Abstract
Background: Abnormalities of blood system often occur several days before acute kidney injury (AKI) in patients with heat stroke (HS). We aimed to investigate the prevalence and prognostic value of the early hematological markers in patients with AKI induced by HS. Methods: In a retrospective cohort study, we analyzed the case records of 176 patients with HS and evaluated the hematological markers for early prediction and risk classification in the patients with AKI. Results: Of 176, 103 (58%) HS cases developed AKI, and men comprised more than half (75%) of the sample population. The nadir platelet count significantly correlated with the levels of peak serum creatinine (r = −0.608, p < 0.01) and blood urea nitrogen (r = −0.546, p < 0.01), and the length of hospital stay (r = −0.393, p < 0.01). The areas under the receiver operating characteristic curves (AU-ROC) indicated the prognostic accuracy of hematological markers, AU-ROC was significantly higher with the nadir platelet count than that with the admission platelet count (AU-ROC of the nadir platelet: 0.73; 95% CI: 0.67–0.82; vs. AU-ROC of the admission platelet: 0.67; 95% CI: 0.59–0.75; p < 0.01). Multiple logistic regression results indicated that the nadir platelet count (adjusted ORs: 37.92; 95% CI: 2.18–87.21; p < 0.01) was independent predictor of AKI in HS. Conclusion: The high mortality observed in HS complicated with AKI, and among the various hematological parameters assessed, thrombocytopenia is associated with AKI induced by HS independently.
Introduction
Heat stroke (HS) is also called body hyperthermia syndrome, whose main feature is body temperature ≥39.0 °C, even up to 42.0 °C. Severe heat stroke is the main type that leads to death, which is acute onset, high disability and mortality rate. HS can be divided into classical HS and exertional HS, the former mainly occurs in the elderly or patients with basic disease; the latter mainly occurs in young, which is due to a lot of movement in the high temperature and humidity environment. The high temperature has wide effects on the body damage, not only cause the temperature regulation system disorder, but also affect other important organs, such as lung, brain, kidney, and blood.Citation1–3 Among the organs, acute kidney injury (AKI) is one of the most common complications of HS, which can rapidly develop into acute renal failure; the mortality rate is as high as 30–80%.Citation4,Citation5
At present, the treatment for the patients with AKI in HS is supportive care, including: control of the body temperature, the maintenance of water and electrolyte balance, and the organ function support. In patients with the end stage of AKI, hemodialysis is highly important for the prognosis. The clinical symptoms and laboratory examinations of AKI in HS were always used to classify,Citation6–8 such as oliguria, anuria, hematuria, proteinuria, blood serum creatinine, and urea nitrogen. However, thrombocytopenia is one index of early AKI but not to be found during AKI in HS.
HS is a highly dynamic process, which is characterized by a short transient thrombocytopenia followed by AKI.Citation9–11 In this study hematological markers and clinical parameters were collected from the hospitalized patients, and the relationship between the decrease in platelet counts and the severity and prognosis of HS complicated with AKI was analyzed. To date, no much related research was carried out.
Methods
Subjects
We retrospectively reviewed the case records of 176 patients with HS, diagnosed during the heat wave periods, from June to October between 2010 and 2014, in Ningbo First Hospital, Zhejiang Province. The clinical diagnosis criteria of HS includes: (1) sudden increase in environmental temperature (air temperature ≥ 35.0 °C), (2) the increase in body temperature above 39.0 °C, (3) a lot of sweat in early, then “no sweat”, which may be complicated with dry skin and different levels of consciousness, etc. Patients who conform to the diagnosis standard were included. Exclusion criteria included complications with other organs dysfunction, such as lung, heart, liver, pancreas, and other organs, or acute injury within 24 h of admission. This study was approved by the ethics committee of the Ningbo First Hospital. Informed consent was not required as it was a retrospective study and the data were analyzed anonymously.
Data collection
Clinical and laboratory data were obtained daily throughout hospitalization and were recorded on standardized data collection forms. It included HS courses, laboratory examinations (platelet counts, leukocyte counts, hematuria, proteinuria, serum creatinine, blood urea nitrogen, etc.), hemodialysis information, the length of hospital stay, and other severe complications. All subjects were admitted to the hospital and monitored daily until discharged. Hemodialysis treatment was guided by the ward physician based upon clinical necessity.
