Abstract
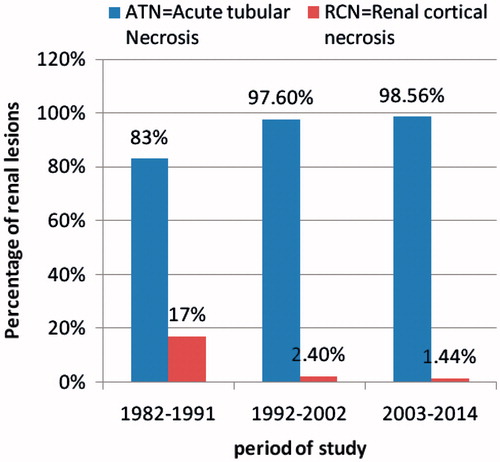
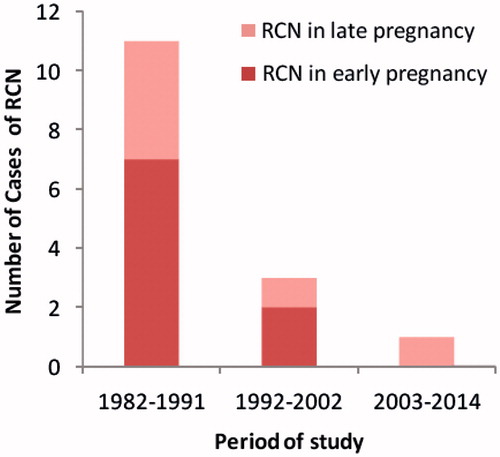
Rational: Obstetrical complications are the commonest causes of Renal Cortical Necrosis (RCN). However, the overall incidence of RCN in obstetric acute kidney injury in developing countries has been decreasing in recent years. Objective: The aim of this study was to evaluate the changing profile of RCN in obstetric AKI over the last three decades. Methods: This single center study included patients with biopsy proven renal cortical necrosis over a period of 32 years from 1982 to 2014. The diagnosis of RCN was suspected in patients with prolonged AKI (>4 weeks) with absolute anuria in the setting of hemorrhage, hypotension and sepsis; and was confirmed by renal biopsy. The changing pattern in the incidence, etiology and outcome of RCN in patients with obstetric AKI was compared in the three study periods, namely 1982–1991, 1992–2002 and 2003–2014. Results: Over a period of 32 years, RCN was diagnosed in 15/259(5.8%) cases of obstetric AKI. Diffuse and patchy cortical necrosis were noted in 8(53.3%) and 7(46.7%) patients, respectively. RCN occurred in 17%(11/65), 2.4%(3/125) and 1.44%(1/69) patients in 1982–1991, 1992–2002 and 2003–2014, respectively. Septic abortion was commonest cause of RCN in the first two study periods but no case was observed in last decade. The decrease in incidence of RCN over the three decades was statistically significant (p-value < 0.001). Maternal mortality decreased to zero in 2003–2014 from 72.7% in 1982–1991. Conclusions: The incidence of RCN in obstetric AKI in developing countries has declined low enough to label it as a disappearing entity.
Introduction
Renal cortical necrosis (RCN) is one of the most severe complications of acute kidney injury in pregnancy (P-AKI), which is characterized by patchy or diffuse ischemic destruction of the renal cortex. It occurs in 1.5–2% of cases of AKI in developed countries and more frequently (3–7%) in developing countries.Citation1–3 It is an important cause of obstetric AKI, with disastrous sequelae.Citation4,Citation5 Progression to end-stage renal disease is a rule in diffuse cortical necrosis.Citation5 Obstetric complications (septic abortion, puerperal sepsis, abruptio placentae, postpartum hemorrhage, and eclampsia) are the main (50–70%) causes of RCN in developing countries.Citation3,Citation6 The incidence of RCN ranges from 10 to 30% of cases of obstetric ARF, compared with only 5% of non-gravid patients.Citation7 In developed countries, RCN accounted for more than 20% of AKI during the third trimester of pregnancy.Citation1,Citation5 The reported incidence of RCN in P-AKI varies between 18 and 42.8% in different Indian studies.Citation3,Citation4,Citation6,Citation8–11 However, the overall incidence of RCN in P-AKI has decreased from 20–30% to 5% in the past two decades in developing countries.Citation12 The aim of present study was to evaluate the changing pattern of RCN in patients with obstetric AKI over the last three decades from a single centre.
