Abstract
Objective: AA amyloidosis occurs in the setting of longstanding inflammation. An increased incidence of coronary artery disease (CAD) was noted in patients with chronic inflammatory disease (CID). Retrobulbar blood flow predicts future macrovascular events including CAD. Increase in carotid artery intima–media thickness is regarded as a marker for early atherosclerosis. The relationship between chronic inflammation and atherosclerosis is well known; however, the connection between amyloidosis-advanced CIDs and retrobulbar microvascular function and carotid intima–media thickness (CIMT) is unidentified. We aimed to investigate whether retrobulbar microcirculation and CIMT were impaired or not in amyloidosis-advanced CID patients compared to normal subjects. Methods: Fourteen patients with renal AA amyloidosis and a group of healthy volunteers were included in the study. Measurement of CIMT and retrobulbar blood flow velocities was performed with ultrasound scanner and color Doppler ultrasonography. Results: The CIMT of patients with renal amyloidosis was significantly thicker than that of the normal population (p < 0.001). The resistivity index of the ophthalmic artery (OA) of patients with renal amyloidosis was significantly higher than the study group (p < 0.001). Conclusion: This study demonstrates that accelerated atherosclerosis which can be shown by increased OA resistivity index and CIMT are found in amyloidal-related CID patients.
Introduction
Amyloidosis is a disorder in which soluble proteins change their secondary structures and deposit extracellularly in tissue as insoluble proteins disrupting the normal functions of the organs. The kidney is one of the most common organs of amyloid deposition in AL, AA, and several of the hereditary amyloidoses.Citation1 AA amyloidosis occurs in the setting of longstanding inflammation. The amyloidogenic protein is an N-terminal fragment of serum amyloid A (SAA) which is synthesized in the liver as an acute-phase reactant. AA amyloidosis is frequently seen in chronic infections, familial Mediterranean fever (FMF), inflammatory bowel disease and rheumatoid arthritis.Citation2
An increased incidence of coronary artery disease (CAD) events was noted in patients with chronic inflammatory disease (CID) despite having a lower burden of traditional cardiovascular (CV) risk factors.Citation3,Citation4 The excess CV risk observed in CID appears to be driven by the damaging effects of systemic inflammation on the vascular system, and thus the concept of inflammation as a CV risk factor has arisen.Citation5 Furthermore, both experimental and clinical studies in basic science have shown that inflammation has a role in mediating all stages of atherosclerosis and the thrombotic complications of this disease as well.Citation6,Citation7 Atherosclerosis is also a result of an active inflammatory and immune-mediated process in which leukocytes and soluble factors play a role in accelerating vessel pathology.Citation6,Citation7
Retrobulbar blood flow velocity measurement is used to examine the integrity of the eye microvascular circulation. It is apparent that structural and functional changes in different microvascular beds can provide key predictive information with respect to the development of future CV risk factors and events.Citation8 Experimental data support the concept that the microvascular beds of the eye and kidney represent preferential targets for systemic disease, where changes in vessel structure and function not only predict local complications but also CV and cerebrovascular events.Citation9 Retinopathy, in particular, is a preclinical marker for microvascular structural abnormalities in the retinal circulation that have been shown to independently predict future macrovascular events including stroke and coronary heart disease.Citation10–12
Carotid intima–media thickness (CIMT) is a measurement of the thickness of carotid artery walls, by which the progression of intima in relation to media thickness demonstrates atherosclerotic disease in humans.Citation13 CIMT is relatively easily obtainable and is strongly associated with future CV events.Citation14–17
The relationship between chronic inflammation and atherosclerosis is well known; however, the possible connection between amyloidosis-advanced CID and retinal microvascular function and CIMT is presently unidentified.
In the present study, we hypothesized that amyloid-advanced subclinical inflammation in CID patients might have more effect on retrobulbar microcirculation and increase the carotid IMT value. Therefore, we aimed to investigate whether retrobulbar microcirculation and carotid IMT were impaired in amyloidosis-advanced CID patients compared to normal control subjects.
