Abstract
Interest in nephrology careers continues to decline in the United States. The reasons for this declining interest are not fully understood but it is plausible that inadequate exposure to the full spectrum of what a career in nephrology encompasses may be part of the explanation. Inpatient-based nephrology electives have been a common venue for residents to gain exposure to nephrology but little is known regarding the details of such electives and how often they include outpatient experiences. We carried out a national survey of nephrology fellowship training program directors to obtain data on the content of nephrology elective experiences as well as their ideas on how to promote interest in the field. The survey revealed the majority of elective experiences to be either exclusively or heavily inpatient based, with only a small percentage having a substantial outpatient component, particularly in outpatient dialysis or transplantation. Training program directors felt that providing greater outpatient experiences to residents during elective rotations would be an effective means to promote interest in nephrology, along with structured faculty mentoring. Our findings suggest that current approaches to the nephrology elective experience are heavily inpatient-based and might benefit from incorporating much more of the rich spectrum of activities a career in nephrology entails. Hopefully such efforts can create and enhance interest in careers in nephrology and potentially begin a sustained reversal of an unfortunate and serious decline in interest.
Introduction
Careers in general internal medicine (IM) and its subspecialties typically include a wide spectrum of activities outside of the inpatient hospital setting. However, IM residents on subspecialty electives often have heavily inpatient-based experiences which may fail to provide them with a representative exposure to the full scope of what physicians in those fields do in their careers. This may have important implications not only for learning but also for helping IM residents to make sound career choices.
Interest in nephrology careers continues to decline in the United States (US).Citation1 Applications for pursuing nephrology fellowship training have dramatically decreased amongst both US and international medical graduates.Citation2–4 Nephrology fellowship training program directors (N-TPDs) in the US are facing an enormous challenge in filling their fellowships positions and the impact of this decrease was clearly felt by them on Match Day 2014. Thirty-two percent of the nephrology fellowship positions in the Match remained unfilled, with an alarming 51% of the participating programs not filling all positions.Citation5 Nephrology in the US is clearly facing a challenging time in attracting prospective trainees into the field.Citation1–6
Several factors can influence medical trainees’ career choices, including intellectual interest in a particular field, the presence or lack of a significant procedural component, income potential, job opportunities, financial debts, family commitments, and geographical constraints, among others.Citation7–12 Exposure to various subspecialties during medical school or residency may be one such variable that can strongly influence career choices.Citation8,Citation9 Although many factors may play a role in attracting medical students and residents into nephrology, one important factor may be how well nephrology is presented to trainees.
Some of the reasons that have been reported in the past for this declining interest in nephrology careers have included lack of mentorship, difficult-to-understand or unstimulating nephrology courses in medical school or during residency, disheartening inpatient elective experiences, a lack of representative nephrology elective experience during medical school or residency, and few opportunities to experience other aspects of nephrology careers such as outpatient nephrology clinics, outpatient dialysis, and kidney transplantation.Citation1,Citation11,Citation13 Other reasons include a perceived heavy workload and poor remuneration in nephrology, and interaction with nephrology fellows or attending physicians who are less satisfied or dissatisfied with their career choice.Citation7,Citation11 Poor job opportunities following fellowship training may also play a role in declining interest in nephrology careers.Citation7,Citation14
It is likely that the type of nephrology elective that IM residents experience may have an important influence on their choice of nephrology as a career and this may be true for many other specialties as well though for some it does not appear likely that inpatient-weighted elective experiences impact negatively on career choice.
The types of nephrology electives offered during IM residency in the US are not known, and in particular it is not known to what extent they provide residents with representative experiences encompassing the broad spectrum of outpatient as well as inpatient activities a practicing nephrologist is engaged in.Citation15 To gain a greater insight, we carried out a national survey of N-TPDs to obtain data on the content of nephrology elective experiences.