Statistical analysis
Continuous variables are presented as mean ± SD. They were compared by the Welch t test. Categorical and discrete variables are presented as numbers and percentages. When appropriate, they were compared by either the Fisher's exact test or the chi-square test. Spearman correlations and linear regression analyses were used to evaluate the relations between hematological markers and biochemical, or clinical parameters. ROC curves were constructed to assess the sensitivity and specificity of the platelet and leukocyte counts in predicting the development of AKI, and the areas under the ROC curves (AU-ROC) indicated the prognostic accuracy of hematological markers. Finally, multiple logistic regression models including sex, age, hematuria, and proteinuria were implemented to identify hematological markers associated with the development of AKI. All analyses were performed using Statistical Package for Social, version 18.0 (SPSS). A two-tail p value <0.05 was interpreted as significant.
Results
Baseline data of the patients
Of the 176 eligible patients from June to October between 2010 and 2014, 103 (58%) patients developed AKI. describes the baseline characteristics of study participants. Patients ranged in age from 19 to 76 years; the mean age for AKI group was 47.5 years and that of non-AKI group was 39.6 years. There were significant differences in age between these two groups of patients (p < 0.01). Men comprised more than half (77, 75%) of the sample population in the AKI group. The most common laboratory findings were thrombocytopenia and leukocytosis. Of all, 87 (85%) patients had platelet counts less than 100 × 109/L, and severe thrombocytopenia (≤30 × 109/L) in 56 (54%) cases. Of all, 96 (93%) patients had leukocytosis more than 10 × 109/L and 46 (45%) patients had severe leukocytosis (≥15 × 109/L). There were significant differences in thrombocytopenia and leukocytosis between these two groups of patients (p < 0.05). Moreover, the severe increase of blood serum creatinine (>450 µmol/L) was noted in 31 (30%) cases, and 23 (22%) patients received hemodialysis treatment, and they stay longer in hospital than patients who did not develop AKI.
Table 1. Characteristics of patients by AKI status.
Relationship between hematological markers and AKI
Thrombocytopenia is an early laboratory finding in patients with AKI induced by HS. The platelet counts reached their minimums within 7 ± 3 days after the acute onset of HS. However, the levels of serum creatinine and blood urea nitrogen reached the maximum within 10 ± 2 days and 8 ± 3 days, respectively. The nadir platelet count preceded the peak blood urea nitrogen and serum creatinine by 3 ± 2 days and 7 ± 2 days, respectively. The platelet counts often returned to normal in most patients after 10 ± 3 days. The leukocytosis reflected the degree and process of inflammation during HS, maximum often at the same time as thrombocytopenia ((7 ± 3) days).
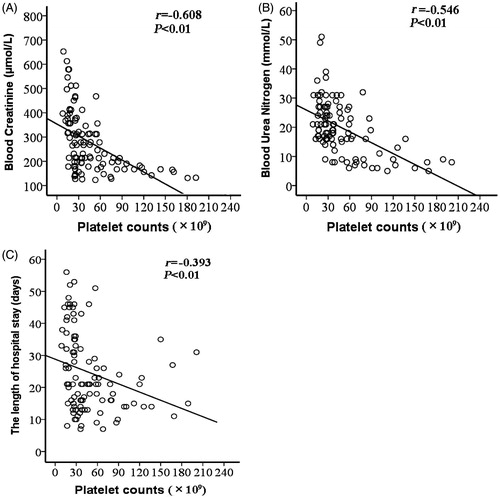
The nadir platelet count negatively correlated with the peak serum creatinine (r = −0.608, p < 0.01), the peak blood urea nitrogen (r = −0.546, p < 0.01), and the length of hospital stay (r = −0.393, p < 0.01) (). However, the peak leukocyte count correlated positively with the peak serum creatinine (r = 0.297, p < 0.01), the peak blood urea nitrogen (r = 0.239, p < 0.01), and the length of hospital stay (r = 0.196, p < 0.01).
Figure 1. Relationship between the nadir platelet counts and the peak blood creatinine (A), the peak blood urea nitrogen (B), and the lengths of hospital stay (C). The r denotes the Spearman correlation coefficient, and the line denotes the linear regression for each comparison.
