, Zhang R, Huang Y, Patzer RE, Kutner NG. Association of race and insurance type with delayed assessment for kidney transplantation among patients initiating dialysis in the United States. Clin J Am Soc Nephrol. 2012;7:1490–1407
- Goldfarb AS-Rumyantzev, Sandhu GS, Baird B, et al. Effect of education on racial disparities in access to kidney transplantation. Clin Transplant. 2011;26:74–81
- Goldfarb AS-Rumyantzev, Sandhu GS, Barenbaum A, et al. Education is associated with reduction in racial disparities in kidney transplant outcome. Clin Transplant. 2012;26:891–899
- Mocan N, Tekin E. The determinants of the willingness to donate an organ among young adults: evidence from the United States and the European Union. Soc Sci Med. 2007;65:2527–2538
- Chaudhry SI, Herrin J, Phillips C, et al. Racial disparities in health literacy and access to care among patients with heart failure. J Card Fail. 2011;17:122–127
- Unruh ML, Evans IV, Fink NE, Powe NR, Meyer KB, Skipped treatments, markers of nutritional nonadherence, survival among incident hemodialysis patients. Am J Kidney Dis. 2005;46:1107–1116
- Goldfarb AS-Rumyantzev, Wright S, Ragasa R, et al. Factors associated with nonadherence to medication in kidney transplant recipients. Nephron Clin Pract. 2010;117:c33–c39
- Tuohy KA, Johnson S, Khwaja K, Pavlakis M. Gender disparities in the live kidney donor evaluation process. Transplantation. 2006;82:1402–1407
- Kayler LK, Meier HU-Kriesche, Punch JD, et al. Gender imbalance in living donor renal transplantation. Transplantation. 2002;73:248–252
- Segev DL, Kucirka LM, Oberai PC, et al. Age and comorbidities are effect modifiers of gender disparities in renal transplantation. J Am Soc Nephrol. 2009;20:621–628
- Axelrod DA, Dzebisashvili N, Schnitzler MA, et al. The interplay of socioeconomic status, distance to center, interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol. 2010;5:2276–2288
- Ghahramani N, Sanati A-Mehrizy, Wang C. Perceptions of patient candidacy for kidney transplant in the United States: A qualitative study comparing rural and urban nephrologists. Exp Clin Transplant. 2014;12:9–14
- Ghahramani N, Wang C, Sanati A-Mehrizy, Tandon A. Perception about transplant of rural and urban patients with chronic kidney disease; a qualitative study. Nephrourol Mon 2014;6:e15726
- US Renal Data System, USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD; 2012
- Do DP, Frank R, Finch BK. Does SES explain more of the black/white health gap than we thought? Revisiting our approach toward understanding racial disparities in health. Soc Sci Med. 2012;74:1385–1393
- Braveman PA, Egerter SA, Cubbin C, Chi KS. An approach to studying social disparities in health and health care. Am J Public Health. 2004;94:2139–2448
- Muller C, Riegle C-Crumb, Schiller KS, Wilkinson L, Frank KA. Race and academic achievement in racially diverse high schools: Opportunity and stratification. Teach Coll Rec. 2010;112:1038–1063
- Petersen E, Baird BC, Barenbaum LL, et al. The impact of employment status on recipient and renal allograft survival. Clin Transplant. 2008;22:428–438
- Goldfarb AS-Rumyantzev, Koford JK, Baird BC, Chelamcharla M, Habib AN, Wang BJ, et al. Role of socioeconomic status in kidney transplant outcome. Clin J Am Soc Nephrol. 2006;1:313–322
- Naiman N, Baird BC, Isaacs RB, et al. Role of pre-transplant marital status in renal transplant outcome. Clin Transplant. 2007;21:38–46
- Gueye AS, Chelamcharla M, Baird BC, et al. The association between recipient alcohol dependency and long-term graft and recipient survival. Nephrol Dial Transplant. 2007;22:891–898
- Schaeffner ES, Mehta J, Winkelmayer WC. Educational level as a determinant of access to and outcomes after kidney transplantation in the United States. Am J Kidney Dis. 2008;51:811–818