Methods
The study was deemed exempt by the institutional review board at the North Shore-Long Island Jewish Health System. The survey was initially sent to all 146 adult US N-TPDs via e-mail in May 2013. The survey was anonymous and consisted of several questions that related to N-TPDs’ perceptions of IM residents’ exposure to clinical nephrology and elective experience during residency training (). The survey also explored N-TPDs’ thoughts on effective measures to foster interest in nephrology careers, optimal duration of a nephrology elective during medical residency, characteristics of an “ideal” nephrology elective experience for residents and reasons for no or limited outpatient experience (if applicable) at their respective institutions (). The survey included yes/no and multiple-choice questions. Survey reminders were subsequently sent in June, July and August 2013. Respondents were not allowed to skip questions. The survey was closed on 30 August 2013.
Table 1. Nephrology elective experience during medical residency: survey questions.
Results
Description and location of IM residency programs
A total of 91 US N-TPDs responded to our survey, representing approximately 62% of the total number of nephrology fellowship programs in 2012–2013. The majority (59.3%) of the responding N-TPDs were from large tertiary academic center programs (defined as having more than 30 residents per intern class). Nearly one-fourth (25.3%) of the respondents were from small to medium-sized tertiary academic center programs (having fewer than 30 residents per intern class). The remaining responding programs included both large community hospital-based programs (9.9%) and small to medium-sized community hospital-based programs (5.5%) with less than 30 residents per intern class. 42.9% of the responding programs were located in northeast US. The remaining programs were either in southeast (19.8%), western (13.2%) or Midwestern US (24.2%).
Clinical nephrology services offered and nephrology faculty involvement in IM residency program leadership
Most of the responding programs offered all of the clinical nephrology services at their institutions that included outpatient hemodialysis (98.9%), home hemodialysis (72.5%), peritoneal dialysis (95.6%), kidney transplant (86.8%), interventional radiology (97.8%), and critical care (97.8%). Nearly one-third of the programs (28.6%) also offered interventional nephrology services at their institutions.
When asked about the involvement of nephrology faculty in IM program leadership (e.g., chair or vice-chair of medicine, IM program directors, and IM clerkship directors) at their institution, N-TPDs responded as follows: very involved (27.5%), frequently involved (23.1%), sometimes involved (19.8%), infrequently involved (22.0%) or not at all involved (7.7%).
Exposure to clinical nephrology during medical residency
N-TPDs were asked to identify clinical or educational experiences at their respective institution that would expose IM residents to clinical nephrology. All (100%) of the responding programs provided nephrology elective experience to medical residents. Other experiences that exposed residents to clinical nephrology at these institutions included: nephrology faculty participation in resident conferences including morning resident report (84.6%), nephrology faculty teaching and supervising as general IM ward attending (56%) and resident rotations on a dedicated inpatient nephrology ward (26.4%). Other experiences, although uncommon, included residents rotating through nephrology outpatient clinics (2.2%) during ambulatory block time and nephrology faculty teaching as intensive care unit attending (1.1%).
Duration of nephrology electives offered and chosen during medical residency
The majority (87.9%) of the responding programs offered a 4-week nephrology elective at their institution. Nearly half (48.4%) of all responding programs also offered a 2-week nephrology elective during IM residency. Other elective durations offered, although far less frequently, included: >4 weeks (3.3%), 3 weeks (8.8%) and <2 weeks (4.4%). The majority (60.4%) of the N-TPDs responded that the 4-week long rotation was the most common nephrology elective chosen by IM residents at their respective institution. However, for nearly one-third (31.9%) of the programs, a 2-week long elective was the most common selection. Very few N-TPDs responded the electives that were >4 weeks (2.2%), 3 weeks (4.4%), or <2 weeks (1.1%), were commonly chosen by residents in their institution.
