Abstract
Purpose: Hyponatremia is a common electrolyte abnormality in a variety of medical conditions. Lower predialysis serum sodium concentration is associated with an increased risk of death in oligoanuric patients on hemodialysis. However, whether hyponatremia affects the short-term mortality in chronic peritoneal dialysis (CPD) patients remains unclear. Methods: We conducted a cross-sectional and two-year follow-up review retrospectively, and 318 patients with CPD were enrolled in a medical center. Serum sodium levels were measured at baseline and categorized as quartile of Na: quartile 1 (124–135 mEq/L), quartile 2 (136–139), quartile 3 (140–141) and quartile 4 (142–148). Mortality and cause of death were recorded for longitudinal analyses. Results: The patients with higher quartile (higher serum sodium) had a trend of lower age, peritoneal dialysis (PD) duration, co-morbidity index, D/P Cr and white blood cell counts and higher renal Kt/Vurea (Kt/V) and serum albumin level. Stepwise multiple linear regression analysis showed that serum sodium level was positively associated with albumin, residual renal Kt/V and negatively associated with age and PD duration in CPD patients. After two-year follow-up, stepwise multivariate Cox proportional hazards model demonstrated that age, co-morbidity index and serum albumin were the significant risk factors for all-cause two-year mortality, but not serum sodium levels. Conclusions: Serum sodium level in CPD patients is associated with nutritional status, residual renal function and duration of PD. However, baseline serum sodium level is not an independent predictor of two-year mortality in CPD patients.
Introduction
Hyponatremia is a common electrolyte abnormality seen in a variety of medical conditions, including congestive heart failure, cirrhosis and the syndrome of inappropriate antidiuretic hormone.Citation1 Hyponatremia has been shown to predict adverse outcome in patients with acute myocardial infarction,Citation2 congestive heart failure,Citation3 pulmonary hypertensionCitation4 and even mild hyponatremia (serum sodium concentration 130–134 mEq/L) is associated with a 47% increased risk of in-hospital mortality.Citation5 Furthermore, in general population, hyponatremia is an independent predictor of deaths and myocardial infarction in middle-aged and elderly community subjects.Citation6 The reasons underlying these associations are unclear. Recently, lower predialysis serum sodium concentration is associated with an increased risk of death in oligoanuric patients on maintenance hemodialysis.Citation7 Each 4-mEq/L increment in baseline predialysis serum sodium concentration was associated with a hazard ratio (HR) for all-cause mortality of 0.84.
In peritoneal dialysis (PD), sodium removal by convective transport predominates over diffusive transport, thereby requiring an augmentation of ultrafiltrate volume to increase Na+ removal.Citation8 In chronic PD (CPD) patients, hyponatremia may occur either from water ingestion in excess of electrolyte, less solute intake or because of loss of electrolyte, mainly Na+ or K+. Hyponatremia has been reported to happen in 15% CPD patients in one year observation.Citation9 Furthermore, hyponatremia in CPD patients has been shown to be associated with lower residual renal function, malnutrition and more comorbidities.Citation9,Citation10 In addition, in a five-year follow-up, hyponatremia was not associated with mortality in CPD patients independently.Citation9 However, whether hyponatremia affects short term (two-year) mortality in CPD patient is not clear.
This two-year longitudinal study investigated the incidence and factors associated with serum sodium by clinically examining CPD patients. Furthermore, this study also analyzed whether baseline serum sodium level or hyponatremia contributed to mortality risk in these patients.
Patients and methods
This clinical investigation complied with the Declaration of Helsinki and was approved by the Medical Ethics Committee of Chang Gung Memorial Hospital (CGMH), Taipei, Taiwan, ROC.
Patients
All patients on maintenance PD in CGMH were included in this study. We retrospectively reviewed the records of all patients treated using PD from January 2005 to January 2007. The criteria for enrolment were PD > 6 months and age ≥ 18 years. The PD prescription for an individual patient was based on characteristics of patient's peritoneal membrane, determined by peritoneal equilibration tests. Intermittent therapies were employed primarily for patients with high-transport characteristics and continuous therapies for those with average- or low-transport characteristics. Forty-three patients were treated with automated PD, and 275 patients underwent continuous ambulatory PD. Dialysis prescription aimed to achieve a total Kt/V of at least 1.8/week.
