Abstract
Objectives: To evaluate dry eye symptoms and clinical tear film alterations in patients with chronic renal failure (CRF). Materials and methods: Thirty-five non-diabetic CRF patients undergoing hemodialysis, and 31 healthy individuals were enrolled. An ocular surface disease index questionnaire (OSDI) was administered, and after a complete ocular examination, Schirmer and tear break-up time (TBUT) tests were performed. Results: OSDI scores were significantly higher (p < 0.01) and TBUT tests were significantly lower (p = 0.01) in CRF patients than in the control group. Schirmer test results were also lower in the CRF patients group, but lacked statistical significance (p = 0.20). Conclusion: Patients with CRF should be advised to obtain an ophthalmic examination, especially for dry eye.
Introduction
Chronic renal failure (CRF) of any etiology can induce eye disorders secondary to metabolic changes and hemodialysis treatment. Eye findings associated with chronic renal disease include conjunctival erythema, metastatic calcification on the ocular surface, conjunctival degenerations such as pinguecula, dry eye, band keratopathy, corneal endothelial impairments, uremic optic neuropathy, pseudotumor cerebri, uremic amaurosis, age-related macular degeneration (AMD) and cataracts.Citation1–11
Dry eye is a multifactorial disease of the ocular surface. It results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface.Citation12 A summary of the available data suggests that the prevalence of dry eye lies somewhere in the range of 5–30% in the population aged 50 years and older,Citation13 but the incidence of dry eye is increasing. Ellwein and colleagues found that the incidence of dry eye cases increased by 57.4% from 1991 to 1998.Citation14
The purpose of this study was to evaluate dry eye symptoms and clinical tear film alterations in patients with CRF undergoing hemodialysis.
Materials and methods
This study was prospective, case-controlled and comparative. All patients signed an informed consent form prior to enrollment. All procedures conformed to the tenets of the Declaration of Helsinki. The study was approved by the ethics committee of the Dışkapı Yıldırım Beyazıt Training and Research Hospital.
Non-diabetic end-stage CRF patients undergoing hemodialysis were enrolled in this study. The study group consisted of 35 CRF patients (35 eyes) and 31 healthy (31 eyes) individuals. Only the right eyes of the patients and the control group were taken into consideration for statistical analysis. Subjects previously diagnosed with dry eye were excluded from the study. Subjects who had any previous ocular-surface disorders or intraocular surgery, who had nasolacrimal duct obstruction, or who were using topical ophthalmic drugs and/or systemic medications were excluded from the study. Contact lens users were also excluded from the study. An ocular surface disease index (OSDI) questionnaire was administered to all subjects to assess the symptoms of dry eye before the ophthalmologic examination. This questionnaire has proved to be reliable for the assessment of dry eye symptoms.Citation18 After a complete ocular examination, including best-corrected visual acuity, slit-lamp and fundus examinations; Schirmer and tear break-up time (TBUT) tests were performed immediately prior to hemodialysis.
The Schirmer I test (without anesthesia) was performed to quantify aqueous tear production. In this test, a 35 × 5 mm filter paper strip was used to measure the quantity of tears produced over a period of 5 min. Five minutes after the Schirmer I test, the TBUT test was performed. Sterile strips of fluorescein were used for TBUT measurements. While the patients were looking upwards, the fluorescein paper was smoothly touched to the inferior fornix conjunctiva and then removed. The patients were directed to blink three times, and then look straightforward without blinking. The tear film was observed under the cobalt-blue filtered light of the slit-lamp biomicroscope, and the interval between the last blink and the appearance of the first dry spot in seconds was accepted as TBUT. Eyes with a Schirmer value of less than 10 mm and TBUT of less than 10 s were assessed to be a dry eye.
Statistical analysis
Statistical analyses were performed using the Statistical Package for Social Sciences (version 20.0, SPSS Inc., Chicago, IL). As the distribution of the data was non-normal, nonparametric tests were used in the analyses. The Kruskal–Wallis One-Way Analysis of Variance on Ranks Test was applied to determine the difference between the control and study eyes. The correlation analysis between the Schirmer and TBUT tests was performed by Spearman correlation analysis. p-Values of less than 0.05 were considered to be statistically significant.
