Abstract
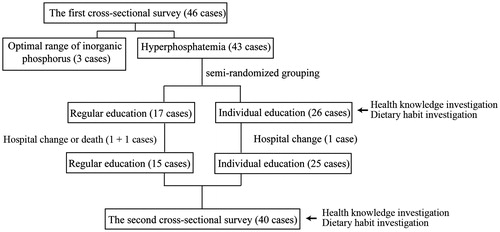
The Hakka are a sub-ethnicity with unique diet customs in South China. This study investigated hyperphosphatemia in hemodialysis patients in relation to the current Hakka dietary customs and explored health education patterns for hyperphosphatemia control. Two continuous cross-sectional surveys were conducted among the local patients on dialysis. After the first survey, the patients with hyperphosphatemia were semi-randomized into regular (group 1) and individual (group 2) education groups. Regular health education was conducted for both groups. In group 2, the awareness of health knowledge and dietary customs was investigated using a self-designed questionnaire. Based on the questionnaire, individual dietary guidance was given. The second survey was performed after 3 months. In the first survey, a high-phosphorus diet was found in all 46 patients with 43 (93.5%) diagnosed with hyperphosphatemia. In group 1 and group 2, 15 patients and 25 patients completed the two surveys, respectively. In group 1, no patient changed their dietary habits; however, in group 2, some patients did. The level of serum inorganic phosphorus in group 1 increased significantly. In group 2, the data remained stable; the awareness rate of chronic kidney disease–mineral and bone disorder (CKD–MBD) increased, and six patients with good compliance showed decreased serum inorganic phosphorus (p = 0.046). High-phosphorus dietary customs and low CKD–MBD knowledge awareness are important reasons for the difficulty in hyperphosphatemia control of patients on dialysis in the Hakka region. Individual health education led by medical staff might be helpful in hyperphosphatemia control, but the pattern still needs further exploration.
Introduction
Chronic kidney disease–mineral and bone disorder (CKD–MBD) is a common complication in patients on hemodialysis.Citation1 Hyperphosphatemia is an important and initiating factor of MBD.Citation2 Based on a recent epidemiological survey, the morbidity related to hyperphosphatemia was 55.6% in the dialysis population and 57.4% in patients on hemodialysis.Citation3 Hyperphosphatemia is associated with the geographical region, as evidenced by the diversity of hyperphosphatemia in China. The morbidity of hyperphosphatemia in South China is twice that in North China. This is associated with diet customs.Citation3 The actual situation in grassroots hospitals might be worse.Citation4
One of the adjuvant therapeutic strategies in hyperphosphatemia control is the reduction of phosphorus intake in the diet.Citation5,Citation6 Diet education is the best method to assure the knowledge and drive of dietary control, which are the key features for patient compliance.Citation7–9 Although good-compliance diet education could decrease the serum inorganic phosphorus by 0.72 mg/dL,Citation10 these experiences came from developed countries and regions with dieticians.Citation8,Citation11 Furthermore, the method of diet education, including health lessons, educational videos, food-containing phosphorus brochures and one-to-one individual health education, may not be appropriate for all populations.Citation11–13 How to carry out dietary management in medically underdeveloped areas still needs further study.
The Hakka, a unique Hakka-dialect speaking Han sub-ethnicity with a population of 65 million, reside mainly in the undeveloped areas of South China and have inherited unique social and dietary customs.Citation14 With a population of 23 million, the Hakka are one of the three largest sub-ethnicities in Guangdong. From 2009, the New Cooperative Medical Scheme for residents in rural areas partially covered the cost of hemodialysis,Citation15 contributing to the increase in the hemodialysis population in the Hakka areas of Guangdong. However, the undeveloped economy and poor medical facilities resulted in the frequent exclusion of the Hakka from medical investigations.Citation3
To explore the economical and efficient methods of local hyperphosphatemia control, the current status of hyperphosphatemia among the hemodialysis patients in the Hakka residential area of Guangdong was investigated. The health education and diet administration were performed by medical staff instead of a dietician.
