Abstract
Hemodialysis catheters remain necessary for long-term vascular access in patients for whom arteriovenous access may be problematic or impossible. Developments in catheter design have improved long-term catheter functionality, and reduced the rate of infection and complications associated with their use. This retrospective study of 284 cases of chronic catheterization in 271 patients treated between 2009 and 2011 using Tal Palindrome™ symmetrical-tip (N = 118) or Quinton™ Permcath™ step-tip (N = 166) hemodialysis catheters evaluates the efficacy and the safety of symmetrical-tip dialysis catheters for chronic hemodialysis, compared with a step-tip catheter. Measurements of catheter performance included mean catheter dwell time, incidence of low blood flow, and rates of infection and catheter-related blood stream infection (CRBSI). The symmetrical-tip catheter had a significantly longer mean dwell time compared with the step-tip catheter; 329.4 ± 38.1 versus 273.1 ± 25.4 d (p < 0.05). In addition, the rate of occurrence of low blood flow per 1000 catheter days was lower for the symmetrical-tip compared with the step-tip catheter; 1.13 versus 6.86 (p < 0.01). The symmetrical-tip catheter was also associated with a lower incidence of complications; the rates of infection (0.28 vs. 0.78; p < 0.01) and CRBSI (0.15 vs. 0.44; p < 0.01) were lower compared with those for step-tip catheters, and catheter removal occurred less often for the symmetrical-tip catheter (8% vs. 16%; p < 0.05). The symmetrical-tip hemodialysis catheter was associated with a longer mean dwell time, lower incidence of low blood flow, and lower infection rate compared with the step-tip catheter.
Introduction
Autogenous arteriovenous (AV) fistula are the preferred method of vascular access for patients requiring chronic hemodialysis.Citation1,Citation2 However, despite various guidelines and initiatives supporting a reduction in hemodialysis catheter use, data from the USA indicate that nearly 80% of hemodialysis patients initiate treatment with a catheter, and catheter use is continued in 52% of patients after 4 months of treatment.Citation3–5
Although hemodialysis catheters are associated with significant mortality and morbidity due to relatively high rates of malfunction and infection,Citation6,Citation7 they continue to be a necessary option for hemodialysis patients in whom AV access is likely to be problematic, impossible, or contraindicted.Citation8 This includes elderly patients with poor vascular condition, those who have an inability to withstand internal fistula due to poor cardiac function and those unsuitable for peritoneal dialysis.Citation2 Furthermore, maturation of an AV fistula typically takes 3 months but can take up to 1 year, and failure to mature is estimated to be as high as 60%.Citation8,Citation9
Given the global trend towards an increasingly elderly hemodialysis population with a similar increasing prevalence of diabetes and cardiovascular comorbidities, the number of patients requiring chronic hemodialysis that are unsuitable for an AV fistula is increasing.Citation10,Citation11 This is especially true in China, where the above factors are leading to an increasing incidence of end-stage renal disease (ESRD).Citation12,Citation13
Continuous advances in catheter design have improved the durability of catheter function and also lowered the incidence of catheter-related infection.Citation1,Citation10 The symmetrical-tip dialysis catheter (Tal Palindrome™, Covidien, Mansfield, MA) is a recent catheter design with a symmetric, spiral tip, and biased ports.Citation14 Results from previous studies suggest that the symmetrical-tip catheter has several functional advantages over other catheter designs; for example, lower rates of thrombosis and re-intervention compared with split distal tip catheters,Citation15 and a lower dysfunction rate compared with step-tip catheters.Citation16 However, there is relatively little clinical data describing long-term performance of the symmetrical-tip catheter for chronic hemodialysis, as much of the existing clinical research was conducted over a timescale of only a few months.Citation15,Citation16 In addition, there have been no previous reports in English-language journals of symmetrical-tip catheter use in China.
We, therefore, conducted a retrospective analysis of patients who underwent chronic hemodialysis catheterization at our institution in Shanghai between May 2009 and December 2011, and evaluated the long-term functionality and infection rate associated with the symmetrical-tip hemodialysis catheter compared with a step-tip catheter.