Results
Demographic data of the study and control patients are given in . There were no significant differences between the patient and control groups in terms of age (p = 0.90), or gender (p = 0.22).
Table 1. Demographic data of the patients and control group.
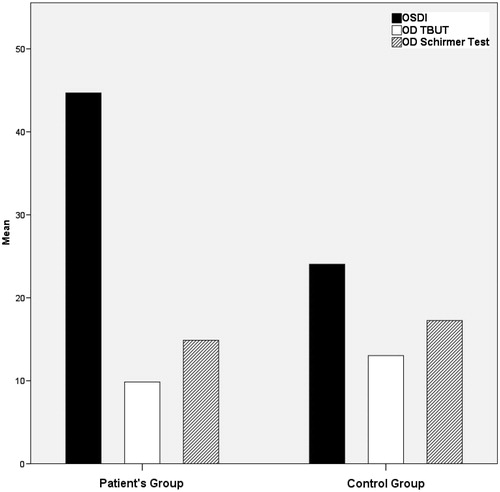
OSDI scores, TBUT and Schirmer test values in the control and study eyes are given in . OSDI scores were significantly (p < 0.01) higher in CRF patients than in the control group. A significant difference was observed for TBUT, which was shorter in patient’s group (p = 0.01). Schirmer test values were also lower in CRF patients but the difference was not statistically significant (p = 0.20). In the CRF group; 68.6% and 37.1% of the patients were diagnosed as having dry eye according to the TBUT and Schirmer results respectively. Whereas, when the cutoff OSDI score was accepted as ≥35, 77.1% of the CRF patients were diagnosed as having dry eye. In contrast, in the control group; 29%, 22.6% and 22.6% of the subjects were diagnosed as having dry eye according to the TBUT and Schirmer and OSDI results respectively ().
Table 2. OSDI, TBUT and Schirmer values in control and study eyes.
There was a statistically significant inverse correlation between the OSDI and TBUT scores (r = −0.271, p = 0.028). There was also a statistically significant positive correlation between the Schirmer and TBUT scores (r = 0.442, p < 0.001), whereas no significant correlation existed between the OSDI and Schirmer’s test scores.
Slit lamp examination revealed mild to moderate conjunctival hyperemia in 52 eyes (74.2%). Calcification of the conjunctiva was found in 33 eyes (47.1%), which was diffuse in 19 eyes (57.6%) and localized in 14 eyes (42.4%). Corneal calcification was not seen in any patient.
The mean duration of hemodialysis was 6.18 ± 6.13 years. The OSDI scores (r = 0.058, p = 0.739), TBUT (r = 0.102, p = 0.559) and Schirmer test values (r = −0.73, p = 0.76) were not associated (Spearman correlation analysis) with the duration of hemodialysis.