- Grubbs V, Gregorich SE, Perez EJ-Stable, Hsu CY. Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol. 2009;4:195–200
- Juergensen PH, Gorban N-Brennan, Finkelstein FO. Compliance with the dialysis regimen in chronic peritoneal dialysis patients: Utility of the pro card and impact of patient education. Adv Perit Dial. 2004;20:90–92
- Alexander GC, Sehgal AR. Barriers to cadaveric renal transplantation among blacks, women, the poor. JAMA. 1998;280:1148–1152
- Federman AD, Adams AS, Ross D-Degnan, Soumerai SB, Ayanian JZ. Supplemental insurance and use of effective cardiovascular drugs among elderly medicare beneficiaries with coronary heart disease. JAMA. 2001;286:1732–1739
- Woodward RS, Page TF, Soares R, Schnitzler MA, Lentine KL, Brennan DC. Income-related disparities in kidney transplant graft failures are eliminated by Medicare's immunosuppression coverage. Am J Transplant. 2008;8:2636–2346
- Stephens MR, Evans M, Ilham MA, sden A, Asderakis A. The influence of socioeconomic deprivation on outcomes following renal transplantation in the United Kingdom. Am J Transplant. 2010;10:1605–1612
- Volkova N, McClellan W, Klein M, et al. Neighborhood poverty and racial differences in ESRD incidence. J Am Soc Nephrol. 2008;19:356–364
- Page TF, Woodward RS, Brennan DC. The impact of Medicare's lifetime immunosuppression coverage on racial disparities in kidney graft survival. Am J Transplant. 2012;12:1519–1527
- Sahota A, Zaghla H, Adkins R, et al. Predictors of employment after liver transplantation. Clin Transplant. 2006;20:490–495
- Paris W Returning to work after heart transplantation. J Heart Lung Transplant. 1993;12:46–53
- van S der Mei Clinical factors influencing participation in society after successful kidney transplantation. Transplantation. 2006;82:80–85
- Rongey C, Bambha K, Vanness D, et al. Employment and health insurance in long-term liver transplant recipients. Am J Transplant 2005;5:1901–1908
- Matas LW, McHugh L, Gillingham K, et al. Employment patterns after successful kidney transplantation. Transplantation. 1996;51:729–733
- White JA-Williams C, Grady K. Who returns to work after heart transplantation? J Heart Lung Transplant. 2005;24:2255–2261
- Zhang H, Xu W, Dahl AK, Xu Z, Wang HX, Qi X. Relation of socio-economic status to impaired fasting glucose and Type 2 diabetes: Findings based on a large population-based cross-sectional study in Tianjin, China. Diabet Med. 2013;8:157–162
- Dupre ME, George LK, Liu G, Peterson ED. The cumulative effect of unemployment on risks for acute myocardial infarction. Arch Intern Med. 2013;172:1731–1737
- Araujo SM, de VM Bruin, Daher F Ede, Almeida GH, Medeiros CA, de PF Bruin. Risk factors for depressive symptoms in a large population on chronic hemodialysis. Int Urol Nephrol. 2011;44:1229–1235
- Chung ML, Lennie TA, Riegel B, Wu JR, Dekker RL, Moser DK. Marital status as an independent predictor of event-free survival of patients with heart failure. Am J Crit Care. 2009;18:562–70
- Datta GD, Neville BA, Kawachi I, Datta NS, Earle CC. Marital status and survival following bladder cancer. J Epidemiol Community Health. 2009;63:807–813
- Goldzweig GE, Hubert A, Walach N, Perry S, Brenner B, et al. How relevant is marital status and gender variables in coping with colorectal cancer? A sample of middle-aged and older cancer survivors. Psychooncology. 2009;18:866–874
- Khattak MW, Sandhu GS, Woodward R, Stoff JS, Goldfarb AS-Rumyantzev. Association of marital status with access to renal transplantation. Am J Transplant. 2010;10:2624–2631
- Sandhu GS, Khattak M, Woodward RS, et al. Impact of substance abuse on access to renal transplantation. Transplantation. 2011;91:86–93
- Gonzalez A, Barinas J, C'Cleirigh O. Substance use: Impact on adherence and HIV medical treatment. Curr HIV/AIDS Rep. 2011;8:223–234
- Fabrizi F, Tin P, Ponticelli C. Hepatitis C virus infection and renal transplantation. Am J Kidney Dis. 2001;38:919–934