Materials and methods
Patients
A total of 284 placements of permanent, indwelling venous catheters in 271 Chinese ESRD patients between 1 May 2009 and 31 December 2011 were included in this retrospective analysis. Of these catheterizations, 118 were performed using 36/40 cm pre-curved or straight symmetrical-tip catheters including 14 cases where step-tip catheters were changed to symmetrical-tip, and 166 catheterizations were performed using 36/40 cm step-tip catheters (Quinton™ Permcath™, Covidien, Mansfield, MA). All patients provided written and informed consent, and the study received ethical approval from the institutional ethics review board. The study was conducted in accordance with the Declaration of Helsinki 2000 and the Declaration of Istanbul 2008.
Description of hemodialysis catheters
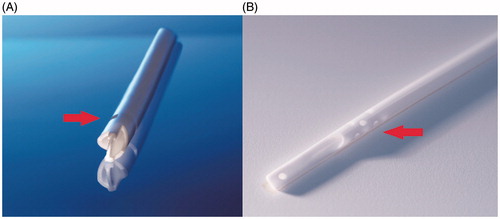
The symmetrical-tip catheter is made from a polyurethane material and has a symmetrical, spiral end-tip design, whereby inflow occurs through a laser-cut side slot located on the most proximal portion of the end hole, and outflow occurs as a jet directed away from the catheter tip. This design is thought to prevent clot formation ().Citation10,Citation17 In contrast, the relatively older step-tip catheter is composed of a soft, silicone material and is designed with a staggered tip to provide a 2.5 cm separation between the arterial lumen and venous tip ().
Figure 1. Close-up view of the (A) symmetrical catheter (Tal Palindrome™) tip showing the symmetrical spiral-tip design and laser-cut side slot (arrow), and (B) the step-tip catheter (Quinton™ Permcath™), showing the side holes (arrow) and staggered tip, which provides a 2.5 cm separation between the arterial lumen and venous tip.
Description of hemodialysis catheter insertion technique
Catheter insertion was conducted under local anesthesia (1% lidocaine) in the department operating room. For patients requiring catheter reinsertion, or in difficult cases, the procedure was performed with ultrasonographic guidance. The preferred insertion site was the internal jugular vein (IJV), followed by the subclavian vein (SC) and external jugular vein (EJV). Anatomical landmarks were used to localize the insertion sites: the puncture site for IJV catheterizations was the apex of the triangle formed by the sternocleidomastoid muscle; the puncture site for SC catheterizations was 0.5 cm from the junction of the clavicular head of the sternocleidomastoid muscle and the clavicle. An alternative puncture site for SC catheterization was 0.5–1 cm below the junction of the lateral third and medial two-thirds of the clavicle shaft.
A modified Seldinger technique was used to place catheters in the IJV and SC.Citation18 The puncture site was prepped and draped and the selected vein was punctured with a 21-Gauge needle, after which a 0.038-in. guide wire was inserted. The subcutaneous tissue at the entry site was pre-dilated with a 12F dilation catheter and then a 16F peel-away sheath placed. The permanent catheter was inserted in its final position using a peel-away sheath. In the case of the IJV and SC catheters, the final position was the right mid-atrium or the superior vena cava–atrium junction.
The venous cut down approach was used to place EJV catheters. Patients were briefly placed into the Trendelenburg position to transcutaneously identify the course of the EJV. Next, a longitudinal 1.5 cm skin incision was made overlying the EJV in the mid-neck region. The EJV was then circumferentially dissected out and partially transected. The permanent catheter was passed into the lumen of the partially transected EJV and directed centrally towards the heart. The final position of the central venous catheter depends on the relative positioning of the upper portion of the right atrium and ribs or intercostal space of the anterior thoracic wall, as determined by pre-surgery chest X-ray. The final position of the catheter tip was usually at the third anterior rib or intercostal space. For difficult cases, such as catheter reinsertion and central venous stenosis, catheter insertion was guided under digital subtraction angiography. Once correctly positioned, one 2-0 silk suture was placed around the catheter at the entry site and the distal end of EJV was tied down around the catheter to prevent back-bleeding and catheter migration. The subcutaneous tunnel was approximately 10–12 cm in length and the catheter cuff was positioned within 2–3 cm of the exit site. The final catheter position was verified using a chest X-ray.