Material and methods
The study was carried out in the Department of Nephrology, Institute of Medical Sciences, Sir Sunderlal Hospital, Banaras Hindu University, Varanasi; over a period of 32 years from 1982 to 2014. The demographic data, clinical presentation, underlying etiology, course of disease and outcome were recorded in individual patients with obstetric AKI. Absolute anuria was defined as no urine output or only a few drops of urine in 24 hours. Anuria was defined as urine output less than 100 mL/24 hours. Renal cortical necrosis was suspected in obstetric AKI in the presence of absolute anuria or oligoanuria persisting longer than 4 weeks in the setting of hypotension, sepsis, shock, and obstetric hemorrhage. Renal biopsy was done in the fifth or sixth week of persistent AKI to confirm the diagnosis of RCN. The obstetrical AKI patients with biopsy proven RCN were included in the present study. RCN was divided into two groups using standard histological criteria: (i) Complete cortical necrosis: Confluent global cortical destruction extending into the columns of Bertin. The thin rim of subcapsular and juxtamedullary tissue may be preserved. Irreversibility of renal function is the rule in complete cortical necrosis. (ii) Patchy cortical necrosis: Contiguous areas of cortical necrosis involving one-third to half of the entire cortical tissue. This form has potential for partial recovery of renal function.
Contrast enhanced computed tomography (CECT) scan showing uniform hypoattenuated subcapsular rim of cortex was considered for diagnosis of RCN. After 2000, diagnosis of RCN was confirmed in two patients using CECT scan of kidney ureter and bladder (KUB) region when CECT facilities were made available to our hospital. Data of 32 years were compiled and divided into three study periods (1982–1991, 1992–2002, and 2003–2014), to analyze the changing patterns in the incidence, etiology and outcome of RCN in patients with obstetric AKI.
Statistical analysis
Statistical analysis was done using SPSS16 software (Chicago, IL). For inter group comparisons, chi-square test was used. A p-value of <0.05 was considered significant.
Results
We studied 259 patients of obstetric AKI between 1982 and 2014. Their ages ranged between 18 and 45 years with mean age of 28.6 years. Over a period of 32 years, renal cortical necrosis was diagnosed in 15/259(5.8%) cases of obstetric AKI. Complete and patchy cortical necrosis were observed in 8(53.3%) and 7(46.7%) patients, respectively. The incidence of RCN in obstetric AKI decreased to 2.4% in 1992–2002 from 17% in 1982–1991. Renal cortical necrosis predominantly occurred following septic abortion in the first 10 years (1982–1991), but it virtually eliminated following post-abortal sepsis in the past decade (2003–2014). Of 4 cases of cortical necrosis in past two decades (1992–2014), diffuse and patchy lesions were noted in one and three patients, respectively (). RCN occurred in 17% (11/65), 2.4% (3/125) and 1.44% (1/69) patients in 1982–1991, 1992–2002, and 2003–2014, respectively (). Septic abortion was the commonest cause of RCN in the first two study periods. However, septic abortion associated RCN is not seen in third period (2003–2014) (). Puerperal sepsis (3), postpartum hemorrhage (1), abruptio placentae (1) and intrauterine death (1) were the causes of RCN in late pregnancy AKI. The decrease in incidence of RCN over the three decades was statistically significant (p-value < 0.001). In first two decades, the number of cases of RCN in early pregnancy was higher than that in late pregnancy, though the difference was not statistically significant (p = 0.918). The maternal mortality in obstetric RCN was 72.2% in 1982–1991. We noted mortality in 1 of 3 patients in 1992–2002 and no mortality in the last decade. Thus, mortality decreased to zero in 2003–2014 from 72.7% in 1982–1991. Partial return of renal function (Dialysis independent) was seen in two cases in our study. Two patients each with complete cortical necrosis progressed to ESRD in 1982–1991 and 1992–2002 ().
Table 1. Number of cases of RCN and obstetric AKI in early and late pregnancy in the three study periods.
Table 2. Outcome of patients with Renal Cortical Necrosis of all cases of obstetric AKI in the three study periods.
