Abstract
Background: Acute heart failure (HF) syndromes are frequently complicated with cardiorenal syndromes. The aim of this study was to evaluate the performance of admission neutrophil gelatinase associated lipocalin (NGAL) levels to predict diuretic dose requirement and to predict the occurrence of acute kidney injury (AKI) in patients presenting with acute decompensated HF. Methods: Patients admitted with HF symptoms between December 2010 and October 2011 were prospectively enrolled. Samples were obtained for NGAL and brain natriuretic peptide. Patients were followed up until discharge or for three days, whichever happened first. They were grouped either to have AKI according to “Acute Kidney Injury Network” criteria or not (“no-AKI”). Results: One hundred patients were enrolled. Urine NGAL levels were higher in AKI group (median 31.3 vs. 16.2 ng/mL) (p < 0.001). Oral furosemide using rates on admission was 60.5% in AKI group, 31.6% in no-AKI group. More AKI developed in patients using less furosemide orally on admission (p = 0.023). Although the mean furosemide doses were similar on the first day (80 mg), diuretic dose increment was less on the following days in AKI group. Urine NGAL levels with 12 ng/mL cut-off value had sensitivity of 79% and specificity of 67% for predicting AKI. Multiple logistic regression analysis yielded an odds ratio of 10.9 for NGAL levels to predict AKI. Conclusion: Urine NGAL level in decompensated HF patients was not a significant predictor of diuretic dose requirement, but was a good marker for predicting AKI at 12 ng/mL cut-off value.
Introduction
Although heart failure (HF) is a chronic disease, most patients with HF experience acute attacks of decompensation, namely acute heart failure syndromes (AHFS).Citation1 Cardiorenal syndromes (CRSs) may complicate the AHFS when acute kidney injury (AKI) ensues resulting in an increased rate of mortality, complications and length of hospital stay.Citation2,Citation3 Renal function may improve after diuretic treatment in some of the patients with AHFS as with the regressing congestion.Citation4
Neutrophil gelatinase associated lipocalin (NGAL) is one of the promising markers that can assist in early recognition of AKI.Citation5,Citation6 It can be measured in plasma and urine. Urine NGAL can be advantageous and easier to measure since it is easily obtained, stable, specific and not affected from urine neutrophils. Hypovolemia and diuretics do not affect the levels of urinary NGAL, thus can be used to differentiate AKI and prerenal azotemia.Citation7 In stable HF patients, it was shown that decreases in GFR and increases in N-terminal probrain natriuretic peptide (NT-proBNP) were associated with elevations in NGAL.Citation8 The pathophysiological association between HF and declining renal functions can evolve into a more complex situation in patients receiving diuretics. Diuretics are generally used on the basis of clinical guidance, but usually without a guidance of a laboratory parameter. NGAL is thought to be the missing link in the triangle of kidney–heart–inflammation, so it might be used as an early marker to develop algorithms that will guide diuretic treatment for patients with AHFS who are at risk of AKI.Citation9
The primary aim of this study was to evaluate the performance of urine NGAL in predicting the occurrence of AKI in AHFS patients. The secondary aim was to test the hypothesis that urine NGAL at admission could predict the dose of intravenous furosemide required to relieve the symptoms of AHFS.
Material and methods
Study population
Adult patients who were admitted to the emergency room of a University Hospital with acute decompensated HF between December 2010 and October 2011, and who consented were prospectively enrolled. This study was approved by Institutional Ethics Board and supported by the Turkish Society of Hypertension and Renal Diseases and Hacettepe University Scientific Research Support Fund.
Acute HF was diagnosed clinically. Congestive HF signs and symptoms (dyspnea, orthopnea, paroxysmal nocturnal dyspnea, decreased exercise capacity) and hypervolemia signs (rales, jugular venous distension, peripheral edema) on physical examination were evaluated as well as the underlying chronic conditions and the acute conditions that might have led to the decompensation of the chronic heart disease.
Patients with chronic renal replacement treatment, congenital heart disease, contrast nephropathy and urinary infection were excluded. Demographic characteristics, chronic diseases, medications, complaints and physical findings, NYHA functional class, laboratory tests and imaging results were recorded for the first three days of admission when available. Patients were followed up until death or discharge from the hospital to determine the length of hospital stay and the mortality rate.
Laboratory assessment
Serum BNP levels were routinely ordered in patients with dyspnea and presumptive or confirmed diagnosis of HF in the emergency room. Urine samples for NGAL were obtained on admission. Urine samples were centrifuged at 1500 rpm for 15 min, and were kept until they were collectively analyzed. Physicians taking care of the study patients were not informed about the results of NGAL and there was no intervention to the treatment protocol.
