Abstract
Backgrounds: The quality of life and survival of elderly depend not only on their age but on many social and health factors. In the present study, comprehensive geriatric assessment (CGA) was made in elderly patients on regular hemodialysis (HD) and those without chronic kidney disease recruited in primary health care in order to compare their sociodemographic characteristics, physical health, functional ability and social support. Method: The 106 HD patients and 300 primary care patients aged 70 years and more were studied. Data on sociodemographic characteristics, neurosensory deficits, pain, falls, polypharmacy, basic activities of daily living (ADL) questionnaire, instrumental activities of daily living (IADL) questionnaire were obtained during interview. The Timed Up and Go, Nutritional Health Checklist, Two Question Instrument for depression and Charlson comorbidity index (CCI) were applied. Results: No significant differences were found for age, gender, education level and dwelling between the two groups. A lower percentage of HD patients lived alone when compared with controls. BMI >25 kg/m2 had 43.4% of HD patients and 49.3% of controls. CCI differed significantly between HD and primary care patients (median: 6 vs. 4) and significantly more HD patients reported depression. No significant difference was found between groups for cognitive dysfunction and ADL, but HD patients had significantly lower IADL scores than controls. The mobility of HD patients was worse; 45.7% of them reported falls in the previous year but only 9.7% from the controls. Conclusions: CGA revealed that HD patients had significantly higher CCI, worse IADL score, mobility and reported more frequent falls, depression and impaired vision than primary care patients.
Introduction
Population ageing is taking place all over the world and the number of persons aged 60 years or over is expected to be more than double, from 841 million people in 2013 to more than 2 billion in 2050.Citation1 Older adults acquire more chronic illnesses than younger ones and often require medical services, most frequently from family doctors. Also, in the past decades the number of patients over 65 years of age on renal replacement therapy (RRT) has risen rapidly.Citation2 According to the ERA-EDTA Registry for 2011, the mean percentage of prevalent patients aged 65 years and older in countries providing individual patient data was 41%, with values of 37% for Bosnia and Herzegovina and 30% for Serbia.Citation3 The life expectancy of patients who began dialysis above 75 years of age is significantly shorter than for those aged between 50 and 60 yearsCitation4 or for patients not on dialysis.Citation5 However, older patients on dialysis are a heterogeneous group with different health, functional and socioeconomic status. Besides age, all these characteristics had an important influence on patient survival.Citation6,Citation7 It was reported that improved initial clinical status of elderly end-stage renal disease (ESRD) patients and better preparation for dialysis was associated with increased survival.Citation8
Decreased functional capacity, sensory deficits, cognitive impairment and depression have frequently been found in hemodialysis (HD) patientsCitation9–11 but only a few studies used comprehensive geriatric assessment (CGA) to evaluate HD patients.Citation11–14 CGA is a multidimensional procedure designed to evaluate an older person’s physical health, functional ability, cognition and mental health, and socioenvironmental circumstances, as well as an extensive review of prescriptions. It was developed in order to improve coordination and integration of treatment and follow-up of elderly patients, together with the outcome.Citation15
In the present study, CGA was conducted in elderly patients on HD with the aim of evaluating their sociodemographic characteristics, physical health, functional ability, cognitive and psychological functions as well as social support in comparison with a similar group of elderly patients without chronic kidney disease recruited in primary health care.
Materials and methods
The cross-sectional study was conducted in four HD centers (three from Bosnia and Herzegovina and one from Serbia) and in a primary health care institution – Health Center, Foča, Bosnia and Herzegovina. The study included 406 patients (106 on HD and 300 recruited in primary health care) who fulfilled the inclusion criteria: age 70 years and more, ability to give informed consent. Exclusion criteria were severe dementia, advanced malignancy, patients or their family refusing participation and, for patients from the control group, exclusion of chronic kidney disease defined according KDOQI guidelines.Citation16
All patients aged 70 years and more, who received regular HD in the four participating HD centers and fulfilled the inclusion–exclusion criteria, were included in the study. They had been on maintenance HD for 1–21 (4.6 ± 4.1) years and were dialyzed three times a week for 4 h using high-flux polysulfone membrane dialyzers with a blood flow rate of 300 mL/min, bicarbonate dialysate and heparin for standard anticoagulation. Balkan nephropathy was the primary kidney disease in 25 patients, diabetic nephropathy in nine, nephroangiosclerosis in 10, glomerulonephritis in 13, polycystic kidney disease in eight, other kidney diseases in 13 patients and in 28 patients the primary kidney disease was unknown.