Subjects and methods
Population
Wuhua County in Meizhou, Guangdong is one of the poorest provincial agricultural counties. Among the 1.2 million permanent residents, 99.9% are Hakkas.Citation16 Wuhua County Hospital is the only authorized facility where hemodialysis for all of the 102 patients in the county with end-stage renal disease is performed. There is no local clinical dietician, no examination of parathyroid hormone or Vitamin D, no additional phosphorus-decreasing oral drugs besides aluminum hydroxide and calcium carbonate and no standard system of dietary health education.
The first cross-sectional survey was performed with 46 maintenance hemodialysis patients (hemodialysis over 6 months) on 12 and 13 May 2014 at this hospital. The other 56 patients were not enrolled in this study because of their unwillingness to undergo a 3-month period of blood biochemical observation and change in dietary structure. All of the enrolled patients in this study are rural Hakkas, 46 ± 11 years old; 28 were male (69%), and 37 were female (80.4%). Among these cases, the median hemodialysis history was 35 months (10–136 months), and the median of hemodialysis times per double weeks was 4 times (2–6 times). The calcium concentration in the dialysate fluid was 1.5 mmol/L. The residual urine volume of 40 cases (87.0%) was <500 mL/day. No multiple myeloma or tuberculosis was found in these patients.
This study was licensed by the ethics review board of Wuhua People’s Hospital. Written informed consent was signed by all the involved patients.
Drug administration for hyperphosphatemia
A serum inorganic phosphorus over 5.5 mg/dL was diagnosed as hyperphosphatemia.Citation9 The treatment of hyperphosphatemia was based on the recommendation from the Chinese Medical Association and K/DOQI clinical practice guidelines:Citation17,Citation18 briefly, the oral administration of an aluminum hydroxide tablet with meals at most for 4 weeks, in cases of serum calcium over 10.2 mg/dL; the oral administration of calcium carbonate with meals in cases of serum calcium not >10.2 mg/dL; and discontinuation of vitamin D administration in cases of intact parathyroid hormone (iPTH) <150 pg/mL or calcium and phosphorus products over 55 mg2/dL2.
Health education
According to the data from the first cross-sectional survey, the patients were divided into a regular education group and an individual education group for the educational health intervention. The inclusive criterion was hyperphosphatemia (serum inorganic phosphorus that reached 5.5 mg/dL). To avoid the intervention for two groups of patients on the same day, semi-randomized grouping was performed. Namely, the patients on Monday, Wednesday and Friday were included in the individual education group, and the patients on the other days were included in the regular group.
The 3-month health education was conducted by a physician in-charge from Guangdong General Hospital who had received 5 days of training on kidney disease-related nutrition before this project. All of the participants were informed about the blood biochemical reports of MBD and received regular education. Based on this, bedside education was performed in the regular group by the doctor according to a special questionnaire to determine the patients’ awareness of CKD–MBD health knowledge and food structure. After the 3-month health education, a second cross-sectional survey was performed.
Statistical analysis
Measurement data were indicated by the mean ± SD or median (Q25–Q75), and enumeration data were indicated with the case number (%). The major results were presented as descriptive statistics. Comparison between the two groups was conducted using independent samples t test, χ2 test or the Fisher probabilistic method. Comparison between pre- and post-health education in the two groups was performed using paired Wilcoxon tests. The data were processed and analyzed by SPSS 19.0 software (Armonk, NY), with two-tailed p < 0.05 considered statistically significant.
Results
Baseline information of the first cross-sectional survey
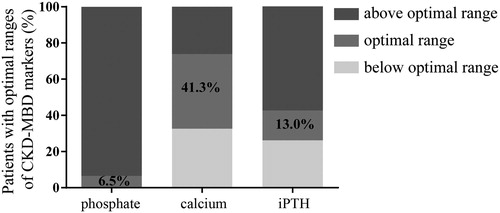
Among the 46 involved patients, hyperphosphatemia and high iPTH were the significant characteristics (). The mean serum inorganic phosphorus level was 73.9% higher and the median iPTH level was 32.5% higher than those in the hemodialysis population at the tertiary hospitals in developed regions in China.Citation3
Figure 1. Percentage of patients with optimal ranges of CKD-MBD markers. Based on the K/DOQI clinical practice guidelines, the optimal ranges of these serum indicators were designated as 3.5–5.5 mg/dL (1.13–1.78 mmol/L) for serum inorganic phosphorus, 8.4–9.5 mg/dL (2.1–2.37 mmol/L) for serum calcium and 150–300 pg/mL for iPTH.