Co-morbid diseases were evaluated according to the categories used by Chung SH.Citation11 Cardiovascular disease (CVD) included previous and present history of congestive heart failure, ischemic heart disease or cerebrovascular disease. Respiratory disease was defined as active tuberculosis, chronic lung disease or asthma attacks. Liver disease included persistently elevated serum glutamic-pyruvic transaminase and serum glutamic-oxaloacetic transaminase or cirrhosis defined by abdominal echo and clinical symptoms. Systemic disease included diabetes mellitus and systemic lupus erythematous.
Co-morbidity was graded by Davies index.Citation12 The co-morbid score of each patient is determined by the number of co-morbid diseases. Grade 0 (low risk) is a score of 0, grade 1 (medium risk) is a score of 1–2 and grade 2 (high risk) is a score of ≥ 3.
Patients who met the inclusion criteria were classified into four groups according to their serum sodium levels. The patient groups were as follows: quartile 1 patients with Na 124–135 mEq/L, quartile 2 patients with Na 136–139 mEq/L, quartile 3 patients with Na 140–141 mEq/L and quartile 4 patients with Na 142–148 mEq/L.
Laboratory measurements
All laboratory values, including blood cell counts, biochemical data, normalized protein nitrogen appearance (nPNA; measurement of nitrogen metabolism), peritoneal transport characteristics and parameters about residual renal function and dialysis adequacy, such as residual renal creatinine clearance (Ccr; normalized to body surface area), peritoneal Ccr, standard total Ccr (normalized to body surface area), residual renal Kt/V (measurement of urea kinetics and clearance), peritoneal Kt/V and total Kt/V, were measured by automated and standardized methods. All blood samples of patients with fasting status for at least 12 hours were collected in the morning, centrifuged and stored at −70 °C until use in assays. Serum albumin, creatinine, cholesterol, triglyceride, white blood cell (WBC) counts, hemoglobin, serum ferritin and transferrin saturation levels were assayed and recorded. Serum calcium was corrected for serum albumin according to the following formula: corrected calcium (in milligrams per deciliter) = serum calcium (in milligrams per deciliter) + 0.8 × [4.0 − serum albumin (in grams per deciliter)]. All other markers were analyzed by standard automated laboratory methods.
Follow-up
Patients were followed-up for two years after initial assessment. The end point of the study was the patient status (dead or alive) at termination of the follow-up period. Patients were censored at transfer to hemodialysis or other centers, renal transplantation or at the end of the observation period.
Statistical analysis
Unless otherwise stated, continuous variables are expressed as mean ± SD, and categorical variables are expressed as number or percentage for each item. Comparisons among the four patient groups were analyzed by one-way ANOVA. Logarithmic conversion was conducted for serum iPTH and ferritin levels. The independent links between baseline serum Na and variables were analyzed further with simple and stepwise backward multiple linear regression analyses, adjusting for other factors linked with Na level. The Cox proportional hazards model was used to measure all variables and determine the significance of variables for predicting the all-cause two-year mortality. To determine the risk of death, HR and 95% CI were obtained using the Cox proportional hazards model. A univariate Cox model, including all previously identified, important variables associated with mortality in maintenance PD patients, was used to measure mortality in the final multivariate model. A backward stepwise multivariate Cox regression model was also used to identify the risk factors for mortality in these patients. All statistical calculations were performed with SPSS for Windows (SAS Institute, Cary, NC).