The control group consisted of 300 consecutive primary care elderly patients without chronic kidney disease, who fulfilled the inclusion criteria and had visited their family physicians between 1 January and 5 May 2012. Among them 123 suffered from hypertension, 41 had diabetes (the majority with numerous chronic complications), 41 had heart disease, 4 had recovered from a cerebrovascular insult and had come for a regular check-up, 17 had chronic obstructive pulmonary disease and the remainder other chronic diseases.
Data were collected by trained doctors during face-to-face interviews, using standardized questionnaires. Data on the dialysis and comorbidities of each patient were obtained from medical records. The HD patients were assessed after the midweek dialysis sessions and the control group patients during a regular visit to their family physician. The following variables were selected:
Sociodemographic characteristics (gender, age, educational level, dwelling, income).
Social activities and integration (cohabitation, support during illness, friendship, hobby).
Mobility
The Timed Up and Go test, seconds.Citation17
Falls – at least one fall in the past 12 months (yes or no).
Neurosensory deficits – impairment of hearing and/or vision (yes or no).
Pain in any part of the body (yes or no).
Nutrition
Nutritional Health Checklist,Citation15 score 0–2 good, 3–5 moderate nutritional risk, ≥6 high nutritional risk.
Body mass index (BMI).
Constipation (yes or no).
Comorbidities – the Charlson comorbidity index (CCI) that includes age and 16 categories of comorbidities.Citation18,Citation19
Cognitive performance – Mini-Cognitive Assessment Instrument.Citation15
Activities of daily living – Katz ADL scale;Citation20 score >6 – patient is independent; score 0 – patient is very dependent.Citation15
Instrumental activities of daily living (IADL) – Lawton IADL scale.Citation21
Depressive symptoms – two question case-finding instrument.Citation22
Polypharmacy – number of different prescribed medications.
Informed consent was obtained from all patients included in the study and the study protocol was approved by the Ethical Committee of the Medical Faculty, Foča, University of East Sarajevo.
Continuous variables with a normal distribution were reported as mean ± SD and categorical variables as frequencies. The Student t-test and Kruskal–Wallis test were used to assess differences between continuous variables, and the χ2 test was used to assess differences between categorical variables. All analyses were performed using the SPSS statistical software package Version 10 (SPSS; (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. IBM Corp, Armonk, NY).
Results
The study involved 106 ESRD patients aged 71–86 years on regular HD and 300 patients without chronic kidney disease aged 70–91 years who were treated in primary health care. The sociodemographic data on the patients presented in showed no significant differences in age, gender and education level between the two groups. Similar proportions of patients from each group had a regular income (retirement) and their distribution according to housing and social activities was also similar. The majority of patients lived in a family, with spouses or children (79.3% of HD patients and 68.3% of controls) and only one from each group lived in an institution for the elderly. However, a lower percentage of the HD patients lived alone when compared with primary care patients (19.8% vs. 31.3%). Also, it was the family who usually supported patients of both groups during illness.
Table 1. Sociodemographic characteristics, social activities and integration of elderly hemodialysis patients and the control group of primary care patients without chronic kidney disease.
The use of the Nutritional Health Checklist showed a significant difference between the groups. Thus, more than half of the patients from the control group received good nutrition versus 16% of HD patients, and almost three times higher percentage of HD patients was at high nutritional risk than controls (). This correlates with the values for BMI. The distribution of patients according to BMI differed significantly between the two groups. None of the primary care patients were underweight as was the case for 5.7% of HD patients. A significantly higher proportion of HD patients suffered from constipation when compared to the controls (). However, similar percentage of HD and primary care patients reported pain in different parts of the body.
Table 2. Physical health, cognition and mental health of two groups of elderly patients.
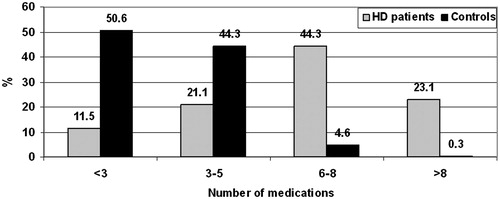
In the HD group, most patients had a CCI between 6 and 8 and the distribution of the two groups of patients according to the CCI differed significantly (). The Kruskal–Wallis test also showed a significant difference in CCI between the medians for HD patients and the controls [6 (range: 4–9) vs. 4 (range: 4–11); p < 0.0001]. All this explains why polypharmacy was more prevalent in HD patients than in those recruited in primary health care ().