Methods
Study population
Fourteen patients with biopsy-proven renal AA amyloidosis who presented to our nephrology outpatient clinic and a group of healthy volunteers were included in the study. Each patient was questioned for history of diabetes mellitus and CAD. None had any symptom of CAD. The patients with diabetes mellitus, stroke or congestive heart failure were excluded. Other exclusion criteria were the use of any vasoactive drugs, smoking, changes of ST segment or T wave specific for myocardial ischemia, Q wave and the left bundle branch block on ECG.
Biochemical assessment
Venous blood samples were taken from each patient and healthy volunteer after an overnight fasting and a 24-h period of abstinence from alcohol and vigorous physical exercise for the determination of serum biochemical parameters. Serum glucose was measured by a spectrophotometric method (Aeroset Automated Analyzer, Abbott Laboratories, Abbott, IL). Hemoglobin A1c, urea, creatinine, protein, albumin, alkaline phosphatase and parathyroid hormone values were also measured. Total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL) and triglyceride were also measured by enzymatic methods. Plasma levels of high sensitivity C-reactive protein (hs-CRP) were measured with a highly sensitive sandwich ELISA technique.
Echocardiographic examination
Echocardiographic examination was performed using GE Vivid 7 (Horten, Norway) echocardiography machine. Two-dimensional, M-mode and subsequent standard and pulsed tissue Doppler echocardiographic examinations were performed. Diastolic and systolic interventricular septal (IVS) thickness, posterior wall (PW) thickness and left ventricular end-diastolic diameter (LVEDD) and left ventricular end-systolic diameter (LVESD) were evaluated on the parasternal long-axis views. All measurements were done using M-mode images. Using transmitral Doppler image, early diastolic peak flow velocity (E), late diastolic peak flow velocity (A) and E/A ratio and E wave deceleration time (DT) were measured. The pulsed-wave Doppler mode was used for the Doppler tissue-imaging (DTI). Filters were set to exclude high-frequency signals, and the Nyquist limit was adjusted to a velocity range of −15 to 20 cm/s. Gains were minimized to allow for a clear tissue signal with minimal background noise. All DTI recordings were obtained during normal respiration. A 5-mm sample volume was placed on the lateral side of the mitral annulus at the apical 4-chamber view.Citation13 The velocities were recorded for 5–10 cardiac cycles at a sweep speed of 100 mm/s. Indexes of regional systolic function, namely, time velocity integral of myocardial systolic (Sm) wave, myocardial early (Em) and atrial (Am) peak velocities (cm/s) were measured. Isovolumic relaxation time (IVRT) was measured as the time interval between the end of Sm and the onset of Em. All diastolic parameters were measured in three consecutive cardiac cycles and averaged.Citation13 The same-blinded investigator performed the echocardiography, and two blinded cardiologists analyzed the echocardiogram recordings.
CIMT measurement
For measurement of CIMT, Logiq 5 ultrasound scanner (General Electric Medical Systems, Wallingford, CT) was used. Sonographic evaluations were performed by a single trained radiologist blinded to the patients’ data. The left common carotid artery was evaluated with the head in the midline position tilted slightly upward. A 7.5 MHz linear probe was placed so that the near and far walls were parallel to it and lumen diameter was maximized in the longitudinal plane. The CIMT was measured at about 1 cm proximal to the bifurcation of the common carotid artery. The CIMT was defined as the distance between the media–adventitia interface and the lumen–intima interface.Citation18 The coefficients of variation of intraobserver measurement of CIMT was 5.2%.
