Abstract
Background: Vascular calcification significantly increases the rates of cardiovascular mortality in hemodialysis (HD) patients. Abnormalities in mineral metabolism may play a role in the pathogenesis of arterial calcification. Whether patients treated with non-calcium-based phosphate binders had reduced aortic vascular calcification compared to those treated with calcium-based phosphate binders is still unclear. Methods: We searched multiple databases for studies published through August 2013 that evaluated the effects of non-calcium-based phosphate binders (NCBP) versus calcium-based phosphate binders (CBP) on cardiovascular calcification and bone remodeling among dialysis patients. We summarized test performance characteristics with the use of forest plots, fixed and random effects models, and Egger regression test. Results: Eighteen eligible randomized controlled trials totaling 3676 patients were included. Meta-analysis results showed NCBP could significantly attenuate the progression of coronary artery calcification than CBP (WMD: −144.62, 95% CI: −285.62 to −3.63). The serum calcium levels significant lower in NCPB group than in CPB groups (WMD: −0.26, 95% CI: −0.37 to −0.14), but the serum iPTH levels were significantly higher in NCPB groups (WMD: 57.1, 95% CI: 13.42 to 100.78). The osteoid volume and osteoblast numbers were significant higher in NCPB group than in CPB group (WMD: 1.75, 95% CI: 0.78 to 2.73 for osteoid volume; WMD: 4.49, 95% CI: 1.83 to 7.15 for osteoblast numbers). The Egger regression test also showed no potential publication bias (p = 0.725). Conclusions: Based on available data, NCBPs have equally effective with CBPs for serum phosphate control. But there was significantly lower incidence of coronary artery calcification and a significant higher bone formatting rate in NCBP groups than in CBP groups. So we recommend NCBPs as phosphate binders for HD patients.
Introduction
Cardiovascular mortality and total mortalities are 10- to 100-folds higher in patients on hemodialysis (HD) than in age-matched controls. The risk of cardiovascular death of a 30-year-old HD patient is similar to that of an 80-year-old in the general population.Citation1,Citation2
Vascular calcification significantly increases the rates of cardiovascular mortality in hemodialysis (HD) patients.Citation3 Several factors involve in the pathogenesis of vascular calcification, such as abnormal mineral metabolism, calcium and phosphate excess, and uremia. Recent years, chronic kidney disease-mineral bone disorder (CKD-MBD) is introduced as a new clinical syndrome, in which the phosphate is the one of most important biochemical parameter and inducer of vascular calcification.Citation4 Several studies have showed that serum levels of phosphate were linearly and independently associated with cardiovascular mortality in dialysis CKD patients.Citation5,Citation6 The use of phosphate binders have been associated with improved survival in hemodialysis patients.Citation7 There are mainly two kinds of phosphate binders, calcium-based (CBP) and non-calcium-based binders (NCBP). Calcium-based binders are widely used as it is inexpensive and effective. However, administration of calcium can lead to hypercalcemia, and increase the risk of metastatic calcification which is significantly associated with the likelihood of developing vascular calcification and CKD-MBD.Citation8 NCBPs binders do not contain calcium. Several studies demonstrated that taking the NCBPs could reduce progression of vascular calcification and improve CKD-MBD status among HD patients.Citation9,Citation10
Lanthanum carbonate (LC) and sevelamer are phosphate binders that do not contain aluminium or calcium. Studies have showed that LC and sevelamer are not only as effective as calcium-based binders, but also potentially improve bone health and helps in reduction of vascular calcification by reducing exogenous calcium.Citation11 Several clinical trials have compared NCBP (LC and sevelamer) and CBP on vascular calcification and cardiovascular mortality, but the results are inconclusive. To make this issue clear, we performed a systematic review and meta-analysis to compare NCBP and CBP on cardiovascular mortality and serum markers of mineral metabolism among patients with dialysis.