The Mini-Cognitive Assessment Instrument was used to assess cognitive dysfunction and no significant difference was found between the groups (). However, a significantly higher percentage of HD patients gave an affirmative response to one or both of the questions in the simple two-question screening tool for depression as compared to the control group ().
A comparison of functional geriatric conditions between HD patients and patients without chronic kidney disease recruited in primary health care is presented in . There was no significant difference in impairment of activities of daily living (ADL) between the two groups as assessed by the Katz ADL scale. On the other hand, HD patients had significantly lower IADL scores than the controls. Namely, 25.5% of HD patients but only 9.7% of controls had an IADL score ≤6. Visual impairment was also more prevalent in HD patients than in the control group (74.5% vs. 36.3%). Mobility of patients was assessed by “The Timed Up and Go test”. Significantly worse mobility was found in HD patients than in controls. In addition, 45.7% of HD patients reported at least one fall in the previous 12 months versus 9.7% of patients from the control group ().
Table 3. Comparison of functional status between elderly hemodialysis patients and primary health care patients.
Discussion
CGA was carried out in two groups of elderly patients, one consisting of 106 HD patients and the other of 300 patients without chronic kidney disease recruited in primary health care, which formed the control. Patients on regular HD had significantly higher CCI, worse IADL scores and mobility and they reported more frequent falls, depression and impaired vision than patients from primary care. On the other hand, the two groups did not differ in sociodemographic characteristics, education level, regular income and accommodation, indicating that these factors might not have had an impact on the registered differences between the groups. Most patients in both groups lived in a family and only one from each group lived in an institution for the elderly. The life of the elderly in the family, rather than in institutions for the elderly, is a general characteristic of society in this region. Many of our patients had previously dwelt in villages but in old age they moved to be in towns with their children. Maybe just because they lived in a family, more than 60% of the patients from both groups socialized with friends. It was also the family that supported patients during illness or other needs. Nevertheless, a significant difference between the groups was found in the proportion of patients who lived alone. Understandably, a smaller percentage of HD patients lived alone when compared with the control group but the percentage of elderly HD patients living alone is similar to values found in other studies.Citation9,Citation13
Protein–energy malnutrition is common among HD patients and its prevalence and significance for patient outcomes have been widely investigated.Citation23–25 However, diverse methods have been used for assessment of nutrition in HD patients, which makes it difficult to compare the results. In the present study, the evaluation started with nutritional history performed with a simple screening tool for nutrition in older persons.Citation15 We found that 16% of HD patients had good nutrition, while 29.2% were at high nutritional risk. This differed significantly from the control group. All HD patients reported that ESRD influenced the kind and amount of food eaten, but 63% of them blamed the use of multiple medications. Despite these results, only 5.7% of HD patients were underweight, which was less than in some other HD populations.Citation26,Citation27 On the contrary, many HD patients were overweight (33%) or even obese (10.4%), so did not differ significantly from primary care patients. A high prevalence of overweight in the HD population has already been reported.Citation26–28 The general prevalence of overweight patients found here is consistent with data that overweight occurred in 60.7% of the adult population in Bosnia and HerzegovinaCitation29 and 54% in Serbia.Citation30 Although, reverse epidemiology regarding BMI and survival was reported for HD patients,Citation31 indicating increased mortality in those with low BMI and no increased mortality in overweight and obese HD patients, more recently obesity has been registered as an independent risk factor for cardiovascular morbidity and mortality in HD patients as for the general population.Citation32,Citation33 Therefore, close monitoring of body weight and maintenance of normal BMI in both HD and other elderly patients is necessary to prevent the adverse health consequences of obesity.
