Abstract
Aim: To explore the underlying mechanism of low-molecular-weight heparin calcium therapy on Henoch–Schönlein purpura nephritis (HSPN). Methods: Eighty-nine children with severe HSPN were randomized into control group (treated with conventional therapy, n = 45) and treatment group (treated with conventional therapy plus low-molecular-weight heparin calcium, n = 44). The concentrations of plasma fibrinogen (Fg), d-dimer and fibrin degradation products (FDPs) were detected before and after treatment. The urinary red blood cell (RBC) and 24 h proteinuria were determined weekly for assessing the children’s kidney function. Results: Two groups were well-matched at baseline. After 8 weeks of treatment, the clinical outcomes of HSPN and outcome of proteinuria of the treatment group were better than the control group (p < 0.05); the content of Fg, d-dimer and FDP in plasma of the treatment group were lower than the control group (p < 0.05); but there was no difference about the curative effect of hematuria and the coagulation function between the two groups (p > 0.05). Conclusions: Fibrinolytic system may participate in the kidney injury of HSPN children and low-molecular-weight heparin calcium could correct blood hypercoagulability through inhibiting hyperfibrinolysis, and thus improving the blood supply of kidney.
Introduction
Henoch–Schönlein purpura (HSP) is a multisystem, self-limiting, nongranulomatous, autoimmune immunoglobulin A mediated small vessel vasculitis primarily affecting children, and it is characterized by a clinical tetrad of nonthrombocytopenic palpable purpura, abdominal pain, arthritis and renal involvement.Citation1 It is easy to repeated attack, especially the children and teenagers, and can also occur in adults. When renal parenchyma is damaged, HSP will turn into Henoch–Schönlein purpura nephritis (HSPN). HSPN is one of the most serious complications of HSP and the crucial factor of prognosis.Citation2,Citation3 The main pathogenesis of HSPN is the abnormal humoral immunityCitation4 accompanying with the participation of cytokines and inflammatory mediators. The severity of renal injury is the key factor determining the prognosis of HSPN.Citation5–7 However, the mechanism of renal injury is still not elucidated. Previous studies suggested that abnormality of coagulation and fibrinolytic system were associated with the pathogenesis of HSPN.Citation8,Citation9 Therefore, it is important to investigate the relationship between the abnormality of coagulation and fibrinolytic system and the renal injury, in order to take appropriate measures to prevent the occurrence of HSPN.
Heparin, as an effective anticoagulation, has been widely used in clinic, and data showed that it could reduce the incidence rate of HSPN in children when it was used before the occurring of kidney damage.Citation10 Therefore, we hypothesized that fibrinolytic system was associated with the renal injury of HSPN children, and the renal injury could be improved through heparin inhibiting the activation of fibrinolytic system.
In this study, we gave HSPN children in the treatment group low-molecular-weight heparin calcium on the basis of conventional therapy and detected the content of plasma fibrinogen (Fg), d-dimer and fibrinogen/fibrin degradation products (FDPs) in plasma before and after treatment, in order to explore the role of fibrinolytic system in the development of HSPN.
Materials and methods
Clinical data and therapy
Eighty-nine children with HSPN were enrolled from the urology department of the hospital from January 2007 to December 2012. The inclusion criteria were according to the standard the recommendation on clinical classification and treatment of children with glomerulopathy made by the Group of Nephrology, Society of Pediatrics, Chinese Medical Association in 2000. Cases were excluded with following conditions: patients undergoing hormone therapy, severe infected patients, patients with severe bleeding tendency, patients with leucopenia, pre-existing shock or HSP patients.
Eighty-nine patients were randomized into control group (n = 45) and treatment group (n = 44). Both the groups received the conventional therapy including oral vitamin C, compound rutin tablets, antihistamine cimetidine and antiallergic drugs loratadine and could be given appropriate antibiotic and hormone treatment. Besides, patients with the treatment group were given injection of low-molecular-weight heparin calcium (Hainan Unipul Pharmaceutical Co., Haikou, China) 100 U/kg/d once a day and continuing for 4 weeks, then dosed 50 U/kg/d for 4 weeks. Meanwhile, the control group was given the placebo. After 8 weeks, the therapy efficacy of both the groups was analyzed. Excellence: After treatment, clinical symptoms disappeared, urine protein turned to be negative and urine red blood cell (RBC) disappeared. Improvement: After treatment, clinical symptoms were alleviated, the level of urine protein and urine RBC were reduced. Failure: After treatment, clinical symptoms were not obviously improved, the level of urine protein and urine RBC was not obviously decreased.