The 43 patients with hyperphosphatemia were semi-randomly divided into the regular education group and individual education group, and 15 and 25 patients had completed the 3-month investigation, respectively (). The following results are based on the data of the 40 hyperphosphatemia cases that completed both surveys. No significant difference was found in the demographic and clinical features between the two groups ().
Table 1. Baseline information of the patients in the two groups before health education.
According to the results of the questionnaire in the individual education group, patient awareness of CKD–MBD knowledge was quite poor (). The customary Hakka diet consists of soup and high amounts of protein and sausage.Citation19,Citation20 Even in patients with end-stage renal disease, there was still a high proportion of patients with a high-phosphorus diet ().
Figure 3. Awareness rate of hyperphosphatemia and dietary habits pre- and post-health education. (a) (1) iPTH, (2) MBD, (3) phosphate binder use, (4) phosphate-rich diet, (5) egg yolk is phosphate-rich and (6) phosphorus removal from meat after boiling in water. (b) (1) less/no meat soup, (2) meat intake control, (3) less/no milk, (4) less/no soybeans, (5) eating egg removal of yolk and (6) meat intake after water boiling.
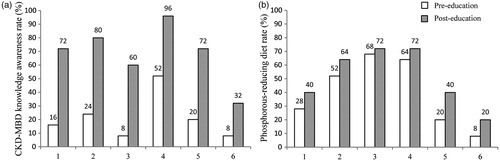
Role of individual dietary health education on the knowledge of hyperphosphatemia and change in dietary structure
The patients who received individual health education gained knowledge regarding parathyroid hormone and CKD–MBD. In addition, many of them could correctly take the phosphorus-decreasing drugs and learned to control the amount of phosphorous in their diet (). Some even changed their dietary habits (). Particularly, 6 patients who understood most of the items of CKD–MBD knowledge presented in the education had changed some of their dietary habits, a situation that was defined as good compliance.
Rice is the main source of carbohydrate for the Hakkas, and “LAO rice” is a conventional rice cooking method in agricultural Hakkas, through which phosphorus can be effectively removed. However, with the progression to a new lifestyle, this dietary habit has not been preserved. Even with health education, no patient would like to re-adopt this cooking method.
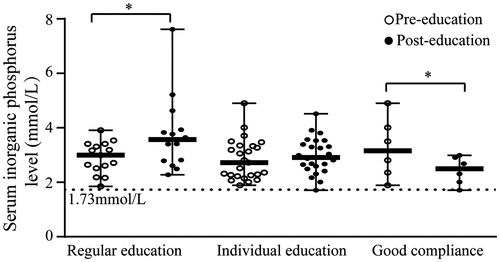
Effects of serum inorganic phosphorus and nutrition indicators by individual dietary health education
After the 3-month investigation, the serum inorganic phosphorus increased significantly in the regular education group, but remained stable in the individual educational group (). In the six patients with good compliance in the individual education group, the serum inorganic phosphorus decreased at the end of the 3-month health education program (), whereas the dry body weight (pre-education, 55.1 ± 10.8; post-education, 55.4 ± 9.3; p = 0.872) and serum albumin level (pre-education, 37.7 ± 2.7 g/L; post-education, 40.2 ± 7.2 g/L; p = 0.262) were stable.
Figure 4. Comparison of serum inorganic phosphorus levels between pre- and post-health education. Error bars indicate the median and range, and circles and dots indicate the serum inorganic phosphorus level pre- and post-health education. *Significant difference between pre- and post-education (p < 0.05).