Following the placement procedure, the exit site was covered with sterile gauze or 3 M tape and the indwelling catheter was sealed with heparinized saline solution. Patients underwent routine hemodialysis the day after surgery.
Clinical parameters and statistics
The primary endpoint was catheter dwell time, defined as the time interval from catheter insertion to catheter removal or the date of the last visit the patient made to the hospital during the study time window. Other endpoints included occurrence of low blood flow, rates of infection and catheter-related blood stream infection (CRBSI) and catheter removal. Low blood flow was defined as a dialyzer blood flow in mL/min less than four times patient body weight in kilograms (i.e. for a patient weighing 75 kg, the cut-off for low blood flow would be 300 mL/min) at a pre-pump pressure of −250 mmHg. This weight-adjusted definition of low blood flow was used to take into account the lower mean body weight of Chinese hemodialysis patients, compared with their European or American counterparts. Although this was a retrospective analysis and the equipment used varied between patients, blood flow and recirculation rates were predominantly measured using the Transonic Hemodialysis Monitor HD02 (Transonic Systems, Ithaca, NY).
This study used the definition of CRBSI set out by the US Centers for Disease Control and Prevention and as recommended by the Kidney Disease Outcomes Quality Initiative guidelines.Citation19 In addition, exit site infection was defined as red, swollen skin adjacent to the exit site with purulent secretion, with patients reporting pain but not presenting with a fever. In this case, patients were treated with MuPirocin antibiotic ointment (SK&F, Shanghai, China) locally for 1 week. Subcutaneous tunnel infection was defined as red, swollen skin at the subcutaneous tunnel and pus observed at the catheter exit site with patients reporting pain and presenting with a fever and shivering.
In addition, a small number of the symmetrical-tip (n = 10) and step-tip (n = 10) catheter cases were randomly selected for measurement of blood flow and recirculation, and assessment of blood flow after reversal of the dialysis lines.
Management of complications
In general, indications for catheter withdrawal included chronic infection, catheter dysfunction (includes low blood flow, and abnormal position dysfunction), death, kidney transplantation (catheter still functional), and catheter cuff exposure.
For patients who experienced low catheter blood flow, mechanical causes such as ectopic catheter, stenosis, and bending or kinking of the catheter were first excluded by methods including non-invasive central venous computed tomography angiography or cardiac ultrasound examination. Low blood flow caused by the catheter tip becoming stuck to a blood vessel wall due to vacuum effects was excluded in the case of the symmetrical-tip catheter by reversing the arterial and venous lines.
Following exclusion of mechanical causes, 50,000–250,000 units of urokinase in 3–5 mL of saline solution were injected into the catheter and kept for 25–30 min; dissolved fibrin or blood clots were then extracted. This process could be repeated 2–3 times until blood flow normalized. In cases with continued poor blood flow, it was assumed that a fibrin sheath had formed around the catheter tip. In this case, 250,000 units of urokinase were infused slowly through the catheter for 12–24 h a day for 3–5 d. If poor blood flow could not be corrected at this time, the catheter was removed and re-inserted.
In view of the vital importance of catheter access for patients requiring chronic hemodialysis, it was a common practice at our institution that patients suspected of catheter-related infection received antibiotic treatment before a decision was made to remove the catheter. Antibiotics were predominantly infused through the catheters using an antibiotic seal. First-line treatment typically included third-generation cephalosporin with aminoglycoside or quinolones, and the treatment was adjusted based on the outcomes of bacterial culture. If antibiotic treatment was effective, it would be continued for at least 2 weeks. Patients with bacteremia or sepsis received treatment with antibiotics under heparin lock for 4–6 weeks.
Statistical methods
Data are expressed as mean ± standard deviation (SD) unless otherwise indicated. The rate of occurrence of infection and low blood flow was calculated as the number of events per 1000 catheter days. Differences in continuous variables were compared using Student’s t-test, apart from differences in rates of infection and low blood flow, which were compared using the Chi-square test. A p value < 0.05 was considered significant.