Elderly patients in the general population and especially those with ESRD are burdened with multiple comorbidities. Congestive heart disease (12.4%) and ischemic heart disease (12.4%) were the most frequent comorbidities in our HD patients and their prevalence was higher than in controls (7.7% and 6.3%). Diabetes was more frequent in patients from primary health care than in HD patients (14% vs. 10.5%) but the opposite was the case with cerebrovascular disease (1.3% vs. 10.5%). Prevalence of comorbidities in our patients differed from those reported in other studies, where diabetes was more frequent.Citation9,Citation34 The CCI was used to summarize medical comorbidity and median CCI for HD patients was significantly higher than for patients from primary care. None of the HD patients had CCI below 6, while 73% of primary care patients had CCI below 6. However, all HD patients obtained 2 points for chronic kidney disease and if these 2 points were subtracted a similar percentage of HD patients (77.3%) had CCI below 6 as the primary care patients. In this case the median value of CCI for HD patients would be 4 (range 4–8) as it was for controls (range 4–11) and the Kruskal–Wallis test did not find a significant difference between the groups (p = 0.466). It could be expected that in view of the similarity in the number of comorbidities, the number of medications used by patients in each group would be similar. However, only 14 (4.7%) patients from primary care used more than five medications, but 71 (67%) among the HD patients. That could be partly explained by the use of drugs necessary for prevention and treatment of different disorders accompanying ESRD, as well as by more frequent cardiovascular diseases.
Cognitive impairment is common in dialysis patientsCitation9,Citation35–37 but normal healthy aging is also accompanied by a decline in cognitive function.Citation38 Although there are several screening tests for assessing cognitive dysfunction, in the present study the Mini-Cognitive Assessment Instrument was used as a suitable test for the family physician. The results showed no significant difference between HD patients and patients from primary care in contrast to the findings obtained elsewhere.Citation9,Citation36 This could be explained by differences in comorbidities of the patients examined and the use of different instruments for cognitive function assessment in these studies and ours.
In order to determine the functional ability of patients, two instruments were used: the Katz ADL scale for assessment of basic ADL and the Lawton IADL scale for assessment of IADL. There was no significant difference in ADL impairment between HD patients and primary care patients. The majority of patients were able to perform all daily living activities without help or with a little help. Only two (1.9%) HD patients and seven (2.3%) patients treated in primary care had Katz score 0 that indicated severe dependence. Using ADL, Parlevliet et al.Citation13 reported significantly more independence in HD patients than in control patients. On the contrary, Soysal et al.Citation14 found significantly lower ADL scores in elderly HD patients compared to a control group consisting of elderly patients with normal kidney function hospitalized at a geriatric clinic. However, diabetes and congestive heart failure were more frequent in their participants than in our HD patient group. The most frequent impairment in daily activities in HD patients was an inability to bathe themselves or to move from bed to chair or to the toilet.
While HD patients were relatively independent with regard to ADL, they expressed difficulties in IADL. Most of them could use the telephone, take their medication and manage their own money without help, but for all other activities they needed assistance. A significantly higher percentage of HD patients had a Lawton score ≤6 in comparison to primary care patients and similar Lawton scores were recorded in other studies.Citation14,Citation39 This is in accordance with the finding that 9.4% of our HD patients used a walking device but none of the primary care patients. In addition, “The Timed Up and Go test” showed that 24.5% of HD patients needed more than 20 s to perform this test in contrast to 13% of elderly patients treated in primary health care (p < 0.0001). “The Timed Up and Go test” is not only a reliable test for quantifying functional mobility but is also reported to be associated with a high risk of falling in elderly patients suffering from different diseases including ESRD.Citation40,Citation41 Our results confirmed these data showing that significantly more HD patients fell in the previous 12 months in comparison to the primary care patients.
Depression is common in the elderly and especially among patients who suffer from chronic diseases.Citation42 Recently, we and others reported that depressive disorders were frequent in the elderly, especially in women, and pointed out the necessity of applying preventive strategies.Citation42,Citation43 Depression was also frequently reported in ESRD patients but its prevalence varied widely probably due to differences in sociodemographic characteristics of patients, modality of treatment, presence of different comorbidities.Citation11,Citation34,Citation44 We used the two-question case-finding instrument for depression proposed by Whooley et al.Citation22 This simple two-question screening tool has been used in several studies and confirmed as an instrument that can detect most cases of depression.Citation34,45 In our study, a significantly higher percentage of HD patients gave an affirmative response to one (33%) or both (31.1%) questions about depression when compared to primary care patients (6% and 14.7%, respectively). Such differences could be assumed bearing in mind more comorbidities and more frequent impairment of vision, mobility and, IADL in HD than in primary care patients.