Plasma BNP was determined by using microparticle enzyme immunoassay method with AxSym device (AxSym System BNP Reagent Pack, Abbott Laboratories, Abbott Park, IL). Values > 100 pg/mL were accepted as positive.
Urine NGAL was determined by using Enzyme-Linked Immuno Sorbent Assay (ELISA) kit (BioVendor Research and Diagnostic Products, Modrice, Czech Republic) with Sirio ELISA reader (Seac, Radim, Italy).
Definitions
For AKI definition, “Acute Kidney Injury Network” (AKIN) criteria were used.Citation10 The difference between the highest creatinine in 48–72 h of admission and basal creatinine was calculated. Creatinine difference ≥ 0.3 mg/dL was defined as AKI. Chronic kidney disease was defined as permanent and steady kidney disease for at least three months (estimated GFR (eGFR) < 60 mL/min and creatinine variability < 25%). Glomerular filtration rate was calculated using the eGFR using modification of diet in renal disease formula (eGFR = 186 × serum creatinine−1.154 × Age−0.203 × [1.210 if black] × [0.742 if female]). For patients who did not have previous serum creatinine values, stable low eGFR values during hospital stay were considered as chronic kidney disease.
Statistical analysis
Data were entered to Statistical Package for the Social Sciences (SPSS)-15 program (Chicago, IL). Means, standard deviations and parametric tests were used when data were normally distributed, medians and non-parametric tests were used if the data were not normally distributed. The relationship between patients' outcomes and NGAL values was evaluated using logistic regression analysis to control for confounding factors. Cut-off value for urinary NGAL was defined by using receiver operating characteristic (ROC) analysis. The relationship between BNP levels and congestive HF was evaluated with Pearson chi-square and Fisher's exact tests. p-Value < 0.05 was defined as statistically significant.
Results
One hundred patients were enrolled in the study. Mean age of the patients was 70.9 ± 12.0 and 49% of them were male (). Most frequent admission complaint was dyspnea (92%) and hypertension was the most prevalent chronic disease (81%). Fifty-five percent of the patients were using per oral furosemide on admission. There were no differences between the AKI and non-AKI groups in terms of admission median systolic blood pressure (135 vs. 130 mmHg), median diastolic blood pressure (70 vs. 80 mmHg) and median serum sodium concentration (135 vs. 136 mEq/L), respectively.
Table 1. Demographic characteristics, known chronic diseases and drug usage for AKI and no AKI groups at the time of admission.
AKI developed in 19% of the patients during the first 72 h of the follow-up. Fourteen patients with AKI (73.7%) had an increase of more than 0.3 g/dL in creatinine, while the rest (26.3%) had a decrease in this period. On the other hand, among patients who were in the non-AKI group, 11 patients (13.6%) had some decrease in creatinine but not as much as 0.3 g/dL. The median serum creatinine level of the patients with AKI was 1.56 g/dL on admission, while of the patients in the non-AKI group was 1.01 g/dL.
There was no statistically significant age and gender difference between the patients who developed AKI and who did not. However, patients with AKI had a higher prevalence of underlying chronic kidney disease and lower percentage of per oral furosemide use before admission (). Community acquired pneumonia was the most common additional comorbidity (25%) in the study cohort. Thirty-five percent of the patients had NYHA class 2, 40% had class 3 and 20% of the patients had class 4 HF. There was no difference between classes with regard to the development of AKI in univariate analysis.
The mean length of hospital stay was 7.4 ± 10.7 days. The length of stay in the hospital was statistically significant for patients who developed AKI when compared to patients who did not develop AKI (). Hospital mortality was higher among patients with AKI when compared to patients without AKI ().
Table 2. Length of stay and outcome.
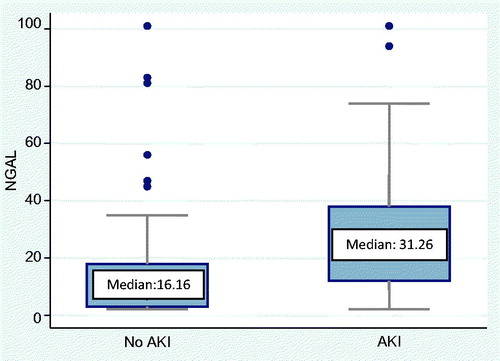
Plasma BNP levels were statistically higher in AKI group when compared to those patients without AKI (2118 ± 1130 vs. 1379 ± 1216 pg/mL, respectively; p = 0.009), so were the urine NGAL levels: median urine NGAL level was 31.2 ng/mL in the AKI group and 16.2 ng/mL in non-AKI group (p < 0.001) (). Median urine NGAL levels were also higher in patients with underlying chronic kidney disease when compared to those without a history of chronic kidney disease (17.7 vs. 5.5 ng/mL, respectively, p = 0.021).
