Abstract
Background: The objective of this study was to assess clinical course and outcome of children with congenital anomalies of the kidney and urinary tract (CAKUT) who had an attack of acute poststreptococcal glomerulonephritis (PSGN). Method: Renal status including blood pressure, proteinuria and glomerular filtration rate was retrospectively analyzed in five children with CAKUT and PSGN at the presentation and during the follow up. Results: In the period 2004–2013, 678 patients were diagnosed and recruited in our CAKUT cohort. During this period, 188 patients were hospitalized with the diagnosis of PSGN. A total of five patients had CAKUT and an episode of PSGN (2.6%). Analysis of the follow-up data revealed that three children fully recovered (bilateral vesicoureteral reflux n = 1, ectopic/hypodysplastic kidney n = 1, ureteropelvic junction obstruction n = 1). One child with bilateral hypodysplasia had progressive worsening of the renal function and has been prepared for renal replacement therapy. Another child with single kidney has stable renal function but has significant rising proteinuria, which was not evident on the routine analysis 2 months before the attack of PSGN. Conclusion: Poststreptococcal glomerulonephritis in children is generally benign disease with low mortality in acute stage and excellent medium and long-term prognosis. We analyzed our series of PSGN patients and found that 2.6% had anomaly of the urinary tract. The unfavorable outcome was noted in children with single kidney and bilateral renal impairment.
Introduction
Congenital anomalies of the kidney and urinary tract (CAKUT) are the major cause of chronic kidney disease (CKD) and end stage renal failure (ESRD) in children and young adults.Citation1–4 The prevalence of CAKUT varies between 3 and 6 per 1000 births. The prognosis is dependent on the severity of malformations (unilateral, bilateral), presence of hypoplasia, dysplasia, and associated urinary tract infections. Traditional risk factors for CKD progression are also important such as hypertension, hyperlipidemia, smoking, nephrotoxic agents, obesity.Citation1,Citation4 CAKUT patients usually have slower progression to ESRD than those with glomerulonephritis. There are few reports on CAKUT patients with poststreptococcal glomerulonephritis (PSGN). Our community has high prevalence of acute postinfectious glomerulonephritis. We analyzed the prevalence, clinical features and outcomes of children with CAKUT and an episode of PSGN.
Patients and methods
We reviewed the in- and out-patient records of the patients who had been diagnosed and treated at the University Children’s Hospital Skopje in the period from 2004 to 2013 under diagnostic categories CAKUT and glomerulonephritis. As this was a retrospective study informed consent was not mandatory.
CAKUT was diagnosed with standard imaging methods: kidney and bladder ultrasound, cystography, radionucleotide scans, intravenous urography and in rare cases MRI urography and cystoscopy. All children had evaluation of renal function, blood pressure and proteinuria at baseline and during the follow up. We also noted the extrarenal manifestations or other conditions (e.g., infections, low birth parameters, diabetes) which may affect the long-term outcome of these children.
PSGN was diagnosed on the basis of established clinical and serological criteria. These included history for previous streptococcal infection (pharyngitis/angina, pyodermia), latent period from initial infection to the onset of nephritic symptoms (>1 week and <4 weeks), positive throat or skin culture for streptococcus pyogenes, significant/rising titer of streptococcal antibodies (ASTO >250 U/L) and transitory hypocomplementemia (C3 <0.70 g/L).Citation5 If the patient fulfilled these criteria renal biopsy was not mandatory. Ultrasound examination was performed to all children with PSGN on admission. Our practice is to admit to the hospital all children with PSGN until resolution of nephritic symptoms.