Observation indices
During the treatment, we detected the urine RBC and 24 h urinary protein weekly to assess patients’ renal function. The coagulation function was also observed in both the groups including blood platelet count (PLT), activated partial thromboplastin time (APTT), prothrombin time (PT) and adverse reactions, such as rash, conjunctivitis and alopecia, in order to evaluate the security of low-molecular-weight heparin calcium therapy.
To evaluate the change of fibrinolytic system before and after treatment, all subjects were drawn peripheral venous blood in fasting state. Then the blood was centrifuged at 750 g for 15 min. The concentrations of Fg, d-dimer and FDP in plasma were determined by coagulometer (Sysmex, Kobe, Japan).
Data statistics
All data were analyzed by SPSS 16.0 software (SPSS Inc., Chicago, IL) and showed in (mean ± SD). Fisher’s Exact Test was used for the comparison of the clinical measurement data. Two-way ANOVA was performed to analyze the variations of each index at each time point, Bonferroni test was performed for comparison among the groups. t-Test was adopted for comparison of averages between groups at each time point. p < 0.05 was considered to be statistically significant.
Results
Baseline patient characteristics
The baseline clinical and laboratory characteristics were similar between the two groups, and no significant difference was found in all indices (gender, age, course, ISKDC pathological type, clinical classification, 24 h proteinuria quantification, serum albumin concentration, number of gross hematuria and Scr) between both the groups ().
Table1. Baseline patient characteristics in 89 children with severe HPSN.
Outcomes
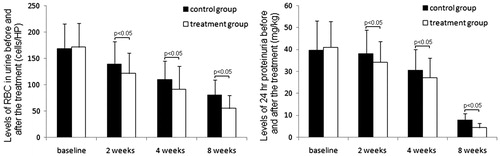
After 8-week treatment, the total effectiveness number (including the number of excellence and improvement) of HSPN in the treatment group was more than that in the control group (p < 0.05), the number of failure in treatment group was less than that in the control group (p < 0.05) (). Besides, the number of excellence and the number of improvement on proteinuria in the treatment group were also more than that in the control group (p < 0.05), but the outcome of hematuresis showed no difference (p > 0.05). The urine RBC and 24 h urinary protein in both the groups decreased; after 2, 4, 8 weeks of treatment, the two indices of the treatment group were less than the control group (p < 0.05) ().
Table 2. Comparisons of outcome of HSPN in the control and treatment groups.
The concentrations of Fg, d-dimer and FDP and adverse reactions
Before treatment, there was no difference on the levels of Fg, d-dimer and FDP (p > 0.05). After 8-week treatment, the concentrations of the three items in the treatment group were lower than the control group (p < 0.05) (). These results suggested that fibrinolytic system probably participated in the process of the renal injury of HSPN.
Table 3. Adverse reaction and concentration of plasma Fg, d-dimer and FDP before and after the treatment.
Adverse reactions: PT, APTT and PLT showed no obvious change (p > 0.05). During the treatment, there were no bleeding, allergy and other adverse reactions in the treatment group except that mild ecchymosis appeared in four children.
Discussion
Adjuvant therapies had been used in combination with conventional treatments, although there was no clear evidence of their efficacy.Citation11 In clinic, because the coagulation factors should be altered in the serum of children with HSP, substitution therapy with coagulation factors has also been considered.Citation12 Previous studies suggested that coagulation and fibrinolytic system participated in the development of HSPN. Therefore, we gave the HSPN children anticoagulation therapy based on conventional therapy in order to explore the characteristics of coagulation and fibrinolysis in the acute stage of children’s allergic purpura and the relationship between the coagulation and fibrinolysis and the renal injury. The results of this study showed that the curative effect of the treatment group was much better than the control group, especially on the therapy of proteinuria. It can be seen that low-molecular-weight heparin calcium can effectively alleviate the renal injury by its anticoagulate effect and protect the kidney function.
