Abstract
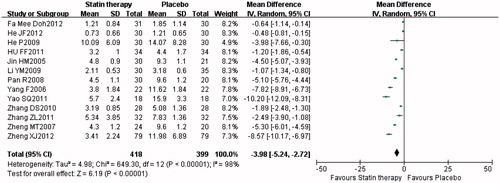
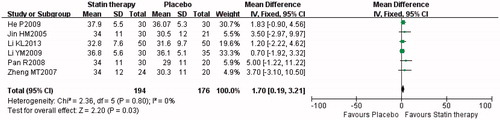
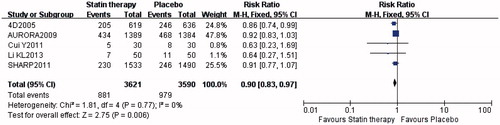
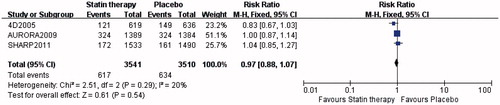
The effects of statin therapy in patients on maintenance dialysis remained uncertain. We conducted a meta-analysis to investigate the effects of statin on major clinical outcomes. We systematically searched Pubmed, Web of Science, Cochrane Library, Chinese National Knowledge Infrastructure, Wanfang and Chinese Technological Journal of Database for randomized controlled trials (RCTs). Criteria for inclusion were RCTs on statins therapy versus placebo, >3 months of follow-up. The outcomes were serum level of low density lipoprotein-cholesterol (LDL-C), high-density lipoprotein-cholesterol (HDL-C), triglyceride (TG), high-sensitivity C-reactive protein (hs-CRP) and albumin (ALB), all cardiac events, cardiovascular deaths and all-cause mortality. Twenty-one trials were identified, providing data for 8186 patients on maintenance dialysis. Statin therapy reduced LDL-C (weighted mean difference [WMD] = −0.74 mmol/L; 95%CI [−0.96, −0.52], p < 0.00001), TG (WMD = −0.36 mmol/L; 95%CI [−0.57, −0.14], p = 0.001), and hs-CRP (WMD = −3.98 mg/L; 95%CI [−5.24, −2.72], p < 0.00001), elevated HDL-C (WMD = 0.25 mmol/L; 95%CI [0.10, 0.39], p = 0.0007) and ALB (WMD = 1.70 g/L; 95%CI [0.19, 3.21], p = 0.03) significantly comparing with placebo. Statin therapy also had benefit in reducing all cardiac events (relative risk [RR] = 0.90; 95%CI [0.83, 0.97], p = 0.006), but had no effect on cardiovascular deaths (RR = 0.97; 95%CI [0.88, 1.07], p = 0.54) or all-cause mortality (RR = 0.98; 95%CI [0.93, 1.04], p = 0.49). In conclusion, statins had no impact on all-cause or cardiovascular mortality, while there was an overall significant improvement for dyslipidemia, hs-CRP, hypoalbuminemia and cardiovascular events in dialysis patients.
Introduction
Cardiovascular disease (CVD) is the leading cause of death in maintenance dialysis patients, the prevalence of CVD in those patients is 10–20 times higher than in the general population, after controlling for age, gender, race and diabetes.Citation1 Lipid abnormalities are a strong risk factor for CVD. Statins, a group of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors, have been demonstrated to improve these abnormalities. With benefit of reducing CVD risk greatly outweighing potential adverse effects, ACC/AHA recommended statin therapy for primary prevention in patients with CVD risk, especially in aging patients.Citation2 Many clinical trials suggested that statins reduce the risk of CVD in chronic kidney disease (CKD) population, while statin therapy in dialysis patients was quite controversial.Citation3 Unlike in the general population, some studies suggested that both hypercholesterolemia and hypocholesterolemia were associated with an excess risk of death in dialysis patients,Citation4 especially cardiovascular death, suggesting a “U-shape” survival curve.Citation5
Several clinical trials had been performed to figure out whether statins should be used in dialysis patients or not. The Study of Heart and Renal Protection (SHARP) suggested benefit, the lipid-lowering therapy safely reduced the incidence of major atherosclerotic events in patients with advanced CKD, but the study also included non-dialysis CKD patients.Citation6 The 4D study (Die Deutsche Diabetes Dialyse Studie)Citation7 and AURORA study (A Study to Evaluate the Use of Rosuvastatin in Subjects on Regular Hemodialysis: An Assessment of Survival and Cardiovascular Events)Citation8 both randomized patients on hemodialysis, but found no benefit in reducing cardiovascular death, non-fatal myocardial infarction or stroke. In this report, we systematically reviewed the data from randomized controlled trials (RCTs) to evaluate the impact of statin therapy on maintenance dialysis patients.