Discussion
The tear film is a complex and delicately balanced unit dependent on the normal function of several components.Citation15,Citation16 Both systemic and local disorders can affect these components of normal tear function, and hence cause dry eye. CRF is a systemic disorder characterized by alterations in kidney structure and function, which manifest in various ways depending upon the underlying cause and the severity of the disease.Citation17 Hormonal and metabolic changes, toxic conditions such as uremia, acute and chronic inflammatory reactions can cause various ocular disorders. Patients with CRF are generally treated using a blood filtration mechanism such as hemodialysis (HD), which can also cause some ocular impairments such as refractive changes, dry eye, increased tear osmolarity, conjunctival calcium deposits, band keratopathy, corneal endothelium changes, and lenticular opacity.Citation1,Citation11
According to the previous studies, long-term HD can cause changes in the tear film and ocular surface.Citation1,Citation18 An increased urea concentration in tears and decreased tear production after HD causes an increase in tear osmolarity. Hyperosmolarity stimulates inflammatory events in epithelial surface cells and the generation of inflammatory cytokines and matrix metalloproteinases (MMPs), which arise from or activate inflammatory cells at the ocular surface. This causes ocular surface damage, cell apoptosis, loss of goblet cells, reduced expression of mucins, and tear film instability.Citation19 According to our study, there was a discrepancy between OSDI scores and Schirmer's test results that shows the aqueous component of the tear. So, the conjunctival inflammation may be the reason for this discrepancy, since deterioration of OSDI score in CRF group may be due to ocular surface inflammation. Ozdemir et al. evaluated the relation between ocular surface disorders and tear function in patients with CRF.Citation20 They found that the abnormal TBUT test results and Rose Bengal staining were significantly more frequent in the patient group than in the control group. But the Schirmer’s test results were similar among the patient and control groups. Similar Schirmer’s test results were obtained in our study, which also demonstrated that there was no significant difference between the Schirmer’s test values of patient and control eyes (p = 0.20). Thus, ocular irritation symptoms in CRF patients undergoing HD treatment would not be related with aqueous insufficiency. Instead the main mechanism may be inflammation itself and tear film instability due to inflammatory process.
In a study by Aktaş et al. the ocular surface changes of 75 eyes of 38 CRF patients were reported. They found dry eye in 21.3% (according to Schirmer test) and 62.7% (according to TBUT) of eyes in patients with CRF.Citation21 According to our results, in the CRF group; 68.6% and 37.1% of the patients were diagnosed as having dry eye according to the TBUT and Schirmer results respectively. Whereas, when the cutoff OSDI score was accepted as ≥35, 77.1% of the CRF patients were diagnosed as having dry eye. In contrast, in the control group; 29%, 22.6% and 22.6% of the subjects were diagnosed as having dry eye according to the TBUT, Schirmer and OSDI results respectively. To the best of our knowledge, there is limited research on evaluation of OSDI in CRF patients undergoing hemodialysis, which is used to measure the impact of dry eye on quality of life. In the current study, we performed three tests for confirmation of the diagnosis. The OSDI questionnaire is a standardized instrument used to evaluate symptoms and can be easily performed and used to support the diagnosis of dry eye syndrome.Citation22,Citation23 This questionnaire was also validated for use in Turkey.Citation24 In our study, in both control and patient eyes, the OSDI results were well correlated with those of the TBUT. OSDI scores were significantly (p < 0.01) higher in CRF patients than in the control group. A significant difference was observed for TBUT, which was shorter in patient’s group (p = 0.01). But there was no difference between the groups according to the Schirmer’s test results. We think that the Schirmer test alone does not seem to be a good test for the diagnosis of dry eye, because reflex tearing can result in misdiagnosis of dry eye patients as normal.
Calcification of the conjunctiva, which is one of the most common complications of CRF, is a kind of metastatic calcification.Citation25 Inflammatory reaction, which is thought to be induced by conjunctival calcification, is reported to cause red eye.Citation26 The major anterior segment finding of the CRF patients in the present study was red eye (74.2%) with conjunctival calcification (47.1%). Aktaş et al. reported red eye with conjunctival calcification in 81.3% of the subjects. They also found a significant correlation between conjunctival calcification and both serum calcium and phosphate concentration.Citation21 In our study, conjunctival deposits may have been a reason for the decreased TBUT values and increased OSDI scores.
There are several limitations to this study. Due to the small sample size, these results are difficult to apply to all CRF patients being treated with HD. Total dialysis time may be an important factor for changes associated with the development of dry eyes. Relatively short HD duration in our study may be the reason of lack of a statistically significant difference between the Schirmer test values. Impression cytology is useful in assessing the inflammation of the ocular surface. The lack of it in the current study is another limitation.