Nephrology elective experience during medical residency
N-TPDs were asked to characterize the nephrology elective experiences for IM residents at their institution. All except one responding program offered inpatient general nephrology consultative service (98.9%) to medical residents at their institution (). The other inpatient experiences included: inpatient end-stage renal disease (ESRD)/dialysis services (42.9%), inpatient renal transplant service (34.1%), critical care nephrology (1.1%) and onco-nephrology consult service (1.1%). The ambulatory experiences offered at responding programs included: outpatient general nephrology experience (58.2%), outpatient renal transplant experience (22%), outpatient hemodialysis experience (12.1%), and outpatient peritoneal dialysis experience (11.0%). Interventional radiology/nephrology experience was offered in five programs (5.5%).
Table 2. Characteristics of nephrology elective experience during medical residency (in percentage).
N-TPDs were asked how they would best describe their “typical” 4-week elective experience for most IM residents at their institution. Over half (52.8%) of the responding N-TPDs described their 4-week elective to be a pure inpatient experience (). Of these, nearly one-third (29.7%) described this experience to be an inpatient consultative elective, while the other 23.1% described the elective to be a combination of both inpatient consultative and inpatient ESRD/dialysis experience. The remaining experiences included: inpatient experience with few renal clinic experiences (on average ≤1 clinic per week) (22%), inpatient experience with several renal clinic experiences (on average >1 or =2 clinics per week) (11%) and 2 weeks of inpatient and 2 weeks of outpatient nephrology experiences (including renal clinics, dialysis unit rounding, and outpatient transplant center experiences) (4.4%). There were no programs offering a 4-week inpatient rotation with an average of more than two clinics per week. Only one program described their elective to be a pure outpatient nephrology experience. Two (2.2%) programs also offered (free responses) either 4 weeks of inpatient or 4 weeks of outpatient experiences based on resident’s interest. The remaining six programs (6.6%) did not offer a 4-week elective.
Table 3. Types of 4- and 2-week nephrology elective experience of US internal medicine residents (in percentage).
N-TPDs were also asked how they would best describe their “typical” 2-week elective experience for most IM residents at their institution. Majority (57.2%) of N-TPDs described their 2-week elective to be a pure inpatient experience (). Of these, over one-third (34.1%) described this experience to be an inpatient consultative elective, while the other 23.1% described the elective to be a combination of both inpatient consultative and inpatient ESRD/dialysis experience. The remaining experiences included: inpatient experience with few renal clinic experiences (on average ≤1 clinic per week) (15.4%), inpatient experience with several renal clinic experiences (on average >1 or =2 clinics per week) (8.8%) and 1 week of inpatient and 1 week of outpatient nephrology experiences (including renal clinics, dialysis unit rounding, and outpatient transplant center experiences) (3.3%). Two programs described their elective to be a pure outpatient experience. There were no programs offering a 2-week inpatient rotation with an average of more than two clinics per week. The remaining programs did not offer 2-week electives to IM residents. Based on our findings, it seems that the 2-week electives were less likely to have outpatient clinic experiences compared with 4-week electives.
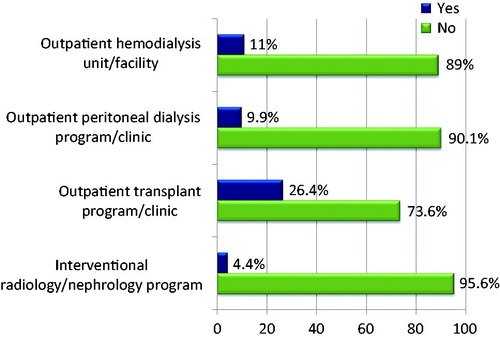
Nearly 90% of the programs did not rotate their IM residents in either their outpatient hemodialysis unit or peritoneal dialysis clinic during their nephrology elective (). Only one-fourth (26.4%) rotated their IM residents in their outpatient kidney transplant program. Four programs (4.4%) also rotated medical residents through their interventional radiology/nephrology program.
Figure 1. Do your medical residents rotate through your outpatient hemodialysis, peritoneal dialysis, transplant and interventional radiology/nephrology programs during their nephrology elective?