Methods
Search strategy
We searched Medline (1966-August 2013), Embase (1980- August 2013), Science Citation Index (1981-August 2013), Cochrane Central Register of Controlled Trials (CENTRAL) and Cochrane Database of Systematic Reviews (Cochrane Library, Issue 2, 2013) for randomized clinical trials that compared NCBP and CBP among dialysis patients. The following terms were used: “lanthanum carbonate”, “sevelamer”, “calcium acetate”, “calcium carbonate”, “hemodialysis” and “chronic kidney disease”. Searches were not restricted by year of publication or language. Reference lists of all included studies were scanned to identify additional potentially relevant studies. Two reviewers independently screened the titles and abstracts of identified papers, and full text copies of all potentially relevant studies were obtained.
Study selection and outcomes
We included studies if they were randomized trials that compared CBPs with NCBPs for cardiovascular calcification and bone remodeling among HD patients.
The primary outcome was change in coronary artery calcium (CAC) level from baseline to end of treatment, the second outcomes were serum calcium level, intact parathyroid hormone (iPTH), osteoid volume and osteoblast numbers.
Data extraction
Two reviewers independently extracted the data information of trial characteristics, patients' data, outcome measures, and study qualities using a standardized protocol and reporting document. Disagreements were resolved by consensus. To quantify the level of agreement between reviewers, a κ statistic was calculated. The κ statistic is a chance-corrected proportional index, with values ranging from +1 (perfect agreement) to −1 (complete disagreement). Information extracted included personal information, methodology, details on interventions, and reported outcomes.
Study quality assessment
We assessed the methods of included studies according to Cochrane Handbook for Systematic Reviews of Interventions, including reporting of randomization method, allocation concealment, blinding of outcome assessment, and completeness of follow-up.
Statistical analysis
The meta-analysis was done in line with recommendations from the Cochrane Collaboration and the Quality of Reporting of Meta-analyses guidelines (QUOROM)Citation12 with standard software (Review manager (RevMan), version 5.2, Cochrane collaboration, The Nordic Cochrane Centre, Copenhagen).Citation13 Sensitive analysis was on an intention-to-treat basis. Heterogeneity was assessed with I2 statistics and Q statistic.Citation14 I2 is the proportion of total variation observed between the trials attributable to differences between trials rather than sampling error (chance). Relative risk (RR) was used as the summary statistic to perform statistical analysis of dichotomous variables. Continuous outcomes were pooled using the weighted mean difference (WMD). A fixed-effect model was used for calculations of summary estimates and their 95% CI. However, when the heterogeneity was significant, a random-effects model was used. Egger regression model was used to evaluate the potential publication bias.
Results
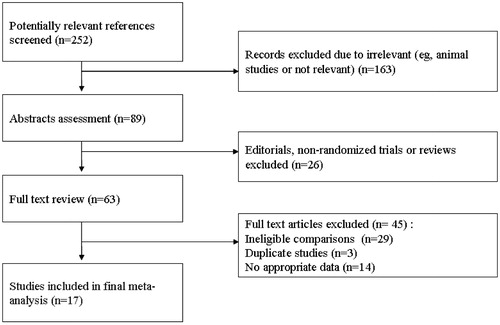
We identified 252 potentially relevant publications. Eighteen trialsCitation4,Citation9,Citation10,Citation15–29 met the predefined inclusion criteria and were included in our meta-analysis (). The 18 trails included 3676 patients (). CAC score was reported in 8 trials.Citation8,Citation9,Citation18,Citation20–22,Citation26,Citation30 Eight trialsCitation4,Citation10,Citation17,Citation18,Citation20,Citation21,Citation28 reported all cause mortality, however only 4 trials reported cardiovascular events.Citation17,Citation18,Citation21,Citation26 Serum markers of mineral metabolism changes were reported in 16 trials.Citation4,Citation9,Citation10,Citation15–21,Citation23,Citation24,Citation27–29
Table 1. Characteristics of included studies.
After adjustment for the agreement between reviewers, the κ coefficient on the agreement of the included studies was 0.92 (95% confidence interval 0.83 to 0.95), suggesting good agreement between reviewers in data extraction. All studies were randomized controlled trials. The methodological quality of the included studies was summarized in .