One of the limitations of our study is its cross-sectional design. Therefore, there is the possibility that both persistent and transient disability were taken into account. Moreover, it was impossible to follow any changes of disorders over time that could lead to improvement or deterioration. In addition, the cross-sectional design made it impossible to assess the significance of disabilities on patient outcome. The second limitation is that our study was focused on comparison of CGA results between elderly HD patients and patients recruited in primary health care, but possible association between different CGA aspects and different uremic and metabolic disorders of HD patients was not examined. Nevertheless, it was of interest to apply CGA, a general geriatric multidimensional assessment, in parallel on patients on regular HD and in primary health care. Previous studies either applied CGA only in HD patientsCitation9 or compared HD patients with patients suffering from some other disease (cancer, Alzheimer) who were more severely ill than the dialysis patients.Citation13,Citation14 Despite these shortcomings, our study confirmed the view highlighted in a several other studies on the feasibility and significance of CGA in HD patients. As CGA encompasses not only medical issues but all aspects of a patient’s care, it enables both professionals and caregivers to identify problems that would not be revealed by standard assessment of HD, which is primarily directed to ESRD-associated disorders and quality of HD treatment. CGA helps to detect issues that should be treated and to identify disorders that could cause new issues and require preventive measures. Therefore, CGA provides an opportunity to improve the care and quality of life of different populations of elderly patients including those on maintenance HD.
In conclusion, several disabilities evaluated by CGA were more frequent in elderly HD patients than in elderly patients treated in primary health care. Many of these geriatric conditions would have remained undetected, if CGA had not been applied. Moreover, some of these conditions can be modified and thus should improve the quality of life, reduce the risk of new disorders and influence the quality of life and outcome for HD patients.
Declaration of interest
The authors declare no conflicts of interest. This work was conducted as a part of projects “Biomarkers in Nephrology” No. 175089 funded by the Ministry of Science, Education and Technological Development, Republic of Serbia.
References
- World Population Ageing 2013 (UN Report). Available at: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf. Accessed November 2014
- Jager KJ, van Dijk PC, Dekker FW, Stengel B, Simpson K, Briggs JD; ERA-EDTA Registry Committee. The epidemic of aging in renal replacement therapy: An update on elderly patients and their outcomes. Clin Nephrol. 2003;60(5):352–360
- Noordzij M, Kramer A, Diez JMA, et al. Renal replacement therapy in Europe: A summary of the 2011 ERA-EDTA Registry Annual Report. Clin Kidney J. 2014;7:227–238
- Letourneau I, Ouimet D, Dumont M, Pichette V, Leblanc M. Renal replacement in end-stage renal disease patients over 75 years old. Am J Nephrol. 2003;23(2):71–77
- US Renal Data System. USRDS 2008 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; 2008
- Verdalles U, Abad S, Aragoncillo I, et al. Factors predicting mortality in elderly patients on dialysis. Nephron Clin Pract. 2010;115(1):c28–c34
- Couchoud C, Labeeuw M, Moranne O, et al.; French Renal Epidemiology and Information Network (REIN) registry. A clinical score to predict 6-month prognosis in elderly patients starting dialysis for end-stage renal disease. Nephrol Dial Transplant. 2009;24(5):1553–1561
- Glaudet F, Hottelart C, Allard J, et al.; REIN Limousin. The clinical status and survival in elderly dialysis: Example of the oldest region of France. BMC Nephrol. 2013;14:131
- Cook WL, Jassal SV. Functional dependencies among the elderly on hemodialysis. Kidney Int. 2008;73(11):1289–1295
- Feng L, Yap KB, Yeoh LY, Ng TP. Kidney function and cognitive and functional decline in elderly adults: Findings from the Singapore longitudinal aging study. J Am Geriatr Soc. 2012;60(7):1208–1214
- Simic Ogrizovic S, Jovanovic D, Dopsaj V, et al. Could depression be a new branch of MIA syndrome? Clin Nephrol. 2009;71(2):164–172
- Aucella F, Stoico L, Cicchella A, et al. Comprehensive geriatric assessment in the hemodialysis elderly population. J Nephrol. 2012;25(Suppl 19):S85–S89
- Parlevliet JL, Buurman BM, Pannekeet MM, et al. Systematic comprehensive geriatric assessment in elderly patients on chronic dialysis: A cross-sectional comparative and feasibility study. BMC Nephrol. 2012;13:30