Figure 1. Distribution of urine NGAL (ng/mL) levels and the median NGAL (ng/mL) levels in AKI and no AKI groups. NGAL, neutrophil gelatinase associated lipocalin; AKI, acute kidney injury.
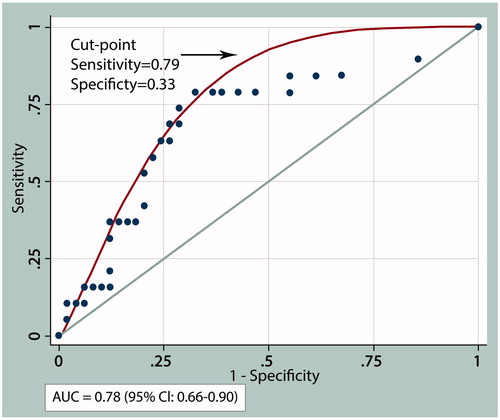
The ROC curve obtained by plotting urine NGAL and AKI frequency yielded an area under the curve (AUC) of 0.7789 (95% CI: 0.66–0.90) (). A cut-off value of ≥ 12 ng/mL for NGAL showed a sensitivity of 79%, specificity of 67% for predicting AKI. On univariate logistic regression analysis, cut-off value of urine NGAL≥12 ng/mL had an odds ratio of 8.9 for the development of AKI.
Figure 2. ROC analysis for urine NGAL (ng/mL) levels with regard to presence or absence of AKI. NGAL, neutrophil gelatinase associated lipocalin; AKI, acute kidney injury.
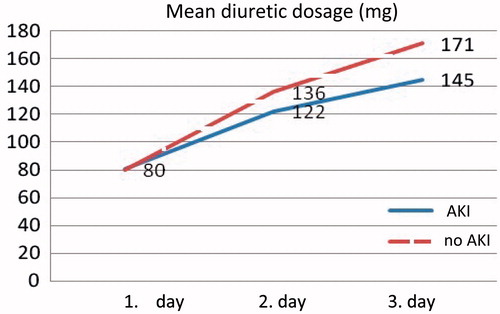
Although the mean intravenous furosemide doses on the first day were similar between groups (80 mg), diuretic dose increment was less on the following days in AKI group (). Patients in AKI and no AKI groups were divided into two subgroups according to the first day diuretic doses (as 80 mg or less, and more than 80 mg). When parameters as first day diuretic dose, age, gender, NYHA class, presence of chronic diseases such as diabetes mellitus and chronic kidney disease, and presence of pneumonia were introduced to a multiple logistic regression analysis, odds ratio of urine NGAL levels in predicting AKI was found to be 10.9.
Figure 3. Mean intravenous furosemide doses at the first, second and third day of hospitalization for AKI and no AKI groups. AKI, acute kidney injury.
Patients who died had higher NGAL levels when compared to those who were discharged, but the results were not statistically significant (11.5 vs. 7 ng/mL, respectively) (p = 0.17). On the other hand, mean BNP levels were significantly higher for patients who died (2232 ± 1512 pg/mL) when compared to those who were discharged (1404 ± 1147 pg/mL) (p = 0.047). Urine NGAL levels did not predict mortality (p = 0.17), while BNP levels had statistically significant association with mortality (p = 0.047).
Discussion
In this cohort of acute decompensated HF patients in the emergency room, the incidence of AKI was 19%. Urine NGAL at a cut-off level of 12 ng/mL had a positive predictive value of 85% and a negative predictive value of 58% to predict AKI. Moreover, multiple logistic regression analysis revealed an odds ratio of 10.9 for NGAL in predicting AKI.