Methods
We searched Pubmed, Web of Science, Cochrane Library, and Chinese National Knowledge Infrastructure, Wanfang and VIP (Chinese Technological Journal of Database). The key words were: “randomized controlled trial (RCT) AND (one of: hemodialysis, peritoneal dialysis, dialysis) AND (one of: lipid-lowering therapy, statin, atorvastatin, simvastatin, fluvastatin, pravastatin, rosuvastatin, ezetimibe)”. All articles were identified by searching from June 1990 to May 2014. In addition, manual searches of selected specialty journals were performed to identify all pertinent literature. Qualitative reviews and published clinical trials were also searched. Criteria for study inclusion: RCTs of statins therapy versus placebo in patients on maintenance dialysis, with a minimum of 3 months of follow-up.
Two reviewers (Ling Sun and Luxi Zou) independently extracted the following information from each study: study population characteristics, experimental drug administration, duration of follow-up and outcomes. The individually recorded decisions of the two reviewers were compared, and any disagreements were resolved by a third reviewer (Bicheng Liu). The risk of bias for included trials was assessed according to the following aspects: Adequacy of randomization (selection bias), allocation concealment (selection bias), blinding (performance bias and detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias) and other bias.
We used the following outcomes to evaluate the benefit of statin therapy in maintenance dialysis patients: serum level of low density lipoprotein-cholesterol (LDL-C), high density lipoprotein-cholesterol (HDL-C), triglyceride (TG), high-sensitivity C-reactive protein (hs-CRP) and albumin (ALB), all cardiac events, cardiovascular deaths and all-cause mortality.
We conducted the analysis using the statistical package Review Manager, Version 5.3 (Cochrane Collaboration, Oxford, UK). We statistically analyzed the dichotomous outcomes using relative risk (RR) as the summary statistic. Continuous outcomes were analyzed using the weighted mean difference (WMD). The meta-analysis was performed using the fixed-effect or random-effect models depending on the absence or presence of significant heterogeneity. Heterogeneity was measured using chi-square (χ2) and I2 tests, and statistical significance was considered to be present when p < 0.05. In the absence of heterogeneity, the Mantel–Haenszel method of the fixed-effect model was used for the meta-analysis. Otherwise, the DerSimonian and Laird method for the random-effect model was selected. The RR and WMD with 95% CI were used to assess the treatment efficacy.
Results
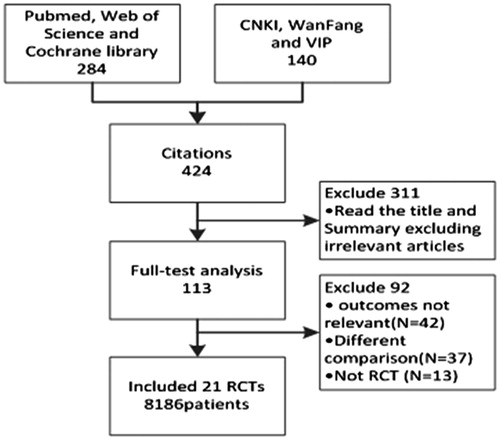
Our searches identified 424 studies. After the initial screen, 113 citations were selected for further review. Twenty-one trialsCitation6–26 with 8168 patients were included based on the criteria mentioned (). describes characteristics, baseline and outcomes of the 21 RCTs included in this report. describes the risk of bias for included studies.