Results
Patient demographics and disease characteristics
A total of 284 cases of chronic catheterization in 271 patients with ESRD were included in the analysis: 118 using symmetrical-tip catheters and 166 using step-tip catheters. The mean age of patients was similar between the symmetrical-tip and step-tip catheter groups: 67.4 ± 15.2 and 67.8 ± 13.1 years, respectively (). The ratio of males to females was lower in the symmetrical-tip group compared with the step-tip group, at 48% versus 71%, however, this difference was not statistically significant (p > 0.05).
Table 1. Demographics and background disease characteristics.
The most common cause for chronic hemodialysis was diabetic nephropathy for patients in the symmetrical-tip catheter group (52% [61/118]), and chronic nephritis (40% [67/166]) for patients in the step-tip catheter group. There was a higher proportion of patients with metabolic disease in the symmetrical-tip catheter group (diabetic neuropathy or hypertension) than in the step-tip group at 69% (82/118; 52 diabetic neuropathy and 18 hypertension) versus 34% (57/166; 19 diabetic neuropathy and 15 hypertension), respectively (p < 0.01) (). The most common route of catheter placement in both the symmetrical-tip and step-tip groups was the right IJV. There was no difference in the routes of catheter placement between the two groups ().
Table 2. Summary of routes of catheter placement.
Long-term catheter functionality and safety
A total of 118 symmetrical-tip catheters and 166 step-tip catheters were placed for a total of 33,874 and 45,342 catheter days, respectively. Overall, the long-term functionality of the symmetrical-tip catheter was favorable compared with the step-tip catheter. In particular, the mean dwell time for the symmetrical-tip catheter group was significantly longer than the step-tip catheter group (329.4 ± 38.1 vs. 273.1 ± 25.4 catheter days; p < 0.05), and the rate of low blood flow occurrence was significantly lower for symmetrical-tip compared with step-tip catheters (1.13 vs. 6.86 per 1000 catheter days; p < 0.01) (). The number of catheter removals was lower with the symmetrical-tip catheters than step-tip catheters (10 vs. 26, respectively; p < 0.05). Infection and low blood flow were responsible for over half of the catheter removals (50% for symmetrical-tip vs. 77% for step-tip catheters; p < 0.05). A summary of reasons for catheter removal is presented in .
Table 3. Mean catheter dwell time, rates of incidence of low blood flow and incidence of infection.
The incidence of infection was lower in the symmetrical-tip catheter group than in the step-tip catheter group; the infection rate was 0.28 versus 0.78 per 1000 catheter days (p < 0.01) and the CRBSI rate was 0.13 versus 0.42 per 1000 catheter days (p < 0.01) for the symmetrical-tip group and step-tip group, respectively.
Catheter flow and recirculation
A flow rate of 250–300 mL/min was measured by Transonic in all of the 10 symmetrical-tip and step-tip catheter cases randomly selected for flow measurement. In addition, recirculation was evaluated in six symmetrical-tip and 10 step-tip catheters. In the symmetrical-tip catheters, the recirculation rate was 0%, with no cases of poor flow on reversing the connection. A recirculation rate of 0–5% was measured in the step-tip catheters, with five cases of poor flow on reversing the connection.
Discussion
AV fistula are preferred over hemodialysis catheters due to the complications associated with catheter use, which include a high incidence of thrombosis,Citation20,Citation21 and bacterial infections.Citation22 Furthermore, hemodialysis catheter dysfunction is associated with significant mortality.Citation23 However, hemodialysis catheters remain a necessary option for patients in whom an AV fistula placement is unfeasable.Citation8 Therefore, given the importance of adequate vascular access for patients requiring hemodialysis, improvements in catheter design aim to improve long-term functionality, while lowering the incidence of infections and complications.
This retrospective analysis of Chinese ESRD patients, who received chronic hemodialysis between 2009 and 2011, is the first report in an English-language journal of symmetrical-tip catheter use in China. The symmetrical-tip catheter was associated with a significantly longer mean catheter dwell time and a significantly lower incidence of low blood flow compared with the step-tip catheter. These results support existing data demonstrating favorable long-term functionality of the symmetrical-tip catheter compared with a split-tip catheter (catheter patency at 180 d, 90% vs. 61%; p < 0.0001) and a step-tip catheter (dysfunction-free survival at 2 months, 78.9% vs. 54.4%; p = 0.015).Citation15,Citation16 In a small sample of patients included in the present study, a lower recirculation rate was measured with the symmetrical-tip catheters compared with the step-tip catheters (0% vs. 0–5%); however, as these measurements were made in a small sample of patients, the conclusions that can be drawn from these data are limited.