Discussion
Renal cortical necrosis (RCN) is a rare but catastrophic cause of acute kidney injury (AKI). It is usually caused by significantly diminished renal arterial perfusion secondary to vascular spasm, microvascular diseases or disseminated intravascular coagulation. In western countries, RCN accounts for ∼2% of all cases of acute renal failure.Citation1,Citation5,Citation13,Citation14 However, the incidence is higher (3–7%) in developing countries.Citation2,Citation4 It can be associated with a variety of conditions like sepsis, extensive burns, pancreatitis, snake bite and diabetic ketoacidosis; but the obstetric complications are the commonest causes of renal cortical necrosis (50–70%).Citation2–4,Citation12 Renal cortical necrosis is one of the most severe complications of AKI in pregnancy. Septic abortion, postpartum hemorrhage, abruptio placentae, puerperal sepsis and intrauterine death (IUD) are the major causes (50–70%) of RCN in developing countries.Citation2,Citation3,Citation12 The diagnosis is suspected in patients of obstetric AKI with prolonged (>4 weeks) anuria and/or oligoanuria in clinical setting of massive hemorrhage, sepsis, shock or disseminated intravascular coagulation. Because of the systemic nature of the illnesses causing RCN, the involvement is usually bilateral. Gold standard for confirmation of diagnosis is histopathological examination of renal tissue, showing ischemic necrosis of all the elements in the cortex (i.e., tubules, glomeruli and blood vessels). It can be complete or patchy. In complete RCN, global necrosis of renal cortex occurs, while patchy RCN involves ∼1/3–1/2 of the cortical tissue.Citation2,Citation4,Citation14 However, contrast enhanced computed tomography (CECT) scan has emerged as a good non-invasive modality of early diagnosis of RCN.Citation15 The characteristic finding is the presence of hypoattenuated subcapsular rim of renal cortex following contrast injection. In addition, a non-contrast CT scan is more sensitive in picking up cortical calcification. However, renal cortical calcification appears too late to be useful for diagnosis and is not even found in all cases. Other less invasive methods of diagnosis like MRI scan are useful alternatives.Citation15,Citation16 Recently, contrast enhanced ultrasound (CEUS) has been proposed as a useful modality for early diagnosis of cortical necrosis.Citation17
In the developed countries, RCN accounts for <2% of all the cases of AKI in adults and more than 20% of AKI during the third trimester of pregnancy.Citation1,Citation5,Citation13 This trend was noted in the western countries as early as the 1980s.Citation18,Citation19 Obstetric AKI-related RCN was observed in 26% (patchy 1% and diffuse 25%) of the cases in 1970s in North India.Citation6 RCN occurred in 18.6% of early pregnancy AKI and 37.8% of late pregnancy AKI.Citation6 In another Indian study, obstetric causes were responsible for RCN in 35/49(71%) patients with 19 cases (39%) due to septic abortion and 16(33%) due to late pregnancy AKI.Citation4 We have earlier observed RCN in 15/63(23.8%) patients of obstetric AKI.Citation3 The reported frequency of RCN in India and Pakistan varies between 23 and 42.8% of all patients with obstetric AKI (). Obstetric causes were responsible for RCN in 56% and 65% of patients in previous Indian studies.Citation3,Citation6 The incidence of RCN ranges from 10 to 30% of all cases of obstetric AKI compared with only 5% of non-gravid patients.Citation7 The incidence of RCN in obstetric AKI was 15.2% in our previous study.Citation12 Obstetrical causes accounted for 9% of the cases of cortical necrosis in patients with obstetric AKI in Pakistan.Citation20 Singhal et al. reported RCN in 9/21 (42.8%) of patients with septic abortion-associated acute renal failure.Citation11 The incidence of RCN has declined from 17% in 1982–1991 to 2.4% in 1992–2002 in obstetric AKI in our recent publication.Citation21 RCN was observed in 2.3% of patients in third trimester AKI in our another study.Citation22 Renal cortical necrosis occurred in 1.4% of patients with obstetric AKI in 2003–2014 in the present study. This decrease in incidence of RCN was probably due to decrease in postabortal sepsis associated AKI, aggressive blood transfusion in case of blood loss, and improved management of pregnancy specific