Retrobulbar blood flow velocities and resistivity index measurement
The right eye was examined. Color Doppler ultrasonography examinations were performed by the same operator using a Toshiba Aplio XU Ultrasound machine (Toshiba America Medical Systems, Inc., Tustin, CA) with a 12.5 MHz linear array probe. Subject positioning, ultrasound technique and arterial vessel location were described using a standardized protocol.Citation19 Subjects were achieved supine and provided fixation with their non-examined eye on a point marked on the ceiling directly above their head. The operator sat behind the subject’s head and lightly placed the ultrasound probe, coupled with gel on the closed eyelid of the study population. Ultrasound image quality was optimized and the machine settings were maintained constant for the remainder of the entire examination. Color imaging mode was used to locate the ophthalmic artery (OA) as it coursed along the medial side of the optic nerve. Color imaging mode was also applied both on the central retinal artery (CRA) and posterior ciliary artery (PCA). Pulsed Doppler recordings of flow velocity were made using a standard gate size of 1.5 mm with the Doppler angle maintained under 60° as previously identified.Citation20 Intraobserver of coefficient variation (CV) of measures was performed by the same operator on 10 separate measurements. The CV was then calculated from the results obtained from the 10 measurements using the formula: (100 × standard deviation/mean). CVs were calculated for the peak systolic velocity (PSV), the mean diastolic velocity (EDV) and the resistivity index (RI) ().
Table 1. Coefficient variation of retrobulbar blood flow and RI of study population.
Statistical analysis
Statistical analysis was performed using the SPSS software version 16 (Chicago, IL). The Chi-square test was used to compare variables in different groups. The variables were investigated using visual (histogram) and analytic methods (Kolmogorov–Smirnov/Shapiro–Wilk’s test) to determine whether or not they are normally distributed. Descriptive analyses were presented using medians and interquartile range for the non-normally distributed variables. The correlation coefficients and their significance were calculated using the Spearman test. The Mann–Whitney U test was performed to compare parameters between groups. A p value of less than 0.05 was considered to show statistically significant result.
Results
Study population
The median age of patients with renal amyloidosis was 40 (33–50) years, and eight were males and six were females. The median age of control group was 50 (38–54) years, and nine were males and five were females. There was no significant difference between ages of the two study groups (p = 0.26). There was no significant difference between the two study groups in terms of systolic (141 (129–147) vs. 115 (100–143); p = 0.17) and diastolic (80 (77–89) vs. 75 (70–90), p = 0.51) blood pressure values (). Body mass indexes (27.7 (26.1–31.8) vs. 27.4 (22.9–29.1), p = 0.63) and waist circumferences (92 (81–103) vs. 90 (75–101), p = 0.66) of the study subgroups were similar ().
Table 2. Demographic properties.
Biochemical assessment
All biochemical parameters except hs-crp levels were similar in the two study groups (). Hs-CRP levels were significantly higher in patients with renal amyloidosis than the normal population ().
Table 3. Biochemical assessment.
Echocardiographic examination
Interventricular septum, PW thickness, LVEDD, LVESD and left ventricular ejection fraction (EF) were similar in the two subgroups ().
Table 4. Echocardiographic parameters.
Standard and tissue Doppler echocardiographic analyses
When the diastolic function parameters achieved by tissue Doppler imaging, namely, mitral E wave, mitral A wave, mitral E deceleration time, lateral Em and lateral Am, IVRT and IVCT values were compared between the two groups, no significant difference was seen ().
CIMT measurement
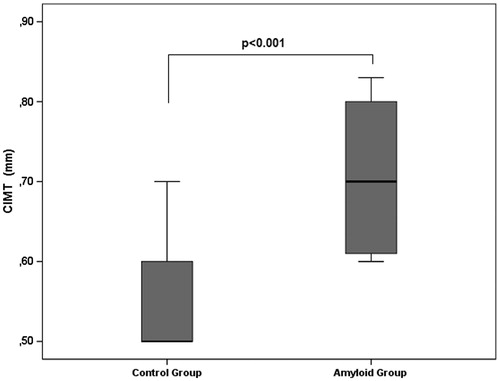
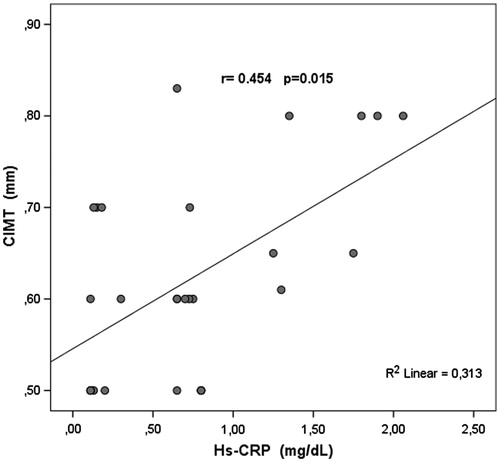
The CIMT of patients with renal amyloidosis was significantly thicker than that of the normal population (p < 0.001) (). The CIMT values were directly correlated with high sensitive CRP levels of the study population (p = 0.015) ().