Results
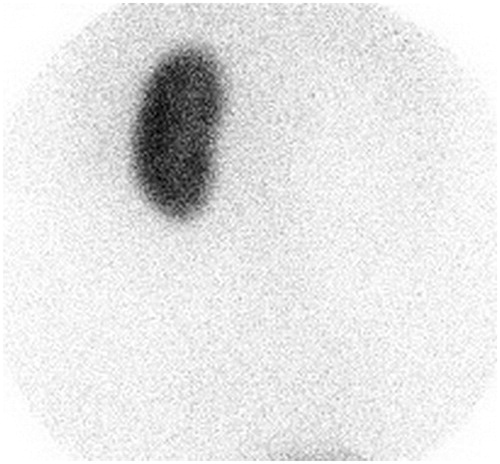
In the period 2004–2013, 678 patients were diagnosed and recruited in our CAKUT cohort. Our search in “other conditions” resulted in detection of six patients with “glomerulonephritis”. One patient was excluded since he had IgA glomerulonephritis. In the same period, 188 patients were hospitalized with the diagnosis of PSGN. No additional patients with CAKUT were detected among hospitalized PSGN patients. Thus, a total of five patients had CAKUT and an episode of PSGN (2.6% of all PSGN patients). The basic demographic data and clinical features of these five patients are presented in . Patient No. 1 had an acute nephritic syndrome after pharyngitis, low C3 complement and elevated ASTO titer (666 U/L). He had increased serum creatinine and proteinuria, which peaked to 3.7 g/d. Renal biopsy was avoided as the ultrasound examination revealed a single left kidney. His nephritic signs resolved, but significant proteinuria remained at the last follow up. An Tc99mDMSA scan confirmed the presence of a single kidney (). It is of note, that this patient had routine urinalysis without proteinuria 2 months before the PSGN attack.
Table 1. Clinical and laboratory features of five patients with CAKUT who suffered from acute poststreptococcal glomerulonephritis.
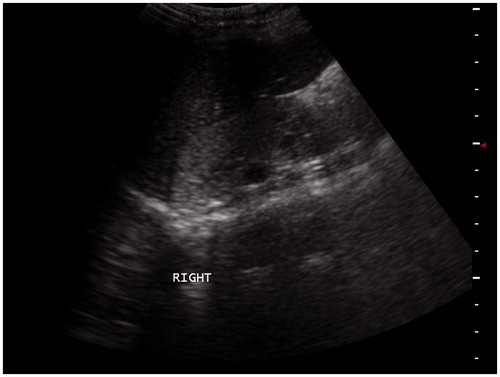
Patient No. 2 presented with acute renal failure in the intensive care unit. She had extensive pyodermia on the lower extremities. Ultrasound examination revealed bilateral small kidneys with irregular contour, hyperechogenic parenchyma with loss of corticomedullary differentiation consistent with bilateral hypodysplasia (). She was treated conservatively: within 3 weeks nephritic signs improved and her creatinine decreased at 118 μmol/L. Voiding cystography did not detect vesicoureteral reflux. Seven years later her creatinine was 413 μmol/L.
Figure 2. Ultrasound scan reveals small right kidney with hyperechogenic parenchyma and loss of corticomedullary differentiation.
Patient No. 3 is a female who was diagnosed with bilateral vesicoureteral reflux and right reflux nephropathy at the age of 2. Two years later, she came with mild nephritic signs after streptococcal pharyngitis. She had a steady recovery. Her renal function, blood pressure and proteinuria were stable the follow up of 9 years.
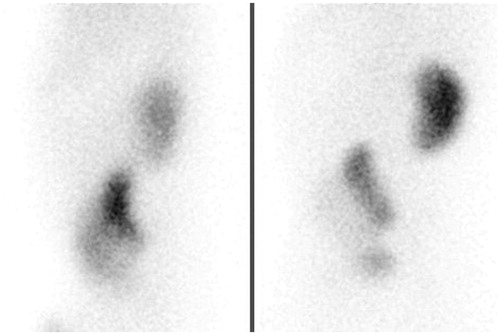
Patient No. 4 had typical postinfectious glomerulonephritis after pyodermia. Ultrasound examination revealed pelvic ectopy of the left kidney, which was smaller, malrotated with irregular contour. He had a complete recovery. Tc99mDMSA scan revealed that the right kidney was smaller compared to the left one and had decreased relative uptake of the radionuclide (40%) (). His blood pressure, proteinuria and GFR were within referent limits during the follow up.
Patient No. 5 was diagnosed left ureteropelvic junction obstruction at the age of four after having an episode of gross painful hematuria. He was managed conservatively. At the age of 12, he had an episode of painless hematuria, which was initially attributed to his ureteropelvic junction obstruction. As the gross hematuria persisted, his urinary red blood cells showed 100% dysmorphy, ASTO titers rose, transitory hypocomplementemia was confirmed, and the PSGN was obvious. Five years after the PSGN episode he does not show hematuria, his blood pressure, renal function and proteinuria are within referent values.