Results
Patient characteristics
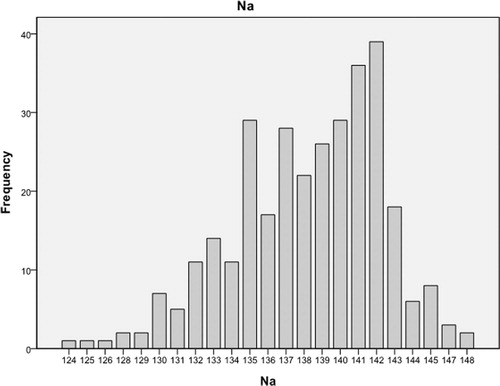
A total of 318 CPD patients (119 males and 199 females) with a mean PD duration of 3.9 ± 2.8 years were analyzed (). lists clinical properties, including age, gender, body mass index (BMI) and biological and hematological data. Mean patient age was 48.6 ± 12.2 year-old. At baseline, mean (SD), median, minimum and maximum baseline serum Na level were 138.2 (4.1), 139, 124 and 148 mEq/L, respectively (). also shows characteristics of patients in the four subgroups with different baseline Na levels. The patients with higher quartile (higher serum sodium) had a trend of lower age, PD duration, co-morbidity index, D/P Cr and WBC counts and higher renal Kt/V and serum albumin level. The groups did not differ in terms of gender, use of diuretics, total KT/V, standard total Ccr by week, nPNA, hemoglobin, serum potassium, cholesterol, triglyceride and ferritin.
Table 1. Baseline demographic and biochemical data in patients with CPD according to quartile of baseline serum Na levels.
Factors associated with serum sodium level in CPD patients
Simple linear regression analysis revealed that HbA1c was associated with age, BMI, high or high average of peritoneal solute transport, triglyceride and transferrin saturation. After adjusting for these significant variables with backward stepwise multiple linear regression analysis, serum sodium level was positively associated with albumin and residual renal Kt/V and negatively associated with age and PD duration in CPD patients ().
Table 2. Simple and multiple linear regression analysis of risk factors associated with baseline Na level in patients with CPD.
Cox regression multivariate analysis for two-year mortality in CPD patients
At the end of this study, 31 patients had died during the two-year study period, and the mortality rate was 9.7% in CPD patients. Eleven (13.1%) patients in quartile 1, 14 (15.0%) patients in quartile 2, 6 (9.2%) patients in quartile 3 and no patients in quartile 4 passed away during this period. Among these patients, 19 (19/31; 45.5%) died of infection and 12 (12/31, 54.5%) died of CVD.
All potential variables entered into the univariate Cox proportional hazards model revealed that age, co-morbidity index, CT ratio, serum HbA1c, Cr, Na, albumin and D/P Cr were the potential variables (p < 0.1) relating to HR of mortality and entered into the multivariate Cox model. Backward stepwise multivariate Cox proportional hazards model demonstrated that age, co-morbidity index and serum albumin were the significant risk factors for all-cause two-year mortality of our CPD patients after adjusting relating variables. But serum sodium was not an independent factor for all-cause mortality in these patients ().
Table 3. Univariate and multivariate Cox analysis of all-cause two-year mortality in patients with CPD, according to basal variables and serum sodium level.
Discussion
The study demonstrated that CPD patients with lower serum sodium had a significant trend of older age, longer PD duration, higher co-morbidity index, higher percentage of high and high-average transporter and WBC counts and lower residual renal Kt/V and serum albumin level than patients with higher serum sodium level. Moreover, factors associated with serum sodium level were further investigated. After related variables adjusted, multiple linear regression analysis demonstrated that serum sodium level was positively associated with albumin and residual renal Kt/V and negatively associated with age and PD duration in CPD patients. Albumin was also found to be a positively predictor of higher baseline serum sodium in maintenance hemodialysis patients.Citation7 Hyponatremia had been shown to be associated with a catabolic state and malnutrition in CPD patients.Citation13 Albumin levels were affected by the nutritional and catabolic status in patients. Therefore, albumin was a predictor of baseline serum sodium in CPD patients. PD duration was negatively associated with serum sodium in our study. In our previous study, the peritoneal transport of CPD patients increased gradually after 4–5 years of PD.Citation14 When peritoneal transport increased, the ultrafiltration volume tended to be reduced and patients tended to be edematous. In our CPD patients, patients with lower sodium level were associated with increased D/P Cr of peritoneal transport and higher percentage of high and high-average transport. Therefore, PD duration and age were negatively associated serum sodium level in the CPD patients. In addition, volume expansion tends to worsen when residual renal function declines in CPD patients, which may contribute to the development of hyponatremia.Citation15,Citation16 Thus, residual renal Kt/V was positively associated with serum sodium level in our study.