Retrobulbar blood flow velocities and resistivity index measurement
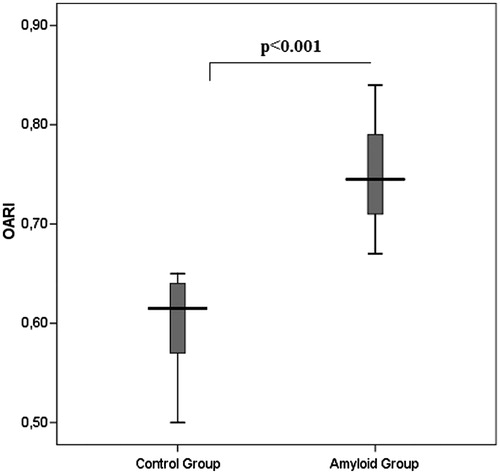
There is no significant difference between peak systolic flow (10.9 (10.2–12.6) vs. 12 (11.3–15.4), p = 0.09), end diastolic flow (2.7 (2–3.8) vs. 3.2 (2.9–3.9), p = 0.19) and resistivity index of CRA (0.75 (0.70–0.80) vs. 0.73 (0.71–0.77), p = 0.66) () of the two study groups. The PSV of PCA of patients with renal amyloidosis was significantly higher than that of the control group (13.9 (9.8--16.8) vs. 10.4 (8.4--12.1), p = 0.01) but the EDV (3.4 (2.7–4.9) vs. 4.2 (3.0–5.5), p = 0.19) () and RI (0.62 (0.52–0.70) vs. 0.70 (0.57–0.75), p = 0.42) of the PCA were not significantly different in both the groups. The EDV of the OA of patients with renal amyloidosis was significantly lower than the control group (8.5 (7.7--9.7) vs. 11.8 (8.8--16.4), p = 0.02). The peak systolic flow of the two groups was similar (32.9 (27.4–46.9) vs. 33.7 (31.2–36.7), p = 0.46) (). The RI of the OA of patients with renal amyloidosis was significantly higher than the control group (0.75 (0.71--0.79) vs. 0.62 (0.57--0.64), p < 0.001) ().
Table 5. Retrobulbar blood flow velocities.
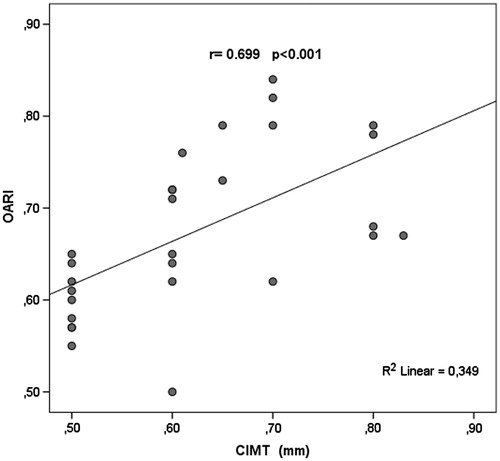
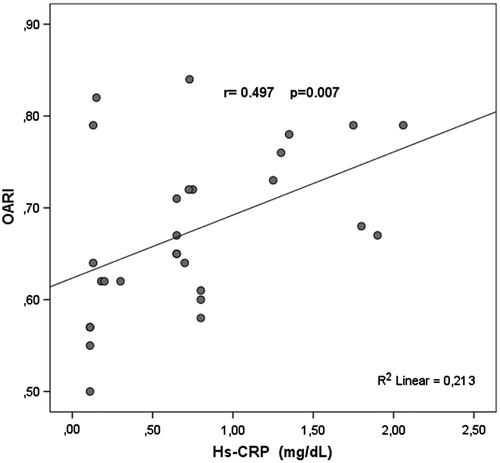
In the study population OARI values are currently correlated with CIMT (p < 0.001) (), and high OARI values were also associated with increased hs-CRP levels (p = 0.007) ().
