Abstract
There is a close relationship between sleep disordered breathing (SDB) and heart failure. We performed home oxygen therapy (HOT) in patients with SAS undergoing dialysis, and investigated its effects on the heart function. The subjects were 10 SDB patients on dialysis. On retiring at night, oxygen was transnasally administered at 1.0 L/min. The human atrial natriuretic peptide (hANP), brain natriuretic peptide (BNP), total protein, Alb, cholesterol and phosphorus levels were measured before the start of oxygen therapy and after 6 weeks. The mean SpO2 increased from 93.5% [91.5, 97.0] to 96.3% [94.8, 97.4] (median [interquartile range]) (p = 0.015). The hANP (p = 0.0039), BNP (p = 0.0098) and serum Alb (p = 0.015) levels significantly improved. There were no significant changes in the cholesterol, phosphorus or total protein levels. These results suggest that nocturnal oxygen therapy improves indices of heart failure, contributing to the prevention and treatment of heart failure in dialysis patients with SDB.
Introduction
Tada et al.Citation1 and Kosmadakis and MedcalfCitation2 reported that the incidence of sleep disordered breathing (SDB) was high in patients undergoing dialysis. Unruh et al.Citation3 indicated that there was a strong association of HD with severe SDB and nocturnal hypoxemia independent of the age, BMI and higher prevalence of chronic disease.
Sasayama et al.Citation4 reported that the introduction of home oxygen therapy (HOT) improved the heart function in non-dialysis patients with SDB. Furthermore, Javaheri and WexlerCitation5 indicated that the treatment of sleep apnea, both obstructive and central, results in a decrease in sympathetic activity and an improvement in systolic function, which are known surrogates of mortality. However, no study has reported the effects of HOT for SDB on the heart function in dialysis patients. In this study, we performed HOT in dialysis patients with SDB, and examined its influence on the heart function.
Materials and methods
In patients undergoing maintenance dialysis in our hospital, SpO2 monitoring was conducted using a sleep apnea-testing system (Smart Watch PMP-300E, Pacific Medico, Tokyo, Japan).
In these subjects, overnight saturation monitoring was transcutaneously performed to examine the mean oxygen saturation and lowest arterial oxygen saturation. An oxygen desaturation index (ODI) was computed. Ten patients diagnosed with SAS, with a mean SpO2 of 95% or lower or a minimum SpO2 of 90% or lower, participated in this study (). Heart failure was evaluated according to the New York Heart Association functional classification (NYHA) 1–2 ().
Table 1. Baseline characteristics of 10 patients.
Table 2. Changes in parameters after nocturnal home oxygen therapy (HOT).
In these patients, HOT was introduced. Using a transnasal camera, oxygen was administered at 1 L/min. Oxygen administration was started before retiring, and completed on waking (6–9 h). After 6 weeks, the human atrial natriuretic peptide (hANP), brain natriuretic peptide (BNP), total protein, Alb, cholesterol and phosphorus levels were measured, and compared with those before the start of HOT. We collected samples after dialysis for hANP and BNP and before dialysis for other parameters. We measured hANP using CLEIA and BNP CLIA techniques. We performed chest X-ray after dialysis. For statistical analysis, Wilcoxon’s signed-rank sum test was used.
The protocol of this study was approved by the Human Ethics committee of Moriguchi Keijinkai Hospital. Informed consent was obtained from all patients prior to participation.
Results
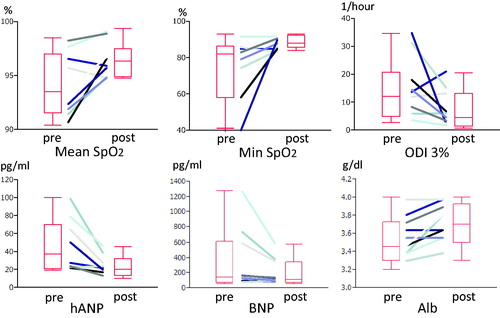
During the 6-week period, no patient required a change of dry weight (DW). HOT increased the mean SpO2 from 93.5% [91.5, 97.0] to 96.3% [94.8, 97.4] (median [interquartile range]) (p = 0.015). The minimum SpO2 significantly improved. The ODI (3%) also improved (). There were no changes in the NYHA classification and cardiothoracic ratio (CTR) ().
A blood biochemical test showed a significant increase in the serum albumin level and significant decreases in the hANP and BNP levels ().
There were no significant differences in the cholesterol, phosphorus or total protein levels ().
Discussion
Kasai reported that there was a close relationship between SDB and heart failure.Citation6 According to Bordier, SDB is observed in 50% of patients with chronic heart failure.Citation7
In patients with SDB, HOT may prevent hypoxemia related to central sleep apnea by increasing the inhaled oxygen concentration and improving the intra-alveolar oxygen reserve.Citation8,Citation9 As a result, it may reduce sleep apnea through an improvement in peripheral tissue oxygen supply, the suppression of sympathetic activities and a reduction in ventricular loading. In Japan, the results of nocturnal oxygen therapy in chronic heart failure patients with SDB have been published. In the oxygen-treated group, the apnea hypopnea index (AHI) was significantly lower than in the control group.Citation8 HOT is advantageous in correcting the elevated sympathetic activities, decreasing the frequency of sleep apnea and improving the sleep structure/symptoms. The enhancement of appetite related to an improvement in daytime activity through these actionsCitation10 may have contributed to the increase in the albumin level.