- Soysal P, Isik AT, Buyukaydin B, Kazancioglu R. A comparison of end-stage renal disease and Alzheimer's disease in the elderly through a comprehensive geriatric assessment. Int Urol Nephrol. 2014;46(8):1627–1632
- Elsawy B, Higgins KE. The geriatric assessment. Am Fam Physician. 2011;83(1):48–56
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–S266
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: The “get-up and go” test. Arch Phys Med Rehabil. 1986;67(6):387–389
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383
- Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919
- Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186
- Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12(7):439–445
- Kopple JD. Effect of nutrition on morbidity and mortality in maintenance dialysis patients. Am J Kidney Dis. 1994;24:1002–1009
- Carrero JJ, Chmielewski M, Axelsson J, et al. Muscle atrophy, inflammation and clinical outcome in incident and prevalent dialysis patients. Clin Nutr. 2008;27:557–564
- Lopes AA, Bragg-Gresham JL, Elder SJ, et al. Independent and joint associations of nutritional status indicators with mortality risk among chronic hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS). J Ren Nutr. 2010;20(4):224–234
- Lorenzo V, Martin M, Rufino M, et al. High prevalence of overweight in a stable Spanish hemodialysis population: A cross sectional study. J Ren Nutr. 2003;13(1):52–59
- Fleischmann E, Teal N, Dudley J, May W, Bower JD, Salahudeen AK. Influence of excess weight on mortality and hospital stay in 1346 hemodialysis patients. Kidney Int. 1999;55(4):1560–1567
- Djukanović L, Aksić-Miličević B, Antić M, et al. Epidemiology of end-stage renal disease and hemodialysis treatment in Serbia at the turn of the millennium. Hemodial Int. 2012;16(4):517–525
- WHO Global Health Observatory Data Repository [online database]. Geneva: World Health Organization; 2013. Available at: http://apps.who.int/gho/data/view.main. Accessed May 2013
- Republička stručna komisija za izradu i implementaciju vodiča u kliničkoj praksi. Gojaznost. Nacionalni vodič za lekare u primarnoj zdravstvenoj zaštiti. Medicinski fakultet Univerziteta u Beogradu: Beograd; 2004. [Serbian]
- Kalantar-Zadeh K. Causes and consequences of the reverse epidemiology of body mass index in dialysis patients. J Ren Nutr. 2005;15:142–147
- Kazory A, Klein A, Chalopin JM, Ducloux D, Courivaud C. Obesity and atherosclerotic events in chronic hemodialysis patients: A prospective study. Nephrol Dial Transplant. 2013;28(Suppl 4):iv188–iv194
- Okamoto T, Morimoto S, Ikenoue T, Furumatsu Y, Ichihara A. Visceral fat level is an independent risk factor for cardiovascular mortality in hemodialysis patients. Am J Nephrol. 2014;39(2):122–129
- Lopes AA, Bragg J, Young E, et al.; Dialysis Outcomes and Practice Patterns Study (DOPPS). Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. 2002;62(1):199–207
- Kurella M, Chertow GM, Luan J, et al. Cognitive impairment in chronic kidney disease. J Am Geriatr Soc. 2004;52:1863–1869
- Post JB, Morin KG, Sano BM, Jegede AB, Langhoff E, Spungen AM. Increased presence of cognitive impairment in hemodialysis patients in the absence of neurological events. Am J Nephrol. 2012;35:120–126
- Shavit L, Mikeladze I, Torem C, Slotki I. Mild hyponatremia is associated with functional and cognitive decline in chronic hemodialysis patients. Clin Nephrol. 2014;82(5):313–319
- Salthouse TA. When does age-related cognitive decline begin? Neurobiol Aging. 2009;30(4):507–514
- Janssen van Doorn K, Heylen M, Mets T, Verbeelen D. Evaluation of functional and mental state and quality of life in chronic hemodialysis patients. Int Urol Nephrol. 2004;36(2):263–267
- Rossier A, Pruijm M, Hannane D, Burnier M, Teta D. Incidence, complications and risk factors for severe falls in patients on maintenance hemodialysis. Nephrol Dial Transplant. 2012;27(1):352–357
- Soangra R, Lockhart TE, Lach J, Abdel-Rahman EM. Effects of hemodialysis therapy on sit-to-walk characteristics in end stage renal disease patients. Ann Biomed Eng. 2013;41(4):795–805
- Byers AL, Yaffe K, Covinsky KE, Friedman MB, Bruce ML. High occurrence of mood and anxiety disorders among older adults: The National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67(5):489–496
- Matović J, Pejović V, Račić M. Comprehensive geriatric assessment of patients in Health Centre Foča. Biomedicinska Istraživanja. 2013;4(1):13–25. [Serbian]
- Petković N, Ristić S, Simić-Ogrizović S. Depression in patients treated with regular hemodialysis. Biomedicinska Istraživanja. 2011;2(1):33–39. [Serbian]