Table 1. Characteristics, baseline and outcomes of included studies in the meta-analysis.
Table 2. Risk of bias for included studies.
Efficacy of statin therapy for LDL-C, HDL-C and TG
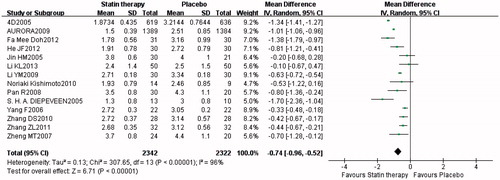
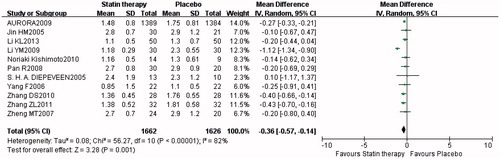
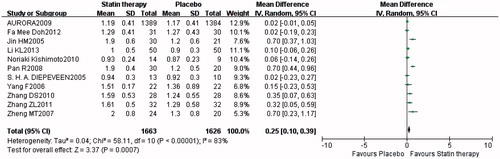
The efficacy of statin therapy for reducing LDL-C was assessed from 14 trials. The total number of patients was 4664. A significant difference was found between statin therapy and placebo groups, with a greater reducing LDL-C in the statin therapy group (WMD = −0.74 mmol/L; 95%CI [−0.96, −0.52], p < 0.00001), with significant heterogeneity between the trials (I2 = 96%, p < 0.00001) (). The efficacy of statin therapy for reducing TG was assessed from 11 trials. The total number of patients was 3288. A significant difference was found, with a greater reducing TG in the statin therapy group (WMD = −0.36 mmol/L; 95%CI [−0.57, −0.14], p = 0.001), with significant heterogeneity between the trials (I2 = 82%, p < 0.00001) (). The efficacy of statin therapy for reducing TG was assessed from 11 trials. The total number of patients was 3289. A significant difference was found, with a greater elevating HDL-C in the statin therapy group (WMD = 0.25 mmol/L; 95%CI [0.10, 0.39], p = 0.0007), also with significant heterogeneity between the trials (I2 = 83%, p < 0.00001) ().
Efficacy of statin therapy for hs-CRP
Thirteen trials provided data on the decrease in hs-CRP, as a protective effect of statin therapy, with 817 patients. There was a significant difference between statin therapy and placebo groups, a greater reducing hs-CRP in the statin therapy group (WMD = −3.98 mg/L; 95%CI [−5.24, −2.72], p < 0.00001), with significant heterogeneity between the trials (I2 = 98%, p < 0.00001) ().
Efficacy of statin therapy for ALB
Six trials provided data on the improvement in ALB as a protective effect of statin therapy, with 370 patients. There was a significant difference between statin therapy and placebo groups, with a greater elevating ALB in the statin therapy group (WMD = 1.70 g/L; 95%CI [0.19, 3.21], p = 0.03), and there was no significant heterogeneity between the trials (I2 = 0%, p = 0.80) ().
Efficacy of statin therapy for all cardiac events
Five trials provided data on reducing all cardiac events as a protective effect of statin therapy, with 7211 patients. A significant difference was found, with significantly lower all cardiac events in the statin therapy group (RR = 0.90; 95%CI [0.83, 0.97], p = 0.006), and there was no significant heterogeneity between the trials (I2 = 0%, p = 0.77) ().
Efficacy of statin therapy for cardiovascular deaths and all-cause mortality
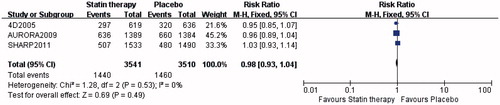
Three trials provided data on cardiovascular deaths and all-cause mortality as a protective effect of statin therapy, with 7051 patients. There was no significant difference in reducing cardiovascular deaths (RR = 0.97; 95%CI [0.88, 1.07], p = 0.54), and there was no significant heterogeneity between the trials (I2 = 20%, p = 0.29) (). There was also no significant difference in reducing all-cause mortality (RR = 0.98; 95%CI [0.93, 1.04], p = 0.49), and there was no significant heterogeneity between the trials (I2 = 0%, p = 0.53) ().