Acute HF syndromes can be complicated with CRSs and AKI frequently develops in acute and critical patients.Citation11 Renal dysfunction during HF is a bad prognostic sign, so early recognition of AKI and appropriate management are very important.Citation2,Citation3 Heterogeneous studies yielded AKI prevalences between 20% and 60% on admission, reaching to 70% when all hospitalization period is taken into account.Citation12–15 Sensitive and early markers of AKI might be used to develop algorithms that will guide the management of these patients. One of the promising markers is NGAL, which has been shown to increase before the serum creatinine increment after a renal insult.Citation16–18
The diagnostic and prognostic value of NGAL in different patient groups yielded heterogeneous results in previous studies. Urine NGAL was found to be an early prognostic marker in HF patients with normal GFR levels.Citation19,Citation20 Though, a few studies question the role of NGAL in predicting the risk of AKI, serum NGAL was used as a marker for AKI, and it was also shown to be associated with a higher risk of AKI at different cut-off levels.Citation21,Citation22 Acute decompensated HF patients with serum NGAL levels over 167.5 ng/mL had 2.7 times increased mortality and 2.9 times increased hospitalization rates.Citation23 Alvelos et al. defined a cut-off value of 170 ng/mL for serum NGAL to foresee type 1 CRS with 100% sensitivity and 86.7% specificity (AUC was 0.93). Only the admission NGAL measurement in acute decompensated HF was important to foresee AKI.Citation24 Hospitalized acute decompensated HF patients might have high admission serum NGAL levels despite normal admission creatinine values.Citation22 Serum and urine NGAL levels were found to be important to foresee disease progression in chronic kidney disease patients.Citation25 Higher NGAL levels were also associated with NYHA functional class, acute decompensation, systolic blood pressure, ejection fraction and mortality and proposed as a marker for cardiovascular risk classification.Citation26,Citation27 Urine NGAL levels in HF patients were also positively correlated with NT-proBNP levels.Citation28 The superiority of NGAL when compared to other biomarkers is, its levels do not change with i.v. diuretic therapy.Citation29
There is not a well-accepted cut-off value for urine NGAL. In this cohort of patients, urine NGAL had highest positive predictive value to foresee AKI at a cut-off value of 12 ng/mL. On single logistic regression analyses, urine NGAL ≥ 12 ng/mL cut-off value had an odds ratio of 8.9, multiple logistic regression analysis odds ratio of NGAL levels in predicting AKI was found to be 10.9. Several studies in the literature suggest cut-off values ranging between 25 and 353.5 ng/mL.Citation30,Citation31
In daily practice, furosemide might be withheld in patients with increasing creatinine levels, yet the mechanism might be increasing congestion of the kidneys and the increased requirement for diuretic treatment in the context of type 2 CRS. Although first day mean i.v. furosemide doses were similar between groups (80 mg), diuretic dose increment was less on the following days in AKI group. This may be due to giving less diuretics after noticing increasing creatinine values not to deteriorate renal functions more or these patients developed more AKI due to less diuretic doses due to congestion. Although we could not demonstrate an association between the NGAL level and the diuretic dose requirement, this may be demonstrated in larger patient populations.
The study has some limitations. First, the sample size was relatively small. Second, we could not confirm the diagnosis of acute decompensated HF with echocardiographic measurements. However, the strength of the study was its real-life setting, very few exclusion criteria and the prospective nature.
Conclusion
One-fifth of patients in this real-life cohort of acute decompensated HF patients developed AKI in the first 72 h and urine NGAL was a valuable biomarker to predict the development of AKI.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Weintraub NL, Collins SP, Pang PS, et al. Acute heart failure syndromes: Emergency department presentation, treatment, and disposition: Current approaches and future aims: A scientific statement from the American Heart Association. Circulation. 2010;122(19):1975–1996
- Hata N, Yokoyama S, Shinada T, et al. Acute kidney injury and outcomes in acute decompensated heart failure: Evaluation of the RIFLE criteria in an acutely ill heart failure population. Eur J Heart Fail. 2010;12(1):32–37
- Damman K, Jaarsma T, Voors AA, Navis G, Hillege HL, van Veldhuisen DJ. Both in- and out-hospital worsening of renal function predict outcome in patients with heart failure: Results from the Coordinating Study Evaluating Outcome of Advising and Counseling in Heart Failure (COACH). Eur J Heart Fail. 2009;11(9):847–854