complications like preeclampsia. However, neighboring country Pakistan still reports high incidence of RCN (20–25%) in obstetric AKI.Citation23–25 In septic abortion, endotoxin-mediated endothelial damage may lead to vascular thrombosis and subsequent renal ischemia and necrosis of renal cortex. RCN in placental abruption may be due to a combination of a hypercoagulable state, endothelial injury and intravascular thrombosis. Abruptio placenta is the most common obstetric cause of RCN accounting for 50–60% of cases in developed countries.Citation14,Citation26 Although obstetrical complications are the commonest causes of RCN in all the published series,Citation1–8 the spectrum of these complications causing RCN differ between developed and developing countries; with placental abruption and concealed hemorrhage being common in the former and sepsis(postabortal and puerperal sepsis) in the latter.Citation1,Citation2,Citation5,Citation12 RCN is very rare following septic abortion in developed countries but a common cause of obstetric RCN in India.Citation6,Citation8,Citation27 The reason for this discrepancy is the fact that abortions are commonly conducted by untrained persons under unhygienic settings accounting for a higher incidence of septic abortion and sepsis-related complications. Our study reveals that septic abortion was the most frequent cause of RCN, but has declined significantly over the past three decades. The possible pathogenic factors causing renal damage in our patients with renal cortical necrosis are: (1) either renal hypo-perfusion (blood loss, hypotension) or (2) endothelial injury either directly (eclampsia, placental abruption) or through release of various circulating factors such as endotoxin in patients with sepsis (septic abortion and puerperal sepsis). Based on these observations, the implementation of the specific measures for the prevention and effective management of sepsis and hemorrhagic complications of pregnancy will further reduce the incidence and severity of renal cortical necrosis in obstetric AKI in developing countries. The degree of renal function recovery after RCN depends upon the amount of viable cortical tissue following initial insult. It is assumed that juxtamedullary glomeruli (15–20% of total) escape destruction, even in the complete cortical necrosis and the early functional return is due to recovery of this nephron segment. These glomeruli undergo hypertrophy with the passage of time, leading to partial renal functional recovery. Two of our patients with RCN recovered sufficient renal function and became dialysis independent and they remain well for 5 and 8 years without need for dialysis.
Table 3. RCN in obstetric AKI from developing countries: comparative study.
The maternal mortality has been reported to be very high (86%) in RCN, mainly due to sepsis and uremic complications (pulmonary edema, hyperkalemia, uremic bleeding).Citation2,Citation3,Citation6 Early initiation of dialysis and improved management of sepsis have significantly reduced the mortality. In the present study, 8 of 11 patients died in 1982–1991 and 1 of 3 patients died in 1992–2002. There was no mortality in 2003–2014. We reported decrease in maternal mortality from 72% in 1984–1994 to 19% in 1995–2005 in patients with RCN in our recent publication.Citation12 Because of reduced mortality, surviving patients either had partial recovery of renal function (dialysis independent) or progressed to ESRD. The reasons for decreased mortality in RCN patients are improved medical facilities for care of sepsis and obstetric hemorrhage, availability of dialysis support and overall improved healthcare system. Thus, prognosis of RCN has improved in the recent years with increased patient survival and better renal outcomes.
In summary, with improvements in abortion practices; and antenatal and perinatal care, the incidence of RCN in obstetric AKI has decreased significantly over the last three decades. Still, because of the catastrophic sequelae, its prevention and aggressive management should always be important for the better renal outcome and prognosis of the patients.
Acknowledgements
This article is dedicated to my mentor and supervisor Prof. P.K. Srivastav M.D.,D.C.H., Former Professor, Department of General Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of paper.