Table 2. Quality assessment of included studies.
Coronary artery calcification
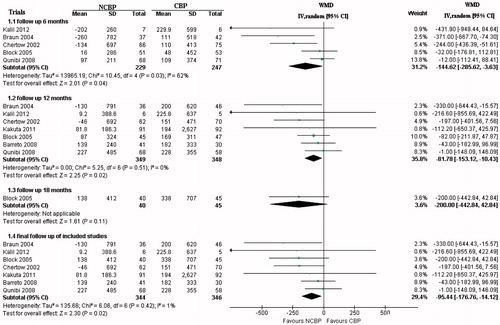
Seven trialsCitation8,Citation18,Citation20–22,Citation26,Citation30 provided data of CAC scores (n = 697). We performed meta-analysis analysis according to the duration of follow-up (). At 6 months follow-up, the increase of CAC scores from baseline were significantly lower in NCPB groups than in CPB groups (WMD: −144.62, 95% CI:−285.62 to −3.63), but there was significant heterogeneity between trials (χ2 = 10.45, p = 0.03, I2 = 62%). At 12 months and final follow-up, the increase of CAC scores from baseline were also significantly lower in NCPB groups than in CPB groups (WMD: −81.78, 95% CI: −153.12 to −10.43 for 12 months; WMD: −95.44, 95% CI: −176.76 to −14.12 for final follow-up), with no significant heterogeneity between trials (χ2 = 5.25, p = 0.51, I2 = 0% for 12 months; χ2 = 6.06, p = 0.42, I2 = 1% for final follow-up).
Cardiovascular events and all cause mortality
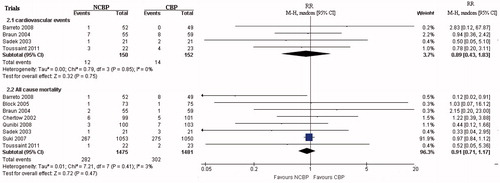
Eight trialsCitation4,Citation10,Citation17,Citation18,Citation20,Citation21,Citation26,Citation28 provided data about all cause mortality (n = 2956), and four trialsCitation17,Citation18,Citation21,Citation26 reported cardiovascular events. For reduction of cardiovascular events, the meta-analysis showed the pooled RR was 0.89; 95% CI (0.43, 1.83), with no significant heterogeneity between trials (χ2 = 0.79, p = 0.85, I2 = 0%; ). This result was not statistically significant (p = 0.75), but in favor of NCPB groups. When compared all cause mortality between NCPB groups and CPB groups, there was also no significant difference (RR: 0.91, 95% CI: 0.71 to 1.17), but with less incidence in NCPB groups (). The test for homogeneity showed that results were consistent across trials (p = 0.47, I2 = 3%).
Serum biochemical markers of mineral metabolism
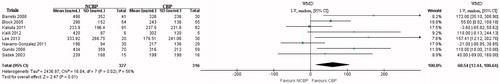
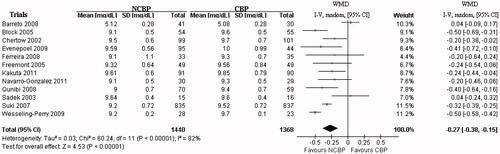
We summarized the comparison results of serum mineral metabolism markers changes between NCPB groups and CPB groups in , including iPTH, Calcium, Phosphate, Ca × P, LDL-C, HDL-C, Pentosidine, WBC, AKP, Osteoprotegerin, sRANKL, Deoxypyridoline, Triglycerides, CRP, Uric acid, HbA1c and BSAP.
Table 3. Comparison of serum mineral metabolism markers changes between NCPB groups and CPB groups.