At the end of two-year follow-up, a total of 31 patients died. The two-year mortality rate in these PD patients was 9.7%. Cox univariate hazard analysis revealed that age, co-morbidity index, CT ratio, serum HbA1c, Cr, sodium, albumin and D/P Cr were possible significant risk factors for all-cause two-year mortality. However, cox multivariate hazard analysis revealed that age, co-morbidity index and serum albumin, but not baseline serum sodium or quartile of serum sodium, were significant risk factors for all-cause two-year mortality in CPD patients.
Hyponatremia has been reported a predictor of adverse outcomes in patient with heart failure,Citation3 myocardial infarction,Citation17 pulmonary arterial hypertension with right heart failureCitation4 and cirrhosis.Citation18 In these patients, hyponatremia develops primarily owing to greater activation of the reninangiotensin-aldosterone system,Citation19 excess vasopressin secretion in response to non-osmotic stimuli,Citation20 higher norepinephrine and epinephrine levelsCitation21 and more severe impairment of renal and hepatic flow.Citation20 The marked neurohormonal activations resulted in increased free-water reabsorption or reduction of renal water excretion, which contributed to the development of hyponatremia. In addition, mild hyponatremia also carried a poor prognosis in community subjects aged 55–75 years without apparent heart disease, stroke or cancer.Citation6
In patients with dialysis, due to loss of renal function, the mechanisms accounting for hyponatremia may be different. Waikar et al. recently demonstrated that among oligoanuric patients on maintenance hemodialysis, predialysis lower serum sodium levels were associated with a greater risk of mortality.Citation7 In these patients, serum sodium is determined by the relative intake of solute and free water during the interdialytic interval; excessive free water intake or reduced solute intake leads to lower predialysis serum sodium concentrations. In addition, the dialysate sodium concentration is typically 140 mEq/L in hemodialysis; patients with lower predialysis serum sodium concentration will experience an increase in serum sodium during each dialysis treatment, which may further drive thirst and cyclical changes in serum osmolality.Citation22 However, the mechanism(s) by which low serum sodium concentration may affect survival are not entirely clear till now.
However, in CPD patients, the baseline serum sodium level was not a predictor of mortality after multiple factors adjusted. Some reasons may account for the phenomenon. First, PD is a continuous treatment, not an intermittent treatment as HD. The effect of intradialytic free water intake on serum sodium compared with HD is minimal. Therefore, the cyclical alteration in serum sodium is fewer in PD than HD. Second, serum sodium level was associated with age and nutritional status in CPD patients. Although serum sodium was a negative predictor of two-year mortality in univariate cox regression analysis, after adjust to other important predictors, such as age, comorbidities and albumin, serum sodium was not an independent predictor of mortality in multivariate cox regression analysis. The finding reflected that serum sodium levels were affected by many other parameters in CPD patients.
This investigation had some limitations. First, the definite reasons of patients with lower sodium levels were not analyzed. Second, the amounts of sodium loss in the urine of patients with residual renal function were not calculated. However, urine volume or percentage of patients with anuria was not associated with serum sodium level in our study. Third, the sodium transport during PD was not further evaluated. Furthermore, the relationship of serum sodium level and sodium transport during PD was not clearly understood.