Discussion
This is the first investigation of hyperphosphatemia among the hemodialysis population at a county hospital in the Hakka residential area. The results demonstrated the strikingly more severe local morbidity due to hyperphosphatemia, a finding that could be associated with the low awareness rate of MBD and local high-phosphorus dietary customs. Although regular dietary education was performed, hyperphosphatemia could not be decreased. On the other hand, the 3-month individual health education and dietary control improved the awareness of health knowledge and dietary structure. In some patients with good compliance, the serum inorganic phosphorus level decreased without malnutrition.
The high prevalence of hyperphosphatemia in this study represents the challenge faced by Hakka regions in China in the prevention and treatment of CKD–MBD. There might be multiple causative factors. First, the patients in this study are from the grassroots hospitals in undeveloped areas. Most of them could not financially support adequate hemodialysis. Among the 46 cases in the first cross-sectional survey, 73.9% patients had hemodialysis twice a week. Second, the poor local medical conditions could aggravate the hyperphosphatemia. Considering that the hypocalcemia in the Hakka residential area is lower than that in other areas,Citation3 the local patients may be more suitable to take the non-calcium phosphate binders that are not supplied in those areas. The lack of the examination of iPTH levels was another factor, which might not be able to effectively control hyperparathyroidism, therefore aggravating the hyperphosphatemia. In addition, young patients develop hyperphosphatemia more easily. The average age of the participants in this study was only 46 years. The younger hemodialysis patients might consume more protein-containing foods.Citation8 Finally, although dietary management is an economical way to lower blood phosphorus levels, it is difficult to carry out in Hakka regions. The dietary questionnaire form showed that the local Hakkas not only prefer a phosphate-rich diet, such as broth and meat, but also nearly avoid the conventional “LAO rice”, which is beneficial in hyperphosphatemia control. These modern Hakka dietary customs restrict the curative effect of health education. A curative effect of health education is often most dependent on educational background.Citation12 The patients in this study had not received high-quality education, and nearly no health education for the prevention of MBD had been provided before this program. Therefore, they had poor compliance with health education. At the end of 3 months of regular education, the serum inorganic phosphorus increased, demonstrating the unique challenge in local hyperphosphatemia control. On the other hand, the dietary problem could be solved through individual health education if the patients have good compliance. These results indicated the importance of exploring the reasonable health education pattern.
One of the characteristics of this study is the individual health education conducted by a physician with short-term nutrition training. The previous successful individual health education was conducted by dieticians.Citation11,Citation21,Citation22 In a well-developed hemodialysis center, there should be ∼1.5 full-time experienced kidney disease dieticians for each 130 patients.Citation12 Considering the lack of professional dieticians in the Hakka residential area, the pattern of medical staff training for health education conduction deserves further study.
The short intervention time is an insufficiency of this study. Based on the previous randomized controlled studies, only health education performed for over 4 months could demonstrate significant curative effects.Citation10 Because individual health education is labor-intensive work, this program was sustained only for 3 months. Obviously, the potential medical labor cost has become the barrier for physicians to conduct individual health education and appears to be much more serious where hemodialysis doctors are insufficient in Hakka regions. A long-term perspective for education in this field might be experienced nurses conducting health education.
It seemed impractical to use the completely randomized grouping in the bedside individual health education in hemodialysis patients. Although semi-randomized grouping could cause selection bias,Citation23 it reduced the human factors that may affect grouping. Furthermore, among the 102 patients on hemodialysis, only 46 were investigated, and this also caused selection bias. Other patients not enrolled in the study had even lower economic and educational levels; thus, we speculated worse complicated MBD conditions and more difficulties in conducting health education among them.
In conclusion, high-phosphorus dietary customs are a significant reason for hyperphosphatemia in the hemodialysis population in the Guangdong Hakka regions. Individual health education led by medical staff is an efficient method to correct hyperphosphatemia and deserves further research.
Acknowledgements
The authors thank the colleagues at the Second Division of Internal Medicine, Wuhua People’s Hospital for their assistance during this work.