BNP and hANP are useful as indices of heart failure.Citation11–13 BNP may also be a prognostic factor for cardiovascular mortality in dialysis patients. Zoccaliet al.Citation14 indicated that BNP was a prognostic factor for total and cardiovascular mortality, independent of the left ventricular mass (LVM) and ejection fraction. Goto et al.Citation15 reported that the elevated levels of BNP indicated an increased risk of cardiac events. Zoccali et al.Citation16,Citation17 emphasized that SDB promoted left ventricular hypertrophy in dialysis patients, being a cardiovascular risk factor. Therefore, it is important to decrease the levels of BNP and hANP in dialysis patients.
Several studies have reported the influence of oxygen therapy on BNP and hANP in non-dialysis heart failure patients with SDB. Svatikova et al.Citation18 performed CPAP and overnight monitoring in patients with OSAS, and reported that there was a significant decrease in the hANP level, although there were no changes in the BNP level. Shigemitsu et al.Citation19 administered oxygen to patients with chronic heart failure at night for 4 months, and indicated that there was a significant decrease in the BNP level, whereas there were no significant changes in the hANP level. They concluded that oxygen administration prevented the progression of heart failure.
In our study, HOT decreased the BNP and hANP levels even in dialysis patients. HOT for SDB in dialysis patients may prevent the progression of heart failure.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Tada T, Kusano KF, Ogawa A, et al. The predictors of central and obstructive sleep apnoea in hemodialysis patients. Nephrol Dial Transplant. 2007;22:1190–1197
- Kosmadakis GC, Medcalf JF. Sleep disorders in dialysis patients. Int J Artif Organs. 2008;31:919–927
- Unruh ML, Sanders MH, Redline S, et al. Sleep apnea in patients on conventional thrice-weekly hemodialysis: Comparison with matched controls from the Sleep Heart Health Study. J Am Soc Nephrol. 2006;17(12):3503–3509
- Sasayama S, Izumi T, Matsuzaki M, et al.; CHF-HOT Study Group. Improvement of quality of life with nocturnal oxygen therapy in heart failure patients with central sleep apnea. Circ J. 2009;73:1255–1262
- Javaheri S, Wexler L. Prevalence and treatment of breathing disorders during sleep in patients with heart failure. Curr Treat Options Cardiovasc Med. 2005;7(4):295–306
- Kasai T. Sleep apnea and heart failure. J Cardiol. 2012;60(2):78–85
- Bordier P. Sleep apnoea in patients with heart failure. Part I: Diagnosis, definitions, prevalence, pathophysiology and hemodynamic consequences. Arch Cardiovasc Dis. 2009;102:651–661
- Toyama T, Seki R, Kasama S, et al. Effectiveness of nocturnal home oxygen therapy to improve exercise capacity, cardiac function and cardiac sympathetic nerve activity in patients with chronic heart failure and central sleep apnea. Circ J. 2009;73:299–304
- Sasayama S, Izumi T, Seino Y, Ueshima K, Asanoi H; CHF-HOT Study Group. Effects of nocturnal oxygen therapy on outcome measures in patients with chronic heart failure and Cheyne–Stokes respiration. Circ J. 2006;70:1–7
- Sasayama S, Izumi T, Matsuzaki M, et al.; CHF-HOT Study Group. Improvement of quality of life with nocturnal oxygen therapy in heart failure patients with central sleep apnea. Circ J. 2009;73:1255–1262
- Tan LB, Cooke A. Measurement of plasma brain natriuretic peptide in heart failure. Lancet. 1994;343(8901):858
- Bettencourt P, Ferreira A, Dias P, Castro A, Martins L, Cerqueira-Gomes M. Evaluation of brain natriuretic peptide in the diagnosis of heart failure. Cardiology. 2000;93(1–2):19–25
- Hartter E, Weissel M, Stummvoll HK, Woloszczuk W, Punzengruber C, Ludvik B. Atrial natriuretic peptide concentrations in blood from right atrium in patient with severe right heart failure. Lancet. 1985;2(8446):93–94
- Zoccali C, Mallamaci F, Benedetto FA, et al.; Creed Investigators. Cardiac natriuretic peptides are related to left ventricular mass and function and predict mortality in dialysis patients. J Am Soc Nephrol. 2001;12(7):1508–1515
- Goto T, Takase H, Toriyama T, et al. Increased circulating levels of natriuretic peptides predict future cardiac event in patients with chronic hemodialysis. Nephron. 2002;92:610–615
- Zoccali C, Benedetto FA, Mallamaci F, et al. Left ventricular hypertrophy and nocturnal hypoxemia in hemodialysis patients. J Hypertens. 2001;19:287–293
- Zoccali C, Benedetto FA, Tripepi G, et al. Nocturnal hypoxemia, night–day arterial pressure changes and left ventricular geometry in dialysis patients. Kidney Int. 1998;53:1078–1084
- Svatikova A, Shamsuzzaman AS, Wolk R, Phillips BG, Olson LJ, Somers VK. Plasma brain natriuretic peptide in obstructive sleep apnea. Am J Cardiol. 2004;94:529–532
- Shigemitsu M, Nishio K, Kusuyama T, Itoh S, Konno N, Katagiri T. Nocturnal oxygen therapy prevents progress of congestive heart failure with central sleep apnea. Int J Cardiol. 2007;115:354–360