The pooled results showed that serum iPTH levels were significantly higher in NCPB groups than in CPB groups (WMD: 57.1, 95% CI: 13.42 to 100.78). The test for homogeneity showed there were significant heterogeneity of these trial results (p = 0.04, I2 = 50%; ). The serum calcium levels were significantly lower in NCPB group than in CPB group (WMD: −0.26, 95% CI: −0.37 to −0.14; ). The test for homogeneity showed there were significant heterogeneity of these trial results (p < 0.0001, I2 = 81%). The serum LDL-C levels were significantly lower in NCPB group than in CPB group (WMD: −20.93, 95% CI: −30.56 to −11.3). The test for homogeneity showed there were significant heterogeneity of these trial results (p < 0.0001, I2 = 89%). The serum AKP and BSAP levels were significantly higher in NCPB group than in CPB group (WMD: 28.27, 95% CI: 12.61 to 43.93 for AKP; WMD: 8.79, 95% CI: 4.29 to 13.29 for BSAP). The test for homogeneity showed that results were consistent across trials (p = 0.91, I2 = 0% for AKP; p = 0.76, I2 = 0% for BSAP). There were no significant difference of serum phosphate and HDL-C level between NCPB group and CPB group (WMD: 0.06, 95% CI: −0.09 to 0.20 for serum phosphate levels; WMD: 0.53, 95% CI: −1.02 to 2.09 for serum HDL-C levels), with no significant heterogeneity of included trials (p = 0.09, I2 = 38% for serum phosphate levels; p = 0.4, I2 = 4% for serum HDL-C levels).
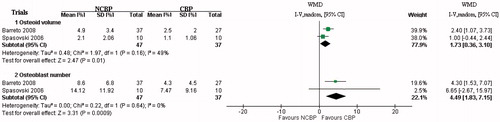
Bone histomorphometry
Two trialsCitation18,Citation25 provided data about bone histomorphometry (n = 84). The osteoid volume and osteoblast numbers were significantly higher in NCPB group than in CPB group (WMD: 1.75, 95% CI: 0.78 to 2.73 for osteoid volume; WMD: 4.49, 95% CI: 1.83 to 7.15 for osteoblast numbers), with no significant heterogeneity of included trials (p = 0.16, I2 = 49% for osteoid volume; p = 0.64, I2 = 0% for osteoblast numbers; ).
Sensitivity analysis
By fixed-effect and random-effect models, we found serum phosphate levels showed inconsistent results. We performed sensitivity analyses by excluding trialsCitation17,Citation24,Citation28 of “unclear randomization methods”. The results showed there was no difference of serum phosphate levels between two groups. For iPTH, the heterogeneity was significant difference. We performed sensitivity analyses by excluding the trialCitation16 of “follow-up length only 12 weeks”. The heterogeneity was not significant difference, and the results did not change. The heterogeneity of serum calcium and Ca × P levels was significant difference. We performed sensitivity analyses by excluding trials of the mean age's significant difference from others (pediatric dialysis patients or mean ages <50 years). The heterogeneity was not significant, and the results did not change.
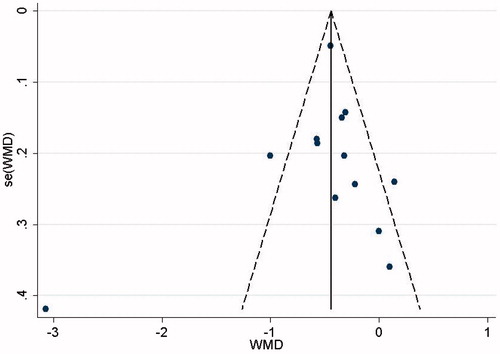
Publication bias
The funnel plot showed that publication bias seemed to be fairly well distributed, with no definite evidence of asymmetry. The Egger regression test also showed no significant publication bias (p = 0.725; ).
Discussion
Our results suggested that NCBP could attenuate the progression of coronary artery calcification in HD patients. However, there was no significant difference in cardiovascular events and all cause mortality between the two treatment groups. Compared with CBP groups, NCBP groups had lower calcium levels, higher iPTH levels, osteoid volumes and osteoblast numbers. So compared with CBP, NCBP is less likely to cause progressive coronary artery calcification, hypercalcemia, low levels PTH, and progressive bone loss.