The responses to whether medical residents participate in nephrology conference during elective time were as follows: always (31.9%), frequently (38.5%), sometimes (27.5%) and never (2.2%).
Fellow involvement and faculty interactions during nephrology elective and research opportunities
Fellow involvement in teaching and supervising medical residents during the elective was also determined on the survey. The responses were as follows: very involved (33.1%), frequently involved (51.6%), sometimes involved (9.9%), infrequently involved (3.3%), and not at all involved (2.2%).
The number of clinical faculty members each resident interacts during a typical 4-week elective was as follows: one (3.3%), two (44%), three (24.2%), four (14.3%) and >four (14.3%).
While over half (53.8%) of the programs offered mainly clinical research opportunities to their medical residents, another one-third (34.1%) of the programs offered both basic science research and clinical research opportunities. A smaller number (4.4%) of programs offered mainly basic science research opportunity to medical residents. Five programs did not offer any research opportunities.
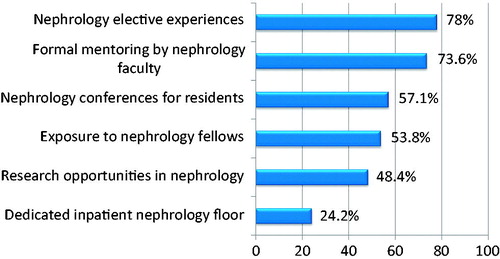
Effective ways of fostering interest in nephrology careers
N-TPDs identified nephrology elective experience (78%) and formal nephrology faculty mentoring (73.6%) as the two most effective ways in fostering interest in nephrology careers (). The other effective ways to foster interest identified by N-TPDs were as follows: nephrology conference for residents (57.1%), exposure to fellows (53.8%), nephrology research opportunities (48.4%) and dedicated inpatient nephrology ward (24.2%). One N-TPD also suggested longitudinal nephrology clinic for medical residents as an effective way to foster interest in nephrology.
“Optimal” duration of nephrology elective during medical residency
While nearly three-fourths (73.6%) of the N-TPDs felt that a 4-week elective would provide adequate exposure to nephrology during residency, another 19 (20.9%) N-TPDs felt that an elective more than 4 weeks long would be needed for adequate exposure to the field. Only one (1.1%) respondent suggested that a 2-week rotation would be adequate, while another four (4.4%) respondents felt that a 3-week elective would provide adequate exposure.
“Ideal” nephrology elective experience
Nearly 88% of the N-TPDs thought that an “ideal” nephrology elective experience for medical residents should consist of both inpatient and outpatient experiences (including outpatient dialysis and transplantation). Only two (2.2%) respondents felt that a pure inpatient consultative experience should be an “ideal” elective experience for medical residents. The other responses were as follows: pure outpatient experience (2.2%) and inpatient consultative and inpatient ESRD/dialysis experience (7.7%).
At the time of this survey, over half (57.1%) of the N-TPDs responded that their nephrology elective structure did not provide medical residents with a realistic insight into the professional life of a practicing nephrologist.
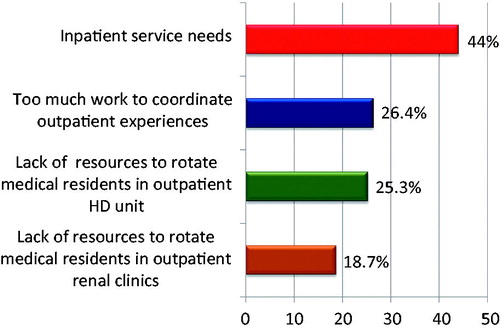
Reasons why medical residents have no or limited outpatient nephrology elective experience
“Inpatient service needs” (44%) and “too much work to coordinate various outpatient experiences” (26.4%) were the top two reasons identified by N-TPDs for no or limited outpatient nephrology elective experience for IM residents (). The other reasons included: lack of resources to rotate medical residents in outpatient hemodialysis units (25.3%), lack of resources to rotate medical residents in outpatient renal clinics (18.7%), “residents do not want any outpatient nephrology exposure” (13.2%), “no access to interventional radiology/nephrology program” (11%), lack of peritoneal dialysis program (2.2%), and non-availability of outpatient transplant program (2.2%).