d-Dimer is the intermediate product in the process of blood coagulation and thrombosis, and the stable and specific degradation product of cross-linked fibrous protein. Rising level of d-dimer indicated the enhancement of secondary fibrinolytic activity, and can be regarded as a molecular marker of hypercoagulability and hyperfibrinolysis.Citation13–15 Zajadacz and Juszkiewicz reported that the level of d-dimer in plasma was increased, but there were two patients whose content of d-dimer was not related to the severity of disease, therefore they pointed out the possibility of coagulation disturbances in HSP with d-dimer rise (as well as decrease of plasma factor XIII and platelets described in relevant literature) should be taken into consideration.Citation16 Fg is a protein possessing coagulation function produced by liver, also the precursor of fibrin. When hypoxia, acidosis, allergy, infection and other factors triggered the extensive vascular endothelial injury, large quantity of coagulation agents was released and the level of Fg was also increased.Citation17 FDP is the degradation product of Fg, its clinical significance is to reflect the dissolve function of fibrin. Rising level of FDP can be seen in dissolve overactive of secondary fibrin, especially in hypercoagulable state or secondary kidney diseases.Citation18 In this study, after 8-week treatment, the levels of Fg, d-dimer and FDP in both the groups significantly declined and the levels of the treatment group were lower than the control group, which indicated that low-molecular-weight heparin calcium could significantly inhibit the activation of fibrinolytic system or hyperfibrinolysis, thus correcting the hypercoagulability, lowering blood viscosity and improving the blood-supply of kidney.Citation19 Moreover, heparin also could dissolve thrombus.Citation20,Citation21
Proteinuria is one of the main characterizations of kidney diseases, the results of this study showed that low-molecular-weight heparin calcium showed good curative effect on proteinuria. Fukui et al.Citation22 conducted one controlled clinical trial in pediatric patients with moderate systems of HSP, their research also showed that intravenous administration of factor XIII concentrate, 30–50 U/kg for days, was associated with significant improvements in the severity of proteinuria and hematuria compared with a non-treated group. Heparin calcium lowering the proteinuria may relate with its effect on reversing the incrassation of glomerular basement membrane. It could delay the development of HSPN through effectively inhibiting the hyperplasia of glomerular mesangial cells and renal matrix. While exploring how the heparin impeded murine lupus nephritis in mice, Hedberg et al.Citation23 discovered that heparin increased enzymatic degradation of nucleosomes and almost completely inhibited binding of nucleosomes to laminin and collagen, after heparin therapy, the nucleosomes–IgG compound on the murine glomerular basement membrane reduced significantly and the development of nephritis was delayed.
Though, we found low-molecular-weight heparin calcium treated the proteinuria effectively, it could not improve the hematuresis for its anticoagulant effect. In order to treat the hematuresis and proteinuria at the same time, the combining therapy of heparin calcium and other drugs should be considered in clinic. In addition, this study was also limited by the small number of subjects.