Cardiovascular calcification in HD patients has been associated with age, diabetes, serum calcium, phosphorus, PTH, LDL and triglyceride concentrations, and markers of inflammation.Citation31
Hyperphosphatemia is a common complication in patients with end-stage renal disease. Hyperphosphatemia results in hyperparathyroidism, metabolic bone disease, soft tissue and vascular calcification and other metabolic derangements. So the control of serum phosphate has long been a goal of CKD treatment. In our analysis, we founded that both groups had adequate serum phosphate control without significant difference and heterogeneity. Inadequate calcium control eventually leads to increased cardiovascular calcification, arterial dysfunctional morbidity and mortality. Studies have demonstrated the calcium-based phosphate binder is associated with arterial calcification and low bone turnover.Citation32,Citation33 In our study, we found the serum calcium levels in CBP groups were significant higher than in NCBP groups. Our meta-analysis results showed that CAC scores were in significant lower in NCBP groups. This result was different from previous two meta-analysis.Citation34,Citation35 This may due to our studies included more study populations. However, the serum calcium level may not reflect the total body calcium load and excess calcium may be prone to deposit in the tissues when the serum phosphate is high or when there is low bone turnover (with reduced intact PTH).Citation4 In our study, we there were no significant difference between groups of cardiovascular events and all cause mortality. This may partly due to this reason.
Our results showed that the serum PTH level in the CBP group was significantly lower than NCBP. Hypercalcemia tends to suppress serum PTH level. The PTH oversuppression would lead to lower bone turnover, lower bone density, and decrease uptake of supplemental calcium in the bone. This will result in a higher risk of vascular calcification.Citation18
Hyperuricemia may be associated with a number of disorders in HD patients, including insulin resistance, dyslipidemia, hypertension and cardiovascular disease.Citation36 In our study, we could see the beneficial effects of NCBP on serum lipids in HD patients. Significant reductions in LDL-cholesterol were seen in NCBP groups but not in CBP groups.
Inflammation, a prevalent condition in HD patients, also plays a pivotal role in diverse complications, and it is a strong predictor of mortality. Increased serum phosphorus is an independent risk factor for the presence of a significant inflammatory state in HD patients. Studies have showed that sevelamer treatment resulted in significant reductions of serum phosphorus and CRP levels. In our study, the analysis result showed no significant difference between NCBP groups and CBP groups. But there was significant heterogeneity. When we excluded the study of Evenepoel et al.Citation19 which was conducted in 7 countries of Europe, there was no significant heterogeneity. The result showed the serum CRP level was significantly lower in NCBP groups. So the different races may affect the treatment results.
In our study, osteoid volume and osteoblast numbers were significantly higher in NCBP groups than in CBP groups. This means NCBP would not cause a mineralization defect or osteomalacia, but improve osteoblasts activity. Interestingly, the two included trials used lanthanum carbonate and sevelamer as NCBP respectively. The result showed no significant heterogeneity. The exact mechanism is unknown. Animals' studies had demonstrated that LC and sevelamer have an anabolic effect on bone tissue.Citation37,Citation38
All meta-analyses are subject to potential bias because of systematic and random errors.Citation39 Our meta-analysis of randomized controlled trials may have several limitations. Firstly, the number of the included studies and participants were relatively small. Secondly, most of included studies were without adequate allocated concealment and blinding. This may affect study results. Thirdly, several results were considered heterogeneous including iPTH, calcium, LDL-C, CRP. Though we performed sensitive analysis, including excluded pediatric dialysis patients, short duration of follow-ups, different races, lower methodological quality, and the reliability of analysis results may still be affected.
Conclusions
In summary, although there are some limitations in our meta-analysis, based on available data, NCBPs have equal effect with CBPs for serum phosphate control. But there was significantly lower incidence of coronary artery calcification and a significant higher bone formatting rate in NCBP groups than in CBP groups. So we recommend NCBPs as phosphate binders for HD patients.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article. This study was supported by the Natural Science Funds of Zhejiang province (Y2081014).