Discussion
Statins reduced major cardiovascular events, all-cause and cardiovascular mortality in persons with non-dialysis by 40–50%,Citation27 while the benefit of statin therapy in dialysis patients was still unclear. The 2013 clinical practice guideline of KDIGO suggested that statin/ezetimibe combination should not be initiated in adults with dialysis-dependent CKD, and statin/ezetimibe combination should be continued in adults already receiving these agents at the time of dialysis initiation.Citation28 Our results showed that statins reduced serum LDL-C and TG, and elevated serum HDL-C, improving dyslipidemia. Furthermore, statins reduced hs-CRP, elevated serum ALB, improving chronic inflammation and malnutrition in patients on dialysis. More importantly, we found that statin therapy reduced major cardiovascular events, although there was no benefit in reducing all-cause or cardiovascular mortality.
Dyslipidemia, both higher level of TC, TG, LDL-C and lower HDL-C could lead to atherosclerosis and CVD.Citation29 Shoji et al. found that the risk of incident myocardial infarction and cerebral infarction was positively associated with the serum non-HDL-C level and inversely with the serum HDL-C level in hemodialysis patients,Citation30 suggested the possibility that statin therapy could reduce the risk of atherosclerotic CVD in some subpopulations of hemodialysis patients. Risk of CVD deaths was determined by two factors: the risk of incident CVD, and the risk of fatality after CVD.Citation31 Some studies suggested higher cholesterol level was shown to predict a better survival in hemodialysis patients, because lower cholesterol level might be an index of protein-energy wasting, which was an important risk factor of fatality after CVD in hemodialysis patients.Citation30 The sub-analysis of 4DCitation32 and SHARPCitation6 showed that statins reduced the composite CVD endpoint significantly in a subgroup with higher cholesterol level, if LDL-C was higher than a certain level, and that the interaction between baseline total cholesterol and the treatment effect was significant. Our results also showed that statins reduced serum LDL-C and TG, elevated serum HDL-C, and reduced all cardiac events, which suggested that statin therapy might be beneficial even in dialysis patients if their lipid level were higher than a certain level.
In addition to improving dyslipidemia, statins also have multiple effects, including anti-inflammatory effect, anti-oxidation effect,Citation10,Citation24 anti-atherosclerotic effects and improving endothelial function.Citation14,Citation25 Dialysis patients accompanied with chronic low grade inflammation widely, which suppressed ALB synthesis and caused the development of malnutrition.Citation15 hs-CRP, an acute phase protein, was an independent risk factor for cardiovascular events in hemodialysis patients.Citation29 ALB correlated with hs-CRP inversely,Citation33 and hypoalbuminemia was also a powerful predictor for CVD events in dialysis patients.Citation34 Our results showed that statins reduced hs-CRP greatly and elevated ALB slightly but significantly (p = 0.03), indicated that statins improved chronic inflammatory state, which presented as hs-CRP reduced, then ALB elevated as a negative acute phase protein. Subsequently both reduction of hs-CRP and elevation of ALB might contribute to the reduction of CVD events.
Two meta-analysesCitation3,Citation35 about statin therapy in dialysis patients both concluded that statin therapy had no benefit in reducing cardiac events, while the studies included were all performed in Caucasian and Black people. In this report, RCTs performed in Chinese population were included, two of them mentioned the outcomes of cardiac events, which might lead to a different result that statin therapy could reduce all cardiac events significantly comparing with placebo. Shoji et al. conducted an cohort study among 45,390 Japanese hemodialysis patients to exam the relationship between serum lipids and incident CVD, and also got the similar conclusion that therapy for dyslipidemia might be benefit in reducing CVD events.Citation30 Although the KDIGO guidelineCitation28 was international guideline for lipid management, evidence specific to Chinese and other Asian populations was still lacking. Further studies were needed to build clinical practice guidelines for more specific subgroups of dialysis patients, such as Asian patients, and patients with higher non-HDL-C level.