Interestingly, the mean catheter dwell times for both the symmetrical-tip (329.4 d) and step-tip (273.1 d) catheters observed in this study far exceed previously published values, which are typically around 100 d.Citation14 However, although the mean dwell times were longer, the range of catheter dwell times in the current study was 13–724 d, which is comparable with ranges of 1–673 d reported in previous studies.Citation14
It is estimated that catheter dysfunction accounts for 17–33% of untimely catheter removals.Citation24,Citation25 Therefore, the lower incidence rate of low blood flow observed with symmetrical-tip versus step-tip catheters in this study may be a contributing factor to the significantly longer mean dwell time associated with this catheter design. It has been proposed that because blood enters the symmetrical-tip catheter through the side slots and exits through the tip, this reduces the formation of thrombus and fibrin sheath formation, leading to a lower rate of fibrin sheath formation with the spiral-tip design of the symmetrical-tip catheter (8.7%), compared with other catheter types (42–100%).Citation10,Citation14
The infection rates observed in this study (0.28 and 0.78 per 1000 catheter days for the symmetrical-tip and step-tip catheters, respectively) are low compared with general literature values for dialysis catheters, which range from 0.25 to 6.5 per 1000 catheter days.Citation15 We propose that the primary factor for the lower rate of infection in the symmetrical-tip catheters versus the step-tip catheters may be the higher patency of the symmetrical-tip catheter; as a result of higher patency, less intervention was required for the former catheter design, and, therefore, the risk of introducing an infection was lower. The significantly lower rates of infection and CRBSI associated with the symmetrical-tip catheter compared with the step-tip catheter may be another contributing factor for the longer mean dwell time associated with the symmetrical-tip catheter. However, it should be noted that other, comparative studies have found the symmetrical-tip catheter to demonstrate superior long-term functionality compared to step- and split-tip catheters, despite reporting similar rates of infection.Citation15,Citation16
There were several limitations to this study. Firstly, patients who had their catheters changed from step-tip to symmetrical-tip were included as two separate cases, which may have caused a bias in results, although there were only eight such patients in total. Further, catheter blood flow and recirculation were not routinely measured for all cases; these measurements would have provided more quantitative data on catheter function. Additionally, a significantly larger proportion of patients in the symmetrical-tip catheter group had metabolic disorders compared with the step-tip catheter group, which may have affected the study outcomes. However, although some research suggests that diabetes is associated with an increased risk of catheter-related infection,Citation26 there are counter examples reporting that diabetes is not a significant independent risk factor for catheter-related infection.Citation15,Citation27,Citation28 Despite these limitations, our findings provide a valuable contribution to the existing literature supporting the use of symmetrical-tip catheters for chronic hemodialysis, and provide the first report of symmetrical-tip catheter use in China.
In summary, this retrospective analysis demonstrated that symmetrical-tip hemodialysis catheters are associated with a longer average dwell time, a lower incidence of low blood flow and lower rates of infection compared with step-tip catheters. These findings support the use of the symmetrical-tip catheter for long-term vascular access in patients requiring chronic hemodialysis who are unsuitable for AV fistula. Given the findings of this study, a larger, randomized controlled study to compare the long-term functionality and complication rate of the symmetrical-tip catheter against other catheter types is warranted.
Declaration of interest
Covidien financially supported third-party editorial assistance for this manuscript, which was provided by Health Interactions Shanghai.