References
- Grunfeld JP, Gaveval D, Bournerias F. Acute renal failure in pregnancy. Kidney Int. 1980;18:179–191
- Chugh KS, Jha V, Sakhuja V, Joshi K. Acute renal cortical necrosis – a study of 113 patients. Ren Fail. 1994;16:37–47
- Prakash J, Tripathi K, Pandey LK, Sahai S, Usha, Srivastava PK. Spectrum of renal cortical necrosis in acute renal failure in Eastern India. Postgrad Med J. 1995;71:208–210
- Chugh KS, Singhal PC, Kher VK, et al. Spectrum of acute cortical necrosis in Indian patients. Am J Med Sci. 1983;286(1):10–20
- Kleinknecht D, Grunfeld JP, Cia Gomez P, Moreau JF, Garcia-Torres R. Diagnostic procedures and long term progress in bilateral cortical necrosis. Kidney Int. 1973;4:390
- Chugh KS, Singhal PC, Sharma BK, et al. Acute renal failure of obstetric origin. Obstet Gynecol. 1976;48:642–646
- Brenner BM, Lazarus JM, ed. Acute Renal Failure. 2nd ed. New York: Churchill Livingstone; 1988
- Prakash J, Tripathi K, Usha, Pandey LK, Srivastava PK. Pregnancy related acute renal failure in eastern India. J Nephrol. 1995;8:214–218
- Prakash J, Tripathi K, Pandey LK, Gadela SR, Usha. Renal cortical necrosis in pregnancy-related acute renal failure. J Indian Med Assoc. 1996;94(6):227–229
- Ali SS, Rizvi SZ, Muzaffar S, Ahmad A, Ali A, Hassan SH. Renal cortical necrosis: A case series of nine patients & review of literature. J Ayub Med Coll Abbottabad. 2003;15(2):41–44
- Singhal PC, Kher V, Dhall GI, et al. Conservative vs surgical management of septic abortion with renal failure. Int J Gynaecol Obstet. 1982;20:189–194
- Prakash J, Vohra R, Wani IA, et al. Decreasing incidence of renal cortical necrosis in patients with acute renal failure in developing countries: A single-centre experience of 22 years from Eastern India. Nephrol Dial Transplant. 2007;22:1213–1217
- Walls J, Schoor WJ, Kerr DNS. Prolonged oliguria with survival in acute bilateral cortical necrosis. Brit Med J. 1968;4:220–222
- Lauler DP, Schreiner GE. Bilateral renal cortical necrosis. Am J Med. 1958;24:519–529
- Jordan J, Low R, Jeffrey RB Jr. CT findings in acute renal cortical necrosis. J Comput Assist Tomogr. 1990;14:155–156
- Francois M, Tostivint I, Mercadal L, Bellin MF, Izzedine H, Deray G. MR imaging features of acute bilateral renal cortical necrosis. Am J Kidney Dis. 2000;35:745–748
- McKay H, Ducharlet K, Temple F, Sutherland T. Contrast enhanced ultrasound (CEUS) in the diagnosis of post-partum bilateral renal cortical necrosis: A case report and review of the literature. Abdom Imaging. 2014;39(3):550–553
- Pertuiset N, Grünfeld JP. Acute renal failure in pregnancy. Baillieres Clin Obstet Gynaecol. 1994;8(2):333–351
- Silke B, Carmody M, Tormey WP, O'Dwyer WF, Fitzgerald GR, Donohue J. Acute renal failure in pregnancy – A decade of change. Ir Med J. 1980;73(5):191–193
- Naqvi R, Akhtar F, Ahmed E, et al. Acute renal failure of obstetric origin during 1994 at our centre. Renal Fail. 1996;18:681–683
- Prakash J, Kumar H, Sinha DK, et al. Acute renal failure in pregnancy in a developing country: Twenty years of experience. Renal Fail. 2006;28:309–313
- Prakash J, Niwas SS, Parekh A, et al. Acute kidney injury in late pregnancy in developing countries. Ren Fail. 2010;32(3):309–313
- Hassan I, Junejo AM, Dawani ML. Etiology and outcome of acute renal failure in pregnancy. J Coll Physicians Surg Pak. 2009;19(11):714–717
- Ansari MR, Laghari MS, Solangi KB. Acute renal failure in pregnancy: One year observational study at Liaquat University Hospital, Hyderabad. J Pak Med Assoc. 2008;58(2):61–64
- Ali A, Ali MA, Ali MU, Mohammad S. Hospital outcomes of obstetrical-related acute renal failure in a tertiary care teaching hospital. Ren Fail. 2011;33(3):285–290
- Jeong JY, Kim SH, Sim JS, et al. MR findings of renal cortical necrosis. J Comput Assist Tomogr. 2002;26:232–236
- Smith K, Browne JC, Shackman R, Wrong OM. Acute renal failure of obstetric origin. Lancet. 1965;12:351–354