Acknowledgments
We thank all the patients and clinical researchers who were involved in the publications we mentioned in this article.
References
- de Jager DJ, Grootendorst DC, Jager KJ, et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA. 2009;302:1782–1789
- Levey AS, Beto JA, Coronado BE, et al. Controlling the epidemic of cardiovascular disease in chronic renal disease: What do we know? What do we need to learn? Where do we go from here? National Kidney Foundation Task Force on Cardiovascular Disease. Am J Kidney Dis. 1998;32:853–906
- Guerin AP, London GM, Marchais SJ, Metivier F. Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant. 2000;15:1014–1021
- Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–252
- Young EW, Albert JM, Satayathum S, et al. Predictors and consequences of altered mineral metabolism: The Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2005;67:1179–1187
- Block GA, Hulbert-Shearon TE, Levin NW, Port FK. Association of serum phosphorus and calcium × phosphate product with mortality risk in chronic hemodialysis patients: A national study. Am J Kidney Dis. 1998;31:607–617
- Ketteler M, Biggar PH. Use of phosphate binders in chronic kidney disease. Curr Opin Nephrol Hypertens. 2013;22:413–420
- Chertow GM, Raggi P, Chasan-Taber S, Bommer J, Holzer H, Burke SK. Determinants of progressive vascular calcification in hemodialysis patients. Nephrol Dial Transplant. 2004;19:1489–1496
- Kakuta T, Tanaka R, Hyodo T, et al. Effect of sevelamer and calcium-based phosphate binders on coronary artery calcification and accumulation of circulating advanced glycation end products in hemodialysis patients. Am J Kidney Dis. 2011;57:422–431
- Qunibi W, Moustafa M, Muenz LR, et al. A 1-year randomized trial of calcium acetate versus sevelamer on progression of coronary artery calcification in hemodialysis patients with comparable lipid control: The Calcium Acetate Renagel Evaluation-2 (CARE-2) study. Am J Kidney Dis. 2008;51:952–965
- Shigematsu T. Multicenter prospective randomized, double-blind comparative study between lanthanum carbonate and calcium carbonate as phosphate binders in Japanese hemodialysis patients with hyperphosphatemia. Clin Nephrol. 2008;70:404–410
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: The QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–1900
- Bradburn M, Deeks J, Altman D. Sbe24: Metan – an alternative meta-analysis command. Stata Technical Bull Reprints. 1998;8: 86–100
- Galbraith RF. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med. 1988;7:889–894
- Lee YK, Choi HY, Shin SK, Lee HY. Effect of lanthanum carbonate on phosphate control in continuous ambulatory peritoneal dialysis patients in Korea: A randomized prospective study. Clin Nephrol. 2013;79:136–142
- Navarro-Gonzalez JF, Mora-Fernandez C, Muros de Fuentes M, Donate-Correa J, Cazana-Perez V, Garcia-Perez J. Effect of phosphate binders on serum inflammatory profile, soluble CD14, and endotoxin levels in hemodialysis patients. Clin J Am Soc Nephrol. 2011;6:2272–2279
- Sadek T, Mazouz H, Bahloul H, et al. Sevelamer hydrochloride with or without alphacalcidol or higher dialysate calcium vs calcium carbonate in dialysis patients: An open-label, randomized study. Nephrol Dial Transplant. 2003;18:582–588
- Barreto DV, Barreto Fde C, de Carvalho AB, et al. Phosphate binder impact on bone remodeling and coronary calcification – results from the BRiC study. Nephron Clin Pract. 2008;110:c273–c283
- Evenepoel P, Selgas R, Caputo F, et al. Efficacy and safety of sevelamer hydrochloride and calcium acetate in patients on peritoneal dialysis. Nephrol Dial Transplant. 2009;24:278–285