In summary, plasma fibrinolytic system possibly participates in the renal injury of HSPN, low-molecular-weight heparin calcium could through inhibiting the activation of fibrinolytic system or hyperfibrinolysis, correct the hypercoagulable state, lower blood viscosity and improve the blood-supply of kidney. Therefore, future research should pay more attention to the better therapy of low-molecular-weight heparin calcium, and the further well-designed prospective studies are needed to confirm the results.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Kurdi MS, Deva RS, Theerth KA. An interesting perioperative rendezvous with a case of Henoch–Schonlein purpura. Anesth Essays Res. 2014;8(3):404–406
- Johnson EF, Lehman JS, Wetter DA, et al. Henoch–Schonlein purpura and systemic disease in children: Retrospective study of clinical findings, histopathology, and direct immunofluorescence in 34 pediatric patients. Br J Dermatol. 2015;172(5):1358--1363
- Davin JC, Coppo R. Henoch–Schönlein purpura nephritis in children. Nat Rev Nephrol. 2014;10(10):563–573
- Pohl M. Henoch–Schönlein purpura nephritis. Pediatr Nephrol. 2015;30(2):245--252
- Almeida JL, Campos LM, Paim LB, et al. Renal involvement in Henoch–Schönlein purpura: A multivariate analysis of initial prognostic factors. J Pediatr. 2007;83(3):259–263
- Alfredo CS, Nunes NA, Len CA, et al. Henoch–Schönlein purpura: Recurrence and chronicity. J Pediatr. 2007;83(2):177–180
- Butani L, Morgenstern BZ. Long-term outcome in children after Henoch–Schönlein purpura nephritis. Clin Pediatr. 2007;46(6):505–511
- Prandota J, Pankow-Prandota L, Kotecki L. Impaired activation of the fibrinolytic system in children with Henoch–Schönlein purpura: Beneficial effect of hydrocortisone plus Sigma-aminocaproic acid therapy on disappearance rate of cutaneous vasculitis and fibrinolysis. Am J Ther. 2001;8(1):11–19
- Matayoshi T, Omi T, Sakai N, et al. Clinical significance of blood coagulation factor XIII activity in adult Henoch–Schönlein purpura. J Nippon Med Sch. 2013;80(4):268–278
- Xu M, Li XJ, Shi H, et al. Plasma TFPI level in children with Henoch–Schönlein purpura and the effect of low molecular weight heparin therapy. Zhonghua Er Ke Za Zhi. 2004;42(11):860–861
- Zaffanello M, Bruqnara M, Franchini M, Fanos V. Adjuvant treatments for Henoch–Schönlein purpura nephritis in children: A systematic review. Curr Ther Res Clin Exp. 2009;70(3):254–265
- Kaku Y, Nohara K, Honda S. Renal involvement in Henoch–Schönlein purpura: A multivariate analysis of prognostic factors. Kidney Int. 1998;53(6):1755–1759
- Shorr AF, Trotta RF, Alkins SA, et al. d-Dimer assay predicts mortality in critically ill patients without disseminated intravascular coagulation or venous thromboembolic disease. Intensive Care Med. 1999;25(2):207–210
- Yilmaz D, Kavakli K, Ozkayin N. The elevated markers of hypercoagulability in children with Henoch–Schönlein purpura nephritis. Pediatr Hematol Oncol. 2005;22(1):41–48
- Shi D, Xia T, Feng H, Cheng Q. Evaluating the diagnostic value of vWF:Ag, D–D and FDP in patients with acute cerebral infarction using ROC curves. Exp Ther Med. 2014;7(6):1573–1577
- Zajadacz B, Juszkiewicz A. Increased levels of plasma d-dimer in the course of Henoch–Schönlein purpura. Wiad Lek. 2005;58(9–10):581–583
- Sillesen M, Johansson PI, Rasmussen LS, et al. Fresh frozen plasma resuscitation attenuates platelet dysfunction compared with normal saline in a large animal model of multisystem trauma. J Trauma Acute Care Surg. 2014;76(4):998–1007
- Chan V, Yeung CK, Chan TK. Antithrombin III and fibrinogen degradation product (fragment E) in diabetic nephropathy. J Clin Pathol. 1982;35(6):661–666
- Moudgil A. Renal venous thrombosis in neonates. Curr Pediatr Rev. 2014;10(2):101–106
- Cetin Iİ, Ekici F, Ünal S, et al. Intracardiac thrombus in children: The fine equilibrium between the risk and the benefit. Pediatr Hematol Oncol. 2014;31(5):481–487
- Pincus KJ, Hynicka LM. Prophylaxis of thromboembolic events in patients with nephritic syndrome. Ann Pharmacother. 2013;47(5):725–734
- Fukui H, Kamitsuji H, Nagao T, et al. Clinical evaluation of a pasteurized factor XIII concentrate administration in Henoch–Schönlein purpura. Japanese Pediatric Group. Thromb Res. 1989;56(6):667–675
- Hedberg A, Fismen S, Fenton KA, et al. Heparin exerts a dual effect on murine lupus nephritis by enhancing enzymatic chromatin degradation and preventing chromatin binding in glomerular membranes. Arthritis Rheum. 2011;63(4):1065–1075