Declaration of interest
The authors report no conflicts of interest. This work was supported by the National Clinical Key Specialty Construction Preparatory Projects; National Key Technology R&D Program (2011BAI10B08).
References
- Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208–2218
- Palmer SC, Hayen A, Macaskill P, et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: A systematic review and meta-analysis. JAMA. 2011;305:1119–1127
- Kong X, Zhang L, Zhang L, et al. Mineral and bone disorder in Chinese dialysis patients: A multicenter study. BMC Nephrol. 2012;13:116
- Xu J, Zhang YX, Yu XQ, et al. Lanthanum carbonate for the treatment of hyperphosphatemia in CKD 5D: Multicenter, double blind, randomized, controlled trial in mainland China. BMC Nephrol. 2013;14:29
- Cupisti A, Morelli E, D’Alessandro C, Lupetti S, Barsotti G. Phosphate control in chronic uremia: Don’t forget diet. J Nephrol. 2003;16:29–33
- Moe SM, Drüeke TB, Block GA, et al. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2009;113:S1–S130
- Sun CY, Chang KC, Chen SH, Chang CT, Wu MS. Patient education: An efficient adjuvant therapy for hyperphosphatemia in hemodialysis patients. Ren Fail. 2008;30:57–62
- Ford JC, Pope JF, Hunt AE, Gerald B. The effect of diet education on the laboratory values and knowledge of hemodialysis patients with hyperphosphatemia. J Ren Nutr. 2004;14:36–44
- Yokum D, Glass G, Cheung CF, Cunningham J, Fan S, Madden AM. Evaluation of a phosphate management protocol to achieve optimum serum phosphate levels in hemodialysis patients. J Ren Nutr. 2008;18:521–529
- Caldeira D, Amaral T, David C, Sampaio C. Educational strategies to reduce serum phosphorus in hyperphosphatemic patients with chronic kidney disease: Systematic review with meta-analysis. J Ren Nutr. 2011;21:285–294
- Cupisti A, D’Alessandro C, Baldi R, Barsotti G. Dietary habits and counseling focused on phosphate intake in hemodialysis patients with hyperphosphatemia. J Ren Nutr. 2004;14:220–225
- Blaszak RT, Mitsnefes MM, Ilyas M, Salman SD, Belcher SM, Brady DR. Hyperphosphatemia in children receiving peritoneal dialysis – An educational program. Pediatr Nephrol. 2005;20:967–971
- Poduval RD, Wolgemuth C, Ferrell J, Hammes MS. Hyperphosphatemia in dialysis patients: Is there a role for focused counseling. J Ren Nutr. 2003;13:219–223
- Shenghong Z, Dequan H. The spatial distribution and group characteristic of Chinese Hakkas. Study of Ethnics in Guangxi. 2007;4:80–85
- Liu ZH. Nephrology in china. Nat Rev Nephrol. 2013;9:523–528
- Zhan JG. The distribution of Hakka in Guangdong and its effect on Hakka culture development. Acad Search Truth Reality. 2012;4:87–93 (in Chinese)
- Wang L, Li GS, Liu ZH. Guidance for diagnosis and treatment of mineral and bone disorder in chronic kidney disease. Chin J Nephrol Dial Transplant. 2013;06:554–559 (in Chinese)
- National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42:S1–S201
- Luo SF. Inheritance and evolution of Hakka dietary culture. Jiangxi Food Industry. 2009;03:20–23 (in Chinese)
- Li B. On the impact of geographical environment upon Hakka food culture. J Jiaying Univ. 2009;03:113–115 (in Chinese)
- Ashurst IB, Dobbie H. A randomized controlled trial of an educational intervention to improve phosphate levels in hemodialysis patients. J Ren Nutr. 2003;13:267–274
- Reddy V, Symes F, Sethi N, et al. Dietitian-led education program to improve phosphate control in a single-center hemodialysis population. J Ren Nutr. 2009;19:314–320
- Harris AD, McGregor JC, Perencevich EN, et al. The use and interpretation of quasi-experimental studies in medical informatics. J Am Med Inform Assoc. 2006;13:16–23