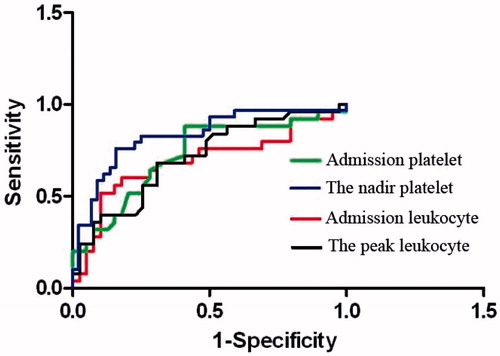
The admission and nadir platelet count were significantly lower in those patients who had AKI than the patients without AKI. Nevertheless, the admission and peak leukocyte count were significantly higher in the patients who had AKI than those without AKI. AU-ROC was significantly higher with the nadir platelet count than that with the admission platelet counts (AU-ROC of nadir platelet: 0.73; 95% CI: 0.67–0.82; vs. AU-ROC of admission platelet: 0.67; 95% CI: 0.59–0.75; p < 0.01) and was also significantly higher than that with the admission and peak leukocyte count (AU-ROC of admission leukocyte: 0.66; 95% CI: 0.61–0.72; and the peak leukocyte: 0.58; 95% CI: 0.54–0.62; p < 0.01) (). At a cut off value of 30 × 109/L, the sensitivity and specificity to predict AKI were 90% and 81% for the nadir platelet count, respectively ().
Table 2. The sensitivity and specificity were evaluated by the predictive values of AKI using different cut off values of platelet and leukocyte count (n = 103).
Multiple logistic regression results after adjusting gender, age, admission platelet counts, the nadir platelet counts, admission leukocyte counts, and peak leukocyte counts. The nadir of platelet counts (adjusted ORs: 37.92; 95% CI: 2.18–87.21; p < 0.01) and clinical hematuria (adjusted ORs: 6.79; 95% CI: 1.93–29.36; p < 0.01) were independent predictors of AKI in HS ().
Table 3. Multiple logistic regression to identify hematological markers and other clinical indicators associated with the development of AKI (n = 103).
Relationship between thrombocytopenia and prognosis
The patients who had thrombocytopenia during the early stage in hospital had more complications. Of 56 cases with the nadir platelet counts ≤30 × 109/L, 17 cases (30%) complicated with respiratory system disease including pulmonary infection, edema, acute respiratory distress or respiratory failure; 12 cases (21%) complicated with acute cardiovascular dysfunction; 3 cases (5%) complicated with acute liver injury; 9 cases (16%) had multiple organ failure. Of 103 patients, 23 cases (22%) received hemodialysis treatment, 20 (87%) from 23 cases had thrombocytopenia (15 cases with platelet counts ≤30 × 109/L); 19 cases (18%) died, 13 cases had the nadir platelet counts ≤30 × 109/L; however, the patients with normal platelet count did not die.
Discussion
The present study demonstrates that little is known about the prognostic importance of thrombocytopenia in patients with AKI in HS. However, in this study, approximately half of the patients (54%) had severe thrombocytopenia (platelet counts ≤ 30 × 109/L), which is identical with Peng et al.Citation12 Meanwhile, these patients also had a higher level of serum creatinine and blood urea nitrogen. We retrospectively studied the clinical processes of patients with HS throughout hospitalization, the patients sequentially developed thrombocytopenia, AKI, and leukocytosis. In these patients, the nadir platelet count inversely correlated with the peak serum creatinine, the peak blood urea nitrogen, and the length of hospital stay, which reflected the severity of renal dysfunction. Thrombocytopenia and leukocytosis in patients with HS were strongly associated with a substantially increased risk of development of AKI.
In this study, the nadir platelet counts, as well as the peak leukocyte counts, was found to be correlated with the clinical and laboratory parameters which reflected the severity of AKI (). Compared with the admission platelet counts, and the admission and peak leukocyte counts, the nadir platelet counts were most accurate for diagnosis of AKI (). The clinical presence of hematuria was another independent predictor for the development of AKI (). Thrombocytopenia is an important finding for development of AKI induced by HS. Several pathological and physiological mechanisms can explain the cause of thrombocytopenia in HS complicated with AKI;Citation13,Citation14 most scholars agree that the increase of platelet damage and coagulation abnormalities, the increase of pro-inflammatory cytokines in plasma, cell membrane disintegration, and a large number of biological toxin spillover are the main mechanisms.Citation15–17 However, the accuracy of mechanisms underlying thrombocytopenia in patients with severe diseases is still unknown.
Among those patients with AKI, timely hemodialysis treatment may reduce the complications and mortality.Citation18–20 The level of platelet counts indicates whether the patients need hemodialysis treatment. But we should alert the wide fluctuations in the level of platelet counts, despite the low of platelet counts in the early stage, it may increased rapidly in a short period of time. In addition to hemodialysis treatment, some other treatment measures are also needed including: add the plasma and platelet, control of body temperature, and the necessity of enteral nutrition support.