Discussion
Subspecialty elective experiences during IM residency provide residents with a potential opportunity to learn more about what a career in that subspecialty entails. However, our survey revealed the majority of nephrology elective experiences to be either exclusively or heavily inpatient based. Outpatient experiences were especially lacking for outpatient dialysis and transplantation, suggesting that the most common elective model for nephrology at present may provide a distorted impression of what a nephrologist does for the majority of their time in practice. Over half of the respondents in our survey described their 2- and 4-week elective to be a pure inpatient experience. In contrast, most nephrology practice occurs in an outpatient setting that includes taking care of patients with chronic kidney disease and hypertension, ESRD patients on outpatient hemodialysis or peritoneal dialysis and kidney transplant patients.Citation15 The Renal Physicians Association 2012 Nephrology Practice Business Benchmarking Survey Report of 111 nephrology practices showed that while 39% of the services were provided in a hospital setting, the remaining services were mainly outpatient based.Citation15 These services included: outpatient dialysis (27%), office practice (22%), and other procedures (11%). The location where the “other procedures” were performed, however, was not specified on the survey report.Citation15 While our survey focused only on the nephrology elective experience, our findings suggest that it is plausible that electives in other subspecialties may also be heavily weighted toward inpatient venues and may be worthy of study.
Can restructuring the elective enhance education and interest in a particular field of medicine? In 1983, Goldenberg et al. studied the educational impact of a rheumatology elective for medical residents, and found that formal training through ambulatory care and/or inpatient oriented electives is essential if medical residents are to achieve adequate skills in subspecialty fields.Citation16 At the North Shore University Hospital and Long Island Jewish Medical Center, the nephrology elective was restructured for all medical traineesCitation8,Citation17,Citation18 to provide them with a richer and more representative educational experience. It includes a 2-week inpatient consultative/dialysis experience and a dedicated 2-week extensive outpatient experience.Citation8 The experience with the combined elective format was perceived favorably by IM residents.Citation8 Eighty-six percent of the IM residents who completed the 4-week redesigned nephrology elective reported that they would consider a career in nephrology, as opposed to 50% of residents who underwent the traditional inpatient-based consultative elective.Citation8
What would be some of the additional perceived benefits of a nephrology elective experience that is more representative of what nephrologists do in practice? As with all specialties, nephrology is a multifaceted field, and its scope extends far beyond the inpatient realm and the conditions seen there. An inpatient-based elective may not well expose the trainee to other career options that are available following nephrology fellowship training. However, a well-designed representative elective that includes both inpatient and extensive ambulatory (clinic, outpatient dialysis and transplantation) experiences would expose medical residents to additional career options in nephrology that they may have never considered such as transplant nephrology, medical directorship of a dialysis or transplant center and interventional nephrology.
Another potential benefit of such an elective would be the opportunity to interact with more faculty members with different perspectives and areas of expertise, making it more likely that a resident will encounter a faculty member who could serve as a mentor or role model. This would be especially important in cases in which a resident may have had an unfavorable experience with one faculty member, potentially resulting in the entire field being perceived negatively.