In summary, the findings of this study showed that dry eye symptoms in CRF patients undergoing hemodialysis have influence on patient's daily life. We recommend that patients with CRF undergo ophthalmic examination, particularly for dry eye. Further studies may be necessary to increase our understanding and diagnosis of dry eye in patients with CRF.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Diaz-Couchoud P, Bordas FD, Garcia JRF, et al. Corneal disease in patients with chronic renal insufficiency undergoing hemodialysis. Cornea. 2001;20:695–702
- Grunwald JE, Alexander J, Maguire M, et al. Prevalence of ocular fundus pathology in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:867–873
- Hsiao CH, Chao A, Chu SY, et al. Association of severity of conjunctival and corneal calcification with all-cause 1-year mortality in maintenance haemodialysis patients. Nephrol Dial Transplant. 2011;26:1016–1023
- Tyler HR. Neurologic disorders seen in the uremic patient. Arch Intern Med. 1970;126:781–786
- Klaassen-Broekema N, van Bijsterveld OP. Diffuse and focal hyperaemia of the outer eye in patients with chronic renal failure. Int Ophthalmol. 1993;17:249–254
- Tokuyama T, Ikeda T, Sato K, et al. Conjunctival and corneal calcification and bone metabolism in hemodialysis patients. Am J Kidney Dis. 2002;39:291–296
- Knox DL, Hanneken AM, Hollows FC, et al. Uremic optic neuropathy. Arch Ophthalmol. 1988;106:50–54
- Servilla KS, Groggel GC. Anterior ischemic optic neuropathy as a complication of hemodialysis. Am J Kidney Dis. 1986;8:61–63
- Dursun D, Demirhan B, Oto S, Aydın P. Impression cytology of the conjunctival epithelium in patients with chronic renal failure. Br J Ophthalmol. 2000;84:225–227
- Laqua H. Cataract in chronic renal insufficiency and dialysis. Klin Monbl Augenheilkd. 1972;160:346–350
- Liew G, Mitchell P, Wong TY, et al. CKD increases the risk of age-related macular degeneration. J Am Soc Nephrol. 2008;19:806–811
- The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye Workshop (2007). Ocul Surf. 2007;5(2):75–92
- The epidemiology of dry eye disease: Report of the Epidemiology Subcommittee of the International Dry Eye Workshop (2007). Ocul Surf. 2007;5(2):93–107
- Ellwein LB, Urato CJ. Use of eye care and associated charges among the medicare population: 1991–1998. Arch Ophthalmol. 2002;120:804–811
- Rolando M, Zierhut M. The ocular surface and tear film and their dysfunction in dry eye disease. Surv Ophthalmol. 2001;45:203–210
- Tseng SC, Tsubota K. Important concepts for treating ocular surface and tear disorders. Am J Ophthalmol. 1997;124(6):825–835
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266
- Charlton JF, Schwab IR, Stuchell R. Tear hyperosmolarity in renal dialysis patients asymptomatic for dry eyes. Cornea. 1996;15:335–339
- Li DQ, Chen Z, Song XJ, Luo L, Pflugfelder SC. Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2004;45:4302–4311
- Ozdemir M, Bakaris S, Ozdemir G, et al. Ocular surface disorders and tear function changes in patients with chronic renal failure. Can J Ophthalmol. 2004;39:526–532
- Aktaş Z, Ozdek S, Asli Dinç U, et al. Alterations in ocular surface and corneal thickness in relation to metabolic control in patients with chronic renal failure. Nephrology. 2007;12:380–385
- Schiffman RM, Christianson MD, Jacobson G, et al. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118:615–621
- Özcura F, Aydin S, Helvacı MR. Ocular surface disease index for the diagnosis of dry eye syndrome. Ocul Immunol Inflamm. 2007;15:389–393
- Irkec M; Turkish OSDI Study Group. Reliability and validity of Turkish translation of the Ocular Surface Disease Index (OSDI) in dry eye syndrome. Invest Ophthalmol Vis Sci. 2007;48Abstract 408–B610
- Chestler RJ, De Venecia G. Calcific eyelid margin lesions in chronic renal failure. Am J Ophthalmol. 1989;107:556–557
- Klaassen-Broekema N, van Bijsterveld OP. Red eyes in renal failure. Br J Ophthalmol. 1992;76:268–271