- Block GA, Spiegel DM, Ehrlich J, et al. Effects of sevelamer and calcium on coronary artery calcification in patients new to hemodialysis. Kidney Int. 2005;68:1815–1824
- Braun J, Asmus HG, Holzer H, et al. Long-term comparison of a calcium-free phosphate binder and calcium carbonate--phosphorus metabolism and cardiovascular calcification. Clin Nephrol. 2004;62:104–115
- Kalil RS, Flanigan M, Stanford W, Haynes WG. Dissociation between progression of coronary artery calcification and endothelial function in hemodialysis patients: A prospective pilot study. Clin Nephrol. 2012;78:1–9
- Ferreira A, Frazao JM, Monier-Faugere MC, et al. Effects of sevelamer hydrochloride and calcium carbonate on renal osteodystrophy in hemodialysis patients. J Am Soc Nephrol. 2008,19:405–412
- Freemont AJ, Hoyland JA, Denton J. The effects of lanthanum carbonate and calcium carbonate on bone abnormalities in patients with end-stage renal disease. Clin Nephrol. 2005;64:428–437
- Spasovski GB, Sikole A, Gelev S, et al. Evolution of bone and plasma concentration of lanthanum in dialysis patients before, during 1 year of treatment with lanthanum carbonate and after 2 years of follow-up. Nephrol Dial Transplant. 2006;21:2217–2224
- Toussaint ND, Lau KK, Polkinghorne KR, Kerr PG. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in hemodialysis: A pilot randomized controlled trial. Nephrology (Carlton). 2011;16:290–298
- Wesseling-Perry K, Harkins GC, Wang HJ, et al. Response of different PTH assays to therapy with sevelamer or CaCO3 and active vitamin D sterols. Pediatr Nephrol. 2009;24:1355–1361
- Suki WN, Zabaneh R, Cangiano JL, et al. Effects of sevelamer and calcium-based phosphate binders on mortality in hemodialysis patients. Kidney Int. 2007;72:1130–1137
- Takei T, Otsubo S, Uchida K, et al. Effects of sevelamer on the progression of vascular calcification in patients on chronic hemodialysis. Nephron Clin Pract. 2008;108:c278–c283
- Qunibi WY, Hootkins RE, McDowell LL, et al. Treatment of hyperphosphatemia in hemodialysis patients: The Calcium Acetate Renagel Evaluation (CARE Study). Kidney Int. 2004;65:1914–1926
- Torres PA, De Broe M. Calcium-sensing receptor, calcimimetics, and cardiovascular calcifications in chronic kidney disease. Kidney Int. 2012;82:19–25
- London GM, Marty C, Marchais SJ, Guerin AP, Metivier F, de Vernejoul MC. Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol. 2004;15:1943–1951
- Andia CJB. Adynamic bone and chronic renal failure: An overview. Am J Med Sci. 2000;320:81–84
- Zhang Q, Li M, Lu Y, et al. Meta-analysis comparing sevelamer and calcium-based phosphate binders on cardiovascular calcification in hemodialysis patients. Nephron Clin Pract. 2010;115:c259–c267
- Jamal SA, Fitchett D, Lok CE, Mendelssohn DC, Tsuyuki RT. The effects of calcium-based versus non-calcium-based phosphate binders on mortality among patients with chronic kidney disease: A meta-analysis. Nephrol Dial Transplant. 2009;24:3168–3174
- Garg JP, Chasan-Taber S, Blair A, et al. Effects of sevelamer and calcium-based phosphate binders on uric acid concentrations in patients undergoing hemodialysis: A randomized clinical trial. Arthritis Rheum. 2005;52:290–295
- von Rosenberg SJ, Wehr UA. Lanthanum salts improve bone formation in a small animal model of post-menopausal osteoporosis. J Anim Physiol Anim Nutr (Berl). 2012;96:885–894
- Sampath TK, Simic P, Moreno S, et al. Sevelamer restores bone volume and improves bone microarchitecture and strength in aged ovariectomized rats. Endocrinology. 2008;149:6092–6102
- Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: Synthesis of best evidence for clinical decisions. Ann Intern Med. 1997;126:376–380