Discussion
Secondary (AA) amyloidosis is characterized by the deposition of SAA protein, an acute phase reactant, in the extracellular tissue. AA amyloidosis can occur as a complication in many chronic inflammatory conditions, such as inflammatory bowel disease, rheumatoid arthritis, juvenile chronic polyarthritis, ankylosing spondylitis, familial Mediterranean fever, chronic infections and certain neoplasms.Citation21 Atherosclerosis has been shown to be associated with a systemic inflammatory state characterized by endothelial and blood cell activation as well as increased plasma concentration of inflammatory factors and endothelial dysfunction.Citation22
The structure of the coronary artery wall is dynamic. By increasing its external diameter, the internal lumen size can be maintained even in the development of atherosclerotic plaques.Citation23,Citation24 Several necropsy studies have reported very strong correlation between atherosclerosis in the carotid and coronary arteries.Citation25,Citation26 Increase in CIMT is regarded as a marker for early atherosclerosis.Citation27
Retinal blood flow velocity and resistivity index may also relate with microvascular function. In this line, ocular microvascular dysfunction assessed with retrobulbar blood flow measurement and due to amyloid-advanced CID occurs earlier than peripheral atherosclerosis, and it may be an early manifestation of developing advanced stage CV disease.Citation11
The present study aimed to investigate the risk of atherosclerosis in patients with renal AA amyloidosis by using the early predictors of atherosclerosis like CIMT and retrobulbar blood flow velocities alteration.
In our study, we compared CIMT of patients with biopsy-proven renal AA amyloidosis and normal population, and found that patients with renal amyloidosis had significantly higher CIMT values than the normal population.
Irie et al. concluded from their study that the addition of Cmax-IMT to conventional risk factors substantially improved the risk stratification for CAD.Citation28 Baldassarre et al. found that a risk-stratification strategy based on CIMT as an adjunct to the Framingham risk score was a rational approach to the prevention of CV disease.Citation29
The OA is the first main branch of the internal carotid artery. Changes in OA blood flow can demonstrate various vascular disorders, including carotid artery stenosis.Citation19 OA Doppler is also easy to accomplish due to the absence of ultrasonic obstacles.Citation30,Citation31 Retrobulbar flow velocities may alter with varying degrees of carotid stenosis.Citation32 Although carotid artery ultrasound analyzing can examine carotid stenosis, additional imaging methods like the velocities and pulsatility indices of the orbital arteries may maintain further information on the hemodynamics of the internal carotid artery.Citation33 OARI supplies important advantages due to the absence of ultrasound difficulties and the vertical angle, which differs from the parallel-signaling of the carotid artery.Citation34
High OARI may show the reduced arterial compliance caused by systemic atherosclerosis,Citation24 and it has clinical importance for the prediction of the coronary artery disease.
Grima et al. found that high OARI values were related to medium/high CV risk and thicker CIMT in HIV-1 infected patients.Citation35 On the other hand, Hu et al. in their study demonstrated that the flow velocities (systolic peak velocity and end-diastolic velocity) and pulsatility indices (resistivity index) in the ophthalmic and central retinal arteries decreased as the degree of carotid stenosis increased.Citation33
In the present study, the results were correlated with results of Grima’s study. We found that patients with renal AA amyloidosis had significantly higher OARI values than the normal population. There was no patient with obstructive carotid artery disease but CIMT of patients with renal amyloidosis was higher than the normal population.