Safety concerns had limited the use of statin therapy in dialysis patients, however, our meta-analysis did not show any significant increase of the adverse events, such as myalgia or myopathy, rhabdomyolysis, liver disease or cancer risk in the statins group compared with the placebo group.Citation6–8
The shortcomings of this analysis were that the population samples differed between the RCTs, with the inclusion of diabetic and non-diabetic subject, with prior CVD or without CVD persons, with races, with baseline of lipid level, with follow-up duration, as well as the inclusion of the different dialysis modalities, might lead to significant heterogeneity. The risk of bias was high in some of the included studies. Random sequence generation and allocation concealment was only reported in six studies (29%), and double blinding was unclear in eighteen studies (86%). Meanwhile it was impossible to meta-analyze all the data, because the studies included always present outcomes and comparisons without full statistical details.
Conclusion
This meta-analysis strengthened existing literature on the lack of survival benefits of statin therapy in dialysis patients. Statins corrected dyslipidemia, reduced hs-CRP, improved hypoalbuminemia and also reduced all cardiac events, while they did not impact all-cause or cardiovascular mortality in patients on maintenance dialysis. However, additional studies for Chinese, other Asian populations and specific subgroups of dialysis patients should be performed.
Acknowledgments
All authors had access to the data and participated in writing this manuscript.
Declaration of interest
The authors have no conflicts of interest to disclose.
References
- Paraskevas KI, Kotsikoris I, Koupidis SA, Tzovaras AA, Mikhailidis DP. Cardiovascular events in chronic dialysis patients: Emphasizing the importance of vascular disease prevention. Int Urol Nephrol. 2010;42:999–1006
- Robinson JG. Starting primary prevention earlier with statins. Am J Cardiol. 2014;114:1437–1442
- Green D, Ritchie JP, Kalra PA. Meta-analysis of lipid-lowering therapy in maintenance dialysis patients. Nephron Clin Pract. 2013;124:209–217
- Iseki K, Yamazato M, Tozawa M, Takishita S. Hypocholesterolemia is a significant predictor of death in a cohort of chronic hemodialysis patients. Kidney Int. 2002;61:1887–1893
- Seliger SL, Stehman-Breen CO. Are HMG-CoA reductase inhibitors underutilized in dialysis patients? Semin Dialysis. 2003;16:179–185
- Baigent C, Landray MJ, Reith C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): A randomised placebo-controlled trial. Lancet. 2011;377:2181–2192
- Wanner C, Krane V, Marz W, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. New Engl J Med. 2005;353:238–248
- Fellstroem BC, Jardine AG, Schmieder RE, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. New Engl J Med. 2009;360:1395–1407
- He JF, Wu J, He M, et al. Effect of atorvastatin on the levels of serum homocysteine and carotid intima-media thickness in patients with continuous ambulatory peritoneal dialysis. MMJC. 2012;14:4–6
- Yang F, Zhong B, Wang N, Jia HY, Li L. Effects of pravastatin on arterial elasticity in hemodialysis patients with type 2 diabetes. Chin J Blood Purif. 2006;5:137–140
- Cui Y, Yang J, Ju L, Ma PL, Li JH, Xie CY. Protective effection of statin therapy in CAPD Patients. Modern J Integr Tradit Chin Western Med. 2011;20:1103–1104
- Li KL, Xiong KL, Li ZH, et al. Protective effection of atorvastatin on cardiovascular in maintenance hemodialysis patients. Chin J Arterioscler. 2013;21:57–60
- Yao SQ, Hou L. Effect of atorvastatin on CRP and IL-6 in maintenance hemodialysis patients. Chin J Diffic Compl Cas. 2011;10:535–536