Another important reason for creating a representative elective experience would be to provide IM residents with the opportunity to understand what fellowships and careers in nephrology entail. There may be negative consequences when a resident pursues a fellowship in a field that they were not adequately exposed to during residency training. A survey of US adult nephrology fellows conducted in 2011 found a significant percentage of fellows who were less or not at all satisfied with their career choice.Citation7 One of the reasons cited for this dissatisfaction for nearly 20% of this group of fellows was that they did not enjoy caring for dialysis and transplant patients.Citation7 A career in nephrology may not be suitable or desirable for every trainee. However, with a well-planned representative elective experience, IM residents would likely make more well-informed decisions regarding whether nephrology is the right career for them. This measure would hopefully select for a population of nephrology trainees with a genuine and long-lasting interest in the field, leading to greater career satisfaction and advocacy for nephrology. While a broad spectrum of activities and interaction with multiple faculty members may provide a robust exposure to the field, if not carefully structured, fragmentation could result and the resident’s exposure to the field could end up being too diffuse. This could potentially interfere with their “immersion” into the field during the rotation.
We acknowledge that there may be limitations to the data we have collected. Although we feel that we had a good response rate, our sample of 91 of the 146 nephrology fellowship programs (in 2012–2013) may not be representative of all the IM training programs in the US, hence, response bias may have influenced our results. Furthermore, we did not survey IM residency programs where nephrology fellowship programs do not exist. It could be argued then that the ideal survey sample would include all institutions which have IM residency programs, regardless of whether they have nephrology fellowship programs as this would capture more institutions which have features consistent with a community hospital setting. Most physicians, including practicing nephrologists, work in community settings and not academic health settings and educational experiences in those settings might in some ways be more representative of what most nephrologists do in practice. We speculate, however, that the nephrology elective experience in an IM training program, where nephrology fellowship does not exist, would be predominately an inpatient-based experience, given that it would probably be much more difficult and cumbersome for a practicing and supervising nephrologist in the community to provide an extensive outpatient nephrology experience. It is also more likely that the outpatient experience at these teaching hospitals may be limited either due to lack of resources to rotate medical residents in dialysis units or due to non-availability of a transplant center. Another limitation in our study was that in order to assess the involvement of nephrology faculty in IM leadership we queried N-TPDs. These responses might have been biased somewhat toward a higher level of involvement compared to what might have been obtained from asking IM-TPDs.
Nearly three-fourth of the respondents felt that nephrology elective experiences were one of the most effective ways of fostering interest in nephrology careers. However, nearly 6 of 10 program directors responded that their current elective structure at their institution did not provide their medical residents with a realistic insight into the professional life of a practicing nephrologist. Nearly 9 of 10 program directors felt that an ideal nephrology elective for medical residents should consist of both combined inpatient and extensive outpatient experience including outpatient dialysis and outpatient transplantation. Most also felt that an elective of at least 4 weeks in duration was needed to provide adequate exposure to the field.
Nearly three of four responding program directors also felt that a formal mentoring program that involves an appointed nephrology faculty member would be another effective measure to foster interest in nephrology careers. Mentoring is perhaps equally important as suggested by a previous study of US adult nephrology fellows on career selection.Citation7 Strong mentorship during medical school and residency was one of the top reasons to choose nephrology careers.Citation7 Other data also support mentoring as influential in career choice.Citation12,Citation19 On the other hand, the survey of non-nephrology IM subspecialty fellows suggested that the lack of mentorship was a key factor for not choosing nephrology as a career.Citation11
Other activities that IM residents can engage in during residency training include long-term clinical research or basic science research that might lead to presentations at local, regional or national meetings, an experience that can also promote interest in the field. Our survey findings suggest most programs offered either clinical or basic science or both research opportunities to their medical residents. We, however, did not assess the duration and success of these research interactions or whether these research experiences have or will lead to increased interest in applying to nephrology fellowship programs.
Conclusions
This is the first study to evaluate the nephrology elective experience of US medical residents in training programs where nephrology fellowship programs exist. While most offered an inpatient-based nephrology elective experience, over half of the responding programs did not offer any outpatient experiences to IM residents. For programs that offered outpatient experiences, these were limited to renal clinic experiences. Most programs did not rotate their medical residents through their outpatient dialysis units or kidney transplant centers.
We believe that the nephrology elective experience of IM residents might be greatly enhanced by providing a more representative exposure which can enrich their learning and provide them with better information to make career choice decisions.