Amyloidosis associated retrobulbar microvascular dysfunction may occur by various mechanisms: firstly, structural (intramural amyloid deposition in the vessel wall causing wall thickening and luminal narrowing), secondly, extravascular (extrinsic compression of the microvasculature from perivascular and interstitial amyloid deposits) and functional (autonomic and endothelial dysfunction).Citation12
On the other hand, inflammation is an important feature of atherosclerotic lesions.Citation6 Systemic inflammation as reflected by a rapid serum concentration of CRP is associated with enhanced risk of CV disease.Citation36 In our study, hsCRP levels were significantly higher in the patients with amyloid-related CID group than the control group. We also found that CIMT and OARI values of patients with renal AA amyloidosis were significantly higher than the normal population and hs-CRP levels correlated with CIMT and OARI values. Our result is in agreement with Libby and associates who observed that chronic inflammation, manifested by increased levels of hsCRP has been associated with atherogenesis.Citation7 A number of molecules involved in inflammation, endothelial damage or homeostasis have been shown as potential CV risk markers. Studies have also revealed that these markers in the atherosclerotic were also related to CIMT.
In conclusion, this study demonstrates that accelerated atherosclerosis which can be shown by increased OARI and CIMT are found in amyloidal-related CID patients and OARI measurement could be used as a screening method for detecting microvascular dysfunction in those patients.
Declaration of interest
All of the authors have no conflict of interest.
References
- Dember LM. Amyloidosis-associated kidney disease. J Am Soc Nephrol. 2006;17:3458–3471
- Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med. 1997;337:898–909
- Caliskan Z, Gokturk HS, Caliskan M, et al. Impaired coronary microvascular and left ventricular diastolic function in patients with inflammatory bowel disease. Microvasc Res. 2014;97:25–30
- Ciftci O, Yilmaz S, Topcu S, et al. Impaired coronary microvascular function and increased intima–media thickness in rheumatoid arthritis. Atherosclerosis. 2008;198:332–337
- Willerson JT, Ridker PM. Inflammation as a cardiovascular risk factor. Circulation. 2004;109:II2–II10
- Ross R. Atherosclerosis – An inflammatory disease. N Engl J Med. 1999;340:115–126
- Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–1143
- Touyz RM. Vascular remodeling, retinal arteries, and hypertension. Hypertension. 2007;50:603–604
- O’Rourke MF, Safar ME. Relationship between aortic stiffening and microvascular disease in brain and kidney: Cause and logic of therapy. Hypertension. 2005;46:200–204
- Cheung N, Wang JJ, Klein R, et al. Diabetic retinopathy and the risk of coronary heart disease: The Atherosclerosis Risk in Communities Study. Diabetes Care. 2007;30:1742–1746
- Cooper LS, Wong TY, Klein R, et al. Retinal microvascular abnormalities and MRI-defined subclinical cerebral infarction: The Atherosclerosis Risk in Communities Study. Stroke. 2006;37:82–86
- Dorbala S, Vangala D, Bruyere J Jr, et al. Coronary microvascular dysfunction is related to abnormalities in myocardial structure and function in cardiac amyloidosis. JACC Heart Fail. 2014;2:358–367
- Sohn DW, Chai IH, Lee DJ, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997;30:474–480
- Bots ML, Hofman A, Grobbee DE. Increased common carotid intima–media thickness. Adaptive response or a reflection of atherosclerosis? Findings from the Rotterdam Study. Stroke. 1997;28:2442–2447
- Bots ML, Hoes AW, Koudstaal PJ, et al. Common carotid intima–media thickness and risk of stroke and myocardial infarction: The Rotterdam Study. Circulation. 1997;96:1432–1437