- Li YM, Xu FF, Chen WS. Effect of different doses of atorvastatin on cytokines and blood pressure during maintenance hemodialysis in patients with chronic renal failure. Zhe Jiang JITCWM. 2009;19:471–473
- Pan R. Effect of fluvastatin on CRP and d-dimer in maintenance hemodialysis patients. China Prac Med. 2008;3:53–54
- Zhang DS. The effect of fluvastation on microinflammation in patients subjected to maintenance hemodialysis. Guangzhou Med J. 2010;41:25–27
- Zheng MT. Effect of fluvastatin on CRP in maintenance hemodialysis patients. Chongqing Med. 2007;36:2012–2013
- Zheng XJ. Effect of Simvastatin in improving the micro-inflammatory state of patients treated with maintenance hemodialysis and its action mechanism. China Modern Doctor. 2012;50:52–54
- Jin HM, Zhu SJ, Shen GY. Effects of simvastatin on microinflammation and coagulation in hemodialysis patients. Chin J Blood Purif. 2005;4:437–439
- He P. The effect of different dose of simvastatin on microinflammation in maintenance hemodialysis patients. J Huaihai Med. 2009;27:538–539
- Zhang XD, Li H, Song J, Shi LH, Li Y. Study on the effect of Simvastatin on serum IL-6, IL-8, and TNF-α in maintenance hemodialysis patients. Acta Acad Med CPAF. 2011;20:337–339
- Zhang ZL, Wang YR. The effect of simvastatin on microinflammation in patients subjected to maintenance hemodialysis. Modern Prev Med. 2011;38:773–776
- Hu FF. The effect of simvastatin on microinflammation in maintenance hemodialysis patients. Clin Med. 2011;31:68–69
- Diepeveen SHA, Verhoeven G, Van der Palen J, et al. Effects of atorvastatin and vitamin E on lipoproteins and oxidative stress in dialysis patients: A randomised-controlled trial. J Int Med. 2005;257:438–445
- Kishimoto N, Hayashi T, Sakuma I, et al. A hydroxymethylglutaryl coenzyme a reductase inhibitor improves endothelial function within 7 days in patients with chronic hemodialysis. Int J Cardiol. 2010;145:21–26
- Doh FM, Chang T-I, Koo HM, et al. The effect of HMG-CoA reductase inhibitor on insulin resistance in patients undergoing peritoneal dialysis. Cardiovasc Drugs Ther. 2012;26:501–509
- Boaz M, Matas Z, Biro A, et al. Comparison of hemostatic factors and serum malondialdehyde as predictive factors for cardiovascular disease in hemodialysis patients. Am J Kidney Dis. 1999;34:438–444
- Wanner C, Tonelli M, Kidney Disease Improving Global Outcomes. KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014;85:1303--1309
- Ma KW, Greene EL, Raij L. Cardiovascular risk-factors in chronic-renal-failure and hemodialysis populations. Am J Kidney Dis. 1992;19:505–513
- Shoji T, Masakane I, Watanabe Y, Iseki K, Tsubakihara Y, Japanese Soc Dialysis T. Elevated non-high-density lipoprotein cholesterol (Non-HDL-C) predicts atherosclerotic cardiovascular events in hemodialysis patients. Clin J Am Soc Nephrol. 2011;6:1112–1120
- Shoji T. Serum lipids and prevention of atherosclerotic cardiovascular events in hemodialysis patients. Clin Exp Nephrol. 2014;18:257–260
- Maerz W, Genser B, Drechsler C, et al. Atorvastatin and low-density lipoprotein cholesterol in type 2 diabetes mellitus patients on hemodialysis. Clin J Am Soc Nephrol. 2011;6:1316–1325
- Zsom L, Zsom M, Fulop T, et al. Correlation of treatment time and ultrafiltration rate with serum albumin and c-reactive protein levels in patients with end-stage kidney disease receiving chronic maintenance hemodialysis: A cross-sectional study. Blood Purif. 2010;30:8–15
- Soriano S, Gonzalez L, Martin-Malo A, Rodriguez M, Aljama P. C-reactive protein and low albumin are predictors of morbidity and cardiovascular events in chronic kidney disease (CKD) 3–5 patients. Clin Nephrol. 2007;67:352–357
- Palmer SC, Navaneethan SD, Craig JC, et al. HMG CoA reductase inhibitors (statins) for dialysis patients. Cochrane Database Syst Rev. 2013;(9):CD004289