References
- Tordoir J, Canaud B, Haage P, et al. EBPG on vascular access. Nephrol Dial Transplant. 2007;22(Suppl 2):ii88–117
- National Kidney Foundation. KDOQI clinical practice guidelines and clinical practice recommendations for 2006 updates: Hemodialysis adequacy, peritoneal dialysis adequacy and vascular acccess. Am J Kidney Dis. 2006;48:S1–S322
- The Fistula First Catheter Last Workgroup Coalition. Fistula First Catheter Last Initiative 2015. Available at: http://esrdncc.org/ffcl/
- Kulawik D, Sands JJ, Mayo K, et al. Focused vascular access education to reduce the use of chronic tunneled hemodialysis catheters: Results of a network quality improvement initiative. Semin Dial. 2009;22(6):692–697
- U.S. Renal Data System. USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease; 2013
- Lacson E Jr, Lazarus JM, Himmelfarb J, Ikizler TA, Hakim RM. Balancing fistula first with catheters last. Am J Kidney Dis. 2007;50(3):379–395
- Ocak G, Halbesma N, le Cessie S, et al. Hemodialysis catheters increase mortality as compared to arteriovenous accesses especially in elderly patients. Nephrol Dial Transplant. 2011;26(8):2611–2617
- Dember LM, Beck GJ, Allon M, et al. Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: A randomized controlled trial. JAMA. 2008;299(18):2164–2171
- U.S. Renal Data System. USRDS 2007 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease; 2007
- Knuttinen MG, Bobra S, Hardman J, Gaba RC, Bui JT, Owens CA. A review of evolving dialysis catheter technologies. Semin Intervent Radiol. 2009;26(2):106–114
- Akoh JA. Prosthetic arteriovenous grafts for hemodialysis. J Vasc Access. 2009;10(3):137–147
- Zuo L, Wang M. Current burden and probable increasing incidence of ESRD in China. Clin Nephrol. 2010;74(Suppl 1):S20–S22
- Chen J. Epidemiology of hypertension and chronic kidney disease in China. Curr Opin Nephrol Hypertens. 2010;19(3):278–282
- Spector M, Mojibian H, Eliseo D, et al. Clinical outcome of the Tal Palindrome chronic hemodialysis catheter: Single institution experience. J Vasc Interv Radiol. 2008;19(10):1434–1438
- Kakkos SK, Haddad GK, Haddad RK, Scully MM. Effectiveness of a new tunneled catheter in preventing catheter malfunction: A comparative study. J Vasc Interv Radiol. 2008;19(7):1018–1026
- Hwang HS, Kang SH, Choi SR, Sun IO, Park HS, Kim Y. Comparison of the palindrome vs. step-tip tunneled hemodialysis catheter: A prospective randomized trial. Semin Dial. 2012;25(5):587–591
- Tal MG, Ni N. Selecting optimal hemodialysis catheters: Material, design, advanced features, and preferences. Tech Vasc Interv Radiol. 2008;11(3):186–191
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography. A new technique. Acta Radiol Suppl (Stockholm). 2008;434:47–52
- Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006;48(Suppl 1):S176–S247
- Watnick S, Stooksbury M, Winter R, Riscoe M, Cohen DM. White thrombus formation in blood tubing lines in a chronic hemodialysis unit. Clin J Am Soc Nephrol. 2008;3(2):382–386
- Willms L, Vercaigne LM. Does warfarin safely prevent clotting of hemodialysis catheters? A review of efficacy and safety. Semin Dial. 2008;21(1):71–77
- U.S. Renal Data System. USRDS 2008 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease; 2008
- Owen WF Jr, Chertow GM, Lazarus JM, Lowrie EG. Dose of hemodialysis and survival: Differences by race and sex. JAMA. 1998;280(20):1764–1768
- Little MA, O'Riordan A, Lucey B, et al. A prospective study of complications associated with cuffed, tunnelled hemodialysis catheters. Nephrol Dial Transplant. 2001;16(11):2194–2200
- Ponikvar R, Buturovic-Ponikvar J. Temporary hemodialysis catheters as a long-term vascular access in chronic hemodialysis patients. Ther Apher Dial. 2005;9(3):250–253
- Jean G, Charra B, Chazot C, et al. Risk factor analysis for long-term tunneled dialysis catheter-related bacteremias. Nephron. 2002;91(3):399–405
- Tanriover B, Carlton D, Saddekni S, et al. Bacteremia associated with tunneled dialysis catheters: Comparison of two treatment strategies. Kidney Int. 2000;57(5):2151–2155
- Pastan S, Soucie JM, McClellan WM. Vascular access and increased risk of death among hemodialysis patients. Kidney Int. 2002;62(2):620–626