- Lin SJ, Koford JK, Baird BC, et al. Effect of donors' intravenous drug use, cigarette smoking, alcohol dependence on kidney transplant outcome. Transplantation. 2005;80:482–486
- Lederer DJ, Caplan CE-Shaw, MK'Shea O, et al. Racial and ethnic disparities in survival in lung transplant candidates with idiopathic pulmonary fibrosis. Am J Transplant. 2006;6:398–403
- Mahle WT, Kanter KR, Vincent RN. Disparities in outcome for black patients after pediatric heart transplantation. J Pediatr. 2005;147:739–743
- Keyhani S, Scobie JV, Hebert PL, McLaughlin MA. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension. 2008;51:1149–1155
- Axelrod DA, Guidinger MK, Finlayson S, et al. Rates of solid-organ wait-listing, transplantation, survival among residents of rural and urban areas. JAMA. 2008;299:202–207
- Ikeda A, Iso H, Toyoshima H, et al. Marital status and mortality among Japanese men and women: The Japan Collaborative Cohort Study. BMC Public Health. 2007;7:73. doi: 10.1186/1471-2458-7-73
- Diaz VA Jr. Cultural factors in preventive care: Latinos. Prim Care. 2002;29:503–517
- Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335:791–799
- Finkelstein JA, Lozano P, Farber HJ, Miroshnik I, Lieu TA. Underuse of controller medications among Medicaid-insured children with asthma. Arch Pediatr Adolesc Med. 2002;156:562–567
- Gurwitz JH, Goldberg RJ, Malmgren JA, et al. Hospital transfer of patients with acute myocardial infarction: The effects of age, race, insurance type. Am J Med. 2002;112:528–534
- Priebe S, Watzke S, Hansson L, Burns T. Objective social outcomes index (SIX): a method to summarise objective indicators of social outcomes in mental health care. Acta Psychiatr Scand. 2008;118:57–63
- Goldfarb A-Rumyantzev, Barenbaum A, Rodrigue J, Rout P, Isaacs R, Mukamal K. New social adaptability index predicts overall mortality. Arch Med Sci. 2012;7:720–727
- Goldfarb AS-Rumyantzev, Rout P, Sandhu GS, et al. Social adaptability index predicts overall mortality in patients with diabetes. J Diabetes Complications. 2012;26:444–449
- Goldfarb AS-Rumyantzev, Rout P, Sandhu GS, Khattak M, Tang H, Barenbaum A. Association between social adaptability index and survival of patients with chronic kidney disease. Nephrol Dial Transplant. 2010;25:3672–3681
- Sandhu GS, Khattak M, Rout P, et al. Social Adaptability Index: application and outcomes in a dialysis population. Nephrol Dial Transplant. 2011;26:2667–2674
- Garg J, Karim M, Tang H, et al. Social adaptability index predicts kidney transplant outcome: A single-center retrospective analysis. Nephrol Dial Transplant. 2011;27:1239–1245
- Goldfarb AS-Rumyantzev, Sandhu GS, Baird BC, Khattak M, Barenbaum A, Hanto DW. Social Adaptability Index predicts access to kidney transplantation. Clin Transplant. 2011;25:834–842
- Vamos EP, Novak M, Mucsi I. Non-medical factors influencing access to renal transplantation. Int Urol Nephrol. 2009;41:607–616
- Malek SK, Keys BJ, Kumar S, Milford E, Tullius SG. Racial and ethnic disparities in kidney transplantation. Transpl Int. 2011;24:419–424
- Educational attainment in the United States: ch 2000 (Update): US Census Bureau, Washington DC. Available at: http://www.census.gov/population/www/socdemo/educ-attn.html. Accessed December 7, 2005
- Chisholm MA-Burns, Erickson SR, Spivey CA, Kaplan B. Health-related quality of life and employment among renal transplant recipients. Clin Transplant. 2012;26:411–417
- Patzer RE, Perryman JP, Pastan S, et al. Impact of a patient education program on disparities in kidney transplant evaluation. Clin J Am Soc Nephrol. 2012;7:648–655
- Sullivan C, Leon JB, Sayre SS, et al. Impact of navigators on completion of steps in the kidney transplant process: A randomized, controlled trial. Clin J Am Soc Nephrol. 2012;7:1639–1645