- Hodis HN, Mack WJ, LaBree L, et al. The role of carotid arterial intima–media thickness in predicting clinical coronary events. Ann Intern Med. 1998;128:262–269
- Danad I, Raijmakers PG, Kamali P, et al. Carotid artery intima–media thickness, but not coronary artery calcium, predicts coronary vascular resistance in patients evaluated for coronary artery disease. Eur Heart J – Cardiovasc Imaging. 2012;13:317–323
- Persson J, Formgren J, Israelsson B, et al. Ultrasound determined intima–media thickness and atherosclerosis: direct and indirect validation. Arterioscler Thromb. 1994;14:261–264
- Tranquart F, Bergès O, Koskas P, et al. Color Doppler imaging of orbital vessels: Personal experience and literature review. J Clin Ultrasound. 2003;31:258–273
- Lockhart CJ, Gamble AJ, Rea D, et al. Nitric oxide modulation of ophthalmic artery blood flow velocity waveform morphology in healthy volunteers. Clin Sci (Lond). 2006;111:47–52
- Gertz MA, Kyle RA. Secondary systemic amyloidosis: Response and survival in 64 patients. Medicine (Baltimore). 1991;70:246–256
- Hansson GK, Libby P. The immune response in atherosclerosis: A double-edged sword. Nat Rev Immunol. 2006;6:508–519
- Davies MJ. Stability and instability: Two faces of coronary atherosclerosis. Circulation. 1996;84:2013–2020
- Glagov S, Weisenberd E, Zarins C, et al. Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med. 1987;316:1371–1375
- Young W, Gofman JW, Tandy R. The quantification of atherosclerosis? The extent of correlation of degrees of atherosclerosis within and between the coronary and cerebral vascular beds. Am J Cardiol. 1960;6:300–308
- Mitchell JRA, Schwartz CJ. Relationship between arterial disease in different sites: A study of the aorta and coronary carotid and iliac arteries. Br Med J. 1962;5288:1293–1301
- Persson J, Formgren J, Israelsson B, et al. Ultrasound determined intima–media thickness and atherosclerosis: direct and indirect validation. Arterioscler Thromb. 1994;14:261–264
- Irie Y, Katakami N, Kaneto H, et al. Maximum carotid intima–media thickness improves the prediction ability of coronary artery stenosis in type 2 diabetic patients without history of coronary artery disease. Atherosclerosis. 2012;221:438–444
- Baldassarre D, Hamsten A, Veglia F, et al. Measurements of carotid intima–media thickness and of interadventitia common carotid diameter improve prediction of cardiovascular events: Results of the IMPROVE (Carotid Intima–Media Thickness [IMT] and IMT-Progression as Predictors of Vascular Events in a High Risk European Population) study. J Am Coll Cardiol. 2012;60:1489–1499
- Michelson EL, Morganroth J, Nichols CW, et al. Retinal arteriolar changes as an indicator of coronary artery disease. Arch Intern Med. 1979;139:1139–1141
- Tedeschi-Reiner E, Strozzi M, Skoric B, Reiner Z. Relation of atherosclerotic changes in retinal arteries to the extent of coronary artery disease. Am J Cardiol. 2005;96:1107–1109
- Ho AC, Lieb WE, Flaharty PM, et al. Color Doppler imaging of the ocular ischemic syndrome. Ophthalmology. 1992;99:1453–1462
- Hu HH, Sheng WY, Yen MY, et al. Color Doppler imaging of orbital arteries for detection of carotid occlusive disease. Stroke. 1993;24:1196–1203
- Maruyoshi H, Kojima S, Kojima S, et al. Waveform of ophthalmic artery Doppler flow predicts the severity of systemic atherosclerosis. Circ J. 2010;74:1251–1256
- Grima P, Guido M, Chiavaroli R, et al. Comparison of intima–media thickness and ophthalmic artery resistance index for assessing subclinical atherosclerosis in HIV-1-infected patients. Cardiovasc Ultrasound. 2011;9:9
- Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–843