In conclusion, the study demonstrates that serum sodium level in CPD patients is associated with nutritional status, residual renal function and duration of PD. However, baseline serum sodium level is not an independent predictor of two-year mortality in CPD patients after adjusted other variables. Clinically, when we see a CPD patient with hyponatremia, we should pay more attention to the nutritional status and fluid status in the patient.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Hannon MJ, Thompson CJ. The syndrome of inappropriate antidiuretic hormone: Prevalence, causes and consequences. Eur J Endocrinol. 2010;162(Suppl 1):S5–S12
- Goldberg A, Hammerman H, Petcherski S, et al. Hyponatremia and long-term mortality in survivors of acute ST-elevation myocardial infarction. Arch Intern Med. 2006;166:781–786
- Klein L, O'Connor CM, Leimberger JD, et al. Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: Results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation. 2005;111:2454–2460
- Forfia PR, Mathai SC, Fisher MR, et al. Hyponatremia predicts right heart failure and poor survival in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2008;177:1364–1369
- Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122:857–865
- Sajadieh A, Binici Z, Mouridsen MR, et al. Mild hyponatremia carries a poor prognosis in community subjects. Am J Med. 2009;122:679–686
- Waikar SS, Curhan GC, Brunelli SM. Mortality associated with low serum sodium concentration in maintenance hemodialysis. Am J Med. 2011;124:77–84
- Nolph KD, Sorkin MI, Moore H. Autoregulation of sodium and potassium removal during continuous ambulatory peritoneal dialysis. Trans Am Soc Artif Intern Organs. 1980;26:334–338
- Kang SH, Cho KH, Park JW, Yoon KW, Do JY. Characteristics and clinical outcomes of hyponatraemia in peritoneal dialysis patients. Nephrology. 2013;18:132–137
- Dimitriadis C, Sekercioglu N, Pipili C, Oreopoulos DG, Bargman JM. Hyponatremia in peritoneal dialysis: Epidemiology in a single center and correlation with clinical and biochemical parameters. Perit Dial Int. 2014;34(3):260–270
- Chung SH, Lindholm B, Lee HB. Is malnutrition an independent predictor of mortality in peritoneal dialysis patients? Nephrol Dial Transplant. 2003;18:2134–2140
- Davies SJ, Phillips L, Naish PF, Russell GI. Quantifying comorbidity in peritoneal dialysis patients and its relationship to other predictors of survival. Nephrol Dial Transplant. 2002;17:1085–1092
- Zevallos G, Oreopoulos DG, Halperin ML. Hyponatremia in patients undergoing CAPD: Role of water gain and/or malnutrition. Perit Dial Int. 2001;21:72–76
- Lee CC, Chen KH, Tian YC, et al. Initial high peritoneal transport status is not a predictor of mortality in peritoneal dialysis patients. Ren Fail. 2010;32:788–795
- Brown EA, Davies SJ, Rutherford P, et al. Survival of functionally anuric patients on automated peritoneal dialysis: The European APD Outcome Study. J Am Soc Nephrol. 2003;14:2948–2957
- Paniagua R, Amato D, Mujais S, et al. Predictive value of brain natriuretic peptides in patients on peritoneal dialysis: Results from the ADEMEX trial. Clin J Am Soc Nephrol. 2008;3:407–415
- Goldberg A, Hammerman H, Petcherski S, et al. Prognostic importance of hyponatremia in acute ST-elevation myocardial infarction. Am J Med. 2004;117:242–248
- Jenq CC, Tsai MH, Tian YC, et al. Serum sodium predicts prognosis in critically ill cirrhotic patients. J Clin Gastroenterol. 2010;44:220–226
- Dzau VJ, Colucci WS, Hollenberg NK, Williams GH. Relation of the renin-angiotensin-aldosterone system to clinical state in congestive heart failure. Circulation. 1981;63:645–651
- Lilly LS, Dzau VJ, Williams GH, Rydstedt L, Hollenberg NK. Hyponatremia in congestive heart failure: Implications for neurohumoral activation and responses to orthostasis. J Clin Endocrinol Metab. 1984;59:924–930
- Mettauer B, Rouleau JL, Bichet D, et al. Sodium and water excretion abnormalities in congestive heart failure. Determinant factors and clinical implications. Ann Intern Med. 1986;105:161–167
- Santos SF, Peixoto AJ. Revisiting the dialysate sodium prescription as a tool for better blood pressure and interdialytic weight gain management in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3:522–530