Acknowledgments
We gratefully acknowledge the nephrology training program directors throughout the US for taking the survey. Results of this study were presented in part at the American Society of Nephrology (ASN) Kidney Week 2013 in Atlanta, Georgia. Dr. Shah serves on the ASN Training Program Directors Executive Committee. Dr. Adams is the Chair of the ASN Training Program Directors Executive Committee. Drs. Shah, Adams and Jhaveri also serve on the ASN Workforce Committee.
Declaration of interest
There was no support or funding for this study. There are no potential conflicts of interest.
References
- Parker MG, Ibrahim T, Shaffer R, Rosner MH, Molitoris BA. The future of nephrology workforce: Will there be one? Clin J Am Soc Nephrol. 2011;6:1501–1506
- National Resident Matching Program, Results and Data. Specialties Matching Service 2014 Appointment Year. Washington, DC: National Resident Matching Program; 2014
- AAMC Electronic Residency Application Service. Nephrology (internal medicine) fellowship data [Data file]; 2013. Available at: https://www.aamc.org/download/360194/data/nephrology.pdf. Accessed December 26, 2014
- National Resident Matching Program, Results and Data. Specialties Matching Service 2013 Appointment Year. Washington, DC: National Resident Matching Program; 2013
- National Resident Matching Program. Specialties Matching Service Nephrology Match for Appointment Year 2015. Available at: http://www.asn-online.org/education/training/workforce/ASN_NRMP_SMS_2015_Analysis.pdf. Accessed December 26, 2014
- Desai T, Ferris M, Christiano C, Fang X. Predicting the number of US medical graduates entering adult nephrology fellowships using search term analysis. Am J Kidney Dis. 2012;59:467–469
- Shah HH, Jhaveri KD, Sparks MA, Mattana J. Career choice selection and satisfaction among US adult nephrology fellows. Clin J Am Soc Nephrol. 2012;7:1513–1520
- Jhaveri KD, Shah HH, Mattana J. Enhancing interest in nephrology careers during medical residency. Am J Kidney Dis. 2012;60:350–353
- Patel AB, Balzer MS. On becoming a nephrologist: Medical students’ ideas to enhance interest in a career in nephrology. Am J Kidney Dis. 2013;62:450–452
- Hoenig M, Shapiro E, Hladik G. Lessons learned from the ASN renal educator listserv and survey. Clin J Am Soc Nephrol. 2013;8:1054–1060
- Jhaveri KD, Sparks MA, Shah HH, et al. Why not nephrology? A survey of US internal medicine subspecialty fellows. Am J Kidney Dis. 2013;61:540–546
- Adams ND. Attracting more residents into nephrology. Clin J Am Soc Nephrol. 2012;7:1382–1384
- Rosner M, Parker M, Kohan D. Nephrology as a career choice: A survey of medical students [Abstract]. J Am Soc Nephrol. 2009;20:767A:SA–PO2867
- Salsberg E, Masselink L, Wu X. The US Nephrology Workforce: Developments and Trends. Washington, DC: American Society of Nephrology; 2014
- Renal Physicians Association. 2012 Nephrology Practice Business Benchmarking Survey (Based on 2011 Data). Rockville, MD: Renal Physicians Association; 2012
- Goldenberg DL, Meenan RF, Allaire S, Cohen AS. The educational impact of a rheumatology elective. Arthritis Rheum. 1983;26:658–663
- Shah HH, Jhaveri KD. Creating interest in nephrology careers: A novel nephrology elective experience for medical students [abstract]. J Am Soc Nephrol. 2013;24:294A:TH–PO858
- Jhaveri KD, Sparks MA, Shah HH. Novel educational approaches to enhance learning and interest in nephrology. Adv Chronic Kidney Dis. 2013;20:336–346
- Adams ND. Choosing nephrology – Or not. Am J Kidney Dis. 2013;61:529–531