- Felker GM, O'Connor CM, Braunwald E. Loop diuretics in acute decompensated heart failure: Necessary? Evil? A necessary evil? Circ Heart Fail. 2009;2(1):56–62
- Cruz DN, de Cal M, Garzotto F, et al. Plasma neutrophil gelatinase-associated lipocalin is an early biomarker for acute kidney injury in an adult ICU population. Intensive Care Med. 2010;36(3): 444–451
- Ronco C. N-GAL: Diagnosing AKI as soon as possible. Crit Care. 2007;11(6):173
- Nickolas TL, O'Rourke MJ, Yang J, et al. Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Ann Intern Med. 2008;148(11):810–819
- Yndestad A, Landro L, Ueland T, et al. Increased systemic and myocardial expression of neutrophil gelatinase-associated lipocalin in clinical and experimental heart failure. Eur Heart J. 2009;30(10):1229–1236
- Di Somma S, Gori CS, Salvatori E. How to manage cardiorenal syndromes in the emergency room. Contrib Nephrol. 2010;165:93–100
- Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31
- Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52(19): 1527–1539
- Forman DE, Butler J, Wang Y, et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43(1):61–67
- Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: A report from the ADHERE database. J Card Fail. 2007;13(6):422–430
- Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and outcomes in heart failure: Systematic review and meta-analysis. J Am Coll Cardiol. 2006;47(10):1987–1996
- Adams KF Jr, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: Rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005;149(2):209–216
- Supavekin S, Zhang W, Kucherlapati R, Kaskel FJ, Moore LC, Devarajan P. Differential gene expression following early renal ischemia/reperfusion. Kidney Int. 2003;63(5):1714–1724
- Devarajan P. Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol. 2006;17(6):1503–1520
- Hewitt SM, Dear J, Star RA. Discovery of protein biomarkers for renal diseases. J Am Soc Nephrol. 2004;15(7):1677–1689
- Damman K, Masson S, Hillege HL, et al. Clinical outcome of renal tubular damage in chronic heart failure. Eur Heart J. 2011;32(21):2705–2712
- Poniatowski B, Malyszko J, Bachorzewska-Gajewska H, Malyszko JS, Dobrzycki S. Serum neutrophil gelatinase-associated lipocalin as a marker of renal function in patients with chronic heart failure and coronary artery disease. Kidney Blood Press Res. 2009;32(2):77–80
- Koca F, Tanboga IH, Can MM, et al. Neutrophil gelatinase-associated lipocalin levels in right and left heart failure: An observational study. Anadolu Kardiyol Derg. 2011;11(6):498–503
- Aghel A, Shrestha K, Mullens W, Borowski A, Tang WH. Serum neutrophil gelatinase-associated lipocalin (NGAL) in predicting worsening renal function in acute decompensated heart failure. J Card Fail. 2010;16(1): 49–54
- Alvelos M, Lourenco P, Dias C, et al. Prognostic value of neutrophil gelatinase-associated lipocalin in acute heart failure. Int J Cardiol. 2011;165:51–55
- Alvelos M, Pimentel R, Pinho E, et al. Neutrophil gelatinase-associated lipocalin in the diagnosis of type 1 cardio-renal syndrome in the general ward. Clin J Am Soc Nephrol. 2011;6(3):476–481
- Bolignano D, Lacquaniti A, Coppolino G, et al. Neutrophil gelatinase-associated lipocalin (NGAL) and progression of chronic kidney disease. Clin J Am Soc Nephrol. 2009;4(2):337–344
- Bolignano D, Basile G, Parisi P, Coppolino G, Nicocia G, Buemi M. Increased plasma neutrophil gelatinase-associated lipocalin levels predict mortality in elderly patients with chronic heart failure. Rejuvenation Res. 2009;12(1):7–14
- Shrestha K, Borowski AG, Troughton RW, Thomas JD, Klein AL, Tang WH. Renal dysfunction is a stronger determinant of systemic neutrophil gelatinase-associated lipocalin levels than myocardial dysfunction in systolic heart failure. J Card Fail. 2011;17(6):472–478
- Damman K, van Veldhuisen DJ, Navis G, Voors AA, Hillege HL. Urinary neutrophil gelatinase associated lipocalin (NGAL), a marker of tubular damage, is increased in patients with chronic heart failure. Eur J Heart Fail. 2008;10(10):997–1000
- Damman K, Ng Kam Chuen MJ, MacFadyen RJ, et al. Volume status and diuretic therapy in systolic heart failure and the detection of early abnormalities in renal and tubular function. J Am Coll Cardiol. 2011;57(22):2233–2241
- Makris K, Markou N, Evodia E, et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) as an early marker of acute kidney injury in critically ill multiple trauma patients. Clin Chem Lab Med. 2009;47(1):79–82
- Perry TE, Muehlschlegel JD, Liu KY, et al. Plasma neutrophil gelatinase-associated lipocalin and acute postoperative kidney injury in adult cardiac surgical patients. Anesth Analg. 2010;110(6):1541–1547