Some limitations in this study need to be emphasized. Firstly, it was a retrospective and descriptive study of AKI in HS over a period of five years. Also, we performed analyses that excluded participants with other organs dysfunction within 24 h of admission, so caution must be exercised in interpreting our data. Secondly, all cases in this study were collected from medical records, and diagnoses were based on the Heat Stroke Diagnostic Guide in the people's Republic of China (2002); therefore, it is not clear how our findings can be generalized to patients in different areas. Thirdly, it is a small cohort study, therefore, these markers require validation in independent cohorts. Furthermore, this study did not specifically compare the relationship between platelet decrease and hemodialysis, and the study cannot differentiate the peak serum creatinine and blood urea nitrogen between patients with and without hemodialysis treatment.
Conclusions
Thrombocytopenia was associated with the development and prognosis of AKI in HS. As the platelet count is a simple and easy available clinical test that is widely used in medical care, and thrombocytopenia is an early laboratory abnormality in HS complicated with AKI, which may bring a rule that evaluate the severity of AKI for timely hemodialysis treatment. We suggest that doctors should pay much attention to the changes of platelet counts and develop effective treatments according to different conditions of each patient.
Declaration of interest
The authors have no conflicts of interest to disclose.
References
- Lumlertgul D, Chuaychoo B, Thitiarchakul S, et al. Heat stroke-induced multiple organ failure. Ren Fail. 1992;14(1):77–80
- Deutsch M, Koskinas J, Emmanuel T, et al. Heatstroke and multi-organ failure with liver involvement in an asylum-seeking refugee. J Emerg Med. 2006;31(3):255–257
- McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ Health Perspect. 2001;109(Suppl. 2):185–189
- Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–1988
- Woodrow G, Brownjohn AM, Turney JH. The clinical and biochemical features of acute renal failure due to rhabdomyolysis. Ren Fail. 1995;17(4):467–474
- Junglee NA, Di Felice U, Dolci A, et al. Exercising in a hot environment with muscle damage: effects on acute kidney injury biomarkers and kidney function. Am J Physiol Renal Physiol. 2013;305(6):F813–820
- Raju SF, Robinson GH, Bower JD. The pathogenesis of acute renal failure in heat stroke. South Med J. 1973;66 (3): 330–333
- Semenza JC. Acute renal failure during heat waves. Am J Pre Med. 1999;17(1):97
- De Souza AL, Rodrigues C, Sztajnbok J, et al. Hypoelectrolytemia accompanied by acute renal failure in exertional heatstroke. Am J Emerg Med. 2006;24(7):888–889
- Yamashita S, Uchida Y, Kojima S, et al. Heatstroke in patients with Parkinson's disease. Neurol Sci. 2012;33(3):685–687
- Puz P, Lasek-Bal A, Ziaja D, et al. Inflammatory markers in patients with internal carotid artery stenosis. Arch Med Sci. 2013;9(2):254–260
- Peng Z, Pai P, Hong-Bao L, et al. The impacts of continuous veno-venous hemofiltration on plasma cytokines and monocyte human leukocyte antigen-DR expression in septic patients. Cytokine. 2010;50(2):186–191
- Lee KL, Niu KC, Lin MT, et al. Attenuating brain inflammation, ischemia, and oxidative damage by hyperbaric oxygen in diabetic rats after heat stroke. J Formos Med Assoc. 2013;112(8):454–462
- Michel V, Peinnequin A, Alonso A, et al. Effect of glucocorticoid depletion on heat-induced Hsp70, IL-1beta and TNF-alpha gene expression. Brain Res. 2007;1164:63–71
- Pozner RG, Ure AE, Jaquenod de Giusti C, et al. Junin virus infection of human hematopoietic progenitors impairs in vitro proplatelet formation and platelet release via a bystander effect involving type IIFN signaling. PLoS Pathog. 2010;6(4):e1000847
- Bouchama A. The 2003 European heat wave. Intensive Care Med. 2004;30(1):1–3
- Yu FC, Lu KC, Liu SH, et al. Energy metabolism in exertional heat stroke with acute renal failure. Nephrol Dial Transplant. 1997;12(10):2087–2092
- Ikeda Y, Sakemi T, Nishihara G, et al. Efficacy of blood purification therapy for heat stroke presenting rapid progress of multiple organ dysfunction syndrome: a comparison of five cases. Intensive Care Med. 1999;25(3):315–318
- Laine O, Makela S, Mustonen J, et al. Enhanced thrombin formation and fibrinolysis during acute Puumala hantavirus infection. Thromb Res. 2010;126(2):154–158
- Fan H, Zhao Y, Zhu JH, et al. Urine neutrophil gelatinase-associated lipocalin in septic patients with and without acute kidney injury. Ren Fail. 2014;36(9):1399–1403