Discussion
Herein, we present five children with CAKUT and poststreptococcal glomerulonephritis. In three children CAKUT was diagnosed during the episode of PSGN. One child with severe PSGN was found to have single kidney. The second child had acute renal failure and the ultrasound examination revealed bilateral hypodysplasia. In the third child, CAKUT (ectopy) was an incidental finding on the ultrasound examination.
Prognosis of PSGN is usually benign with low mortality rate in the acute stage. The long-term prognosis in children is also excellent.Citation5–9 The prognosis of the disease may be not so favorable in patients with additional risk factors such as low birth weight, older age, hypertension, diabetes or preexisting kidney disease.Citation10–13
Analysis of the follow-up data in our series revealed that three children fully recovered. One child with bilateral hypodysplasia had progressive worsening of the renal function and has been prepared for renal replacement therapy. The second child with single kidney has stable renal function but has significantly increasing levels of proteinuria. It is of note that the proteinuria was not evident on the routine analysis 2 months before the attack of PSGN. This child has an additional risk factor—he was born small for gestational age.
There are only few reports on PSGN in children with CAKUT. Sheridan et al. described a 7-year-old boy with bilateral vesicoureteral reflux and reflux nephropathy who developed acute renal failure without evidence of either infection or obstruction.Citation14 The serology and renal biopsy established the diagnosis of PSGN. His renal function did not improve and he started chronic dialysis.
Fujinaga et al. reported a 9-year-old boy who presented with PSGN and acute renal failure (serum creatinine 4 mg/dL).Citation15 Ultrasonography revealed severe bilateral hydronephrosis. Voiding urethrocystography demonstrated bilateral vesicoureteral reflux grade V. Since significant proteinuria persisted renal biopsy was performed showing global sclerotic changes in 13 of 23 glomeruli, but crescent formations were not detected. Such severe disease course was due to marked chronic tubulointerstitial changes as a consequence of megaureter-megacystis syndrome and bilateral reflux nephropathy.
Naito-Yoshida et al. reported a case of severe PSGN superimposed on bilateral renal dysplasia.Citation16 Patient’s creatinine increased from the baseline level of 1.1–2.2 mg/dL, than after 1 month returned to the baseline value (1.2 mg/dL). Interestingly, over time the slope of creatinine clearance was steeper than before the episode of PSGN.
According to the Brenner theory individuals with low nephron number are prone to developing progressive renal damage later in life, when other risk factors become operative (infections, hypertension, diabetes, nephrotoxic drugs).Citation17 At the single-nephron level, hyperfiltration leads to intraglomerular hypertension with consequent proteinuria. If untreated, glomerular filtration rate progressively falls in these individuals in parallel with a further rise in proteinuria which may lead, in the long run, to end-stage renal failure. Glomerular hyperfiltration has been observed in patients with unilateral renal agenesis, congenitally reduced nephron number (bilateral hypoplasia/dysplasia) and acquired reduction in renal mass (bilateral reflux nephropathy).
In our report on five children with PSGN superimposed on CAKUT, the prognosis is worse than in children with PSGN without CAKUT. The children with single kidney, those with bilateral hypoplasia/dysplasia and with bilateral reflux nephropathy are expected to have lower nephron mass. Postreptococcal glomerulonephritis usually has benign course. The unfavorable course is seen in children with crescents, particularly in those if more than 50% of glomeruli are affected.Citation5,Citation10 Even without crescents some glomerular lesions in PSGN will heal with glomerulosclerosis that will additionally reduce the number of functional glomeruli. In children without CAKUT 20–30% of glomeruli affected by crescents will not significantly affect the outcome. Contrary, in children with CAKUT who already have lower nephron mass, this additional damage in 20–30% of glomeruli will have significant impact on the renal function and the long-term outcome due to exaggerated hyperfiltration.
The limitation of our study is the low number of patients and the lack of renal biopsy. The precise histologic evaluation will be valuable in predicting the outcome. Further studies and reports on larger number of patients where PSGN is superimposed on CAKUT are needed, particularly from countries, where PSGN is still common.
Conclusions
Poststreptococcal glomerulonephritis in children is generally benign disease with low mortality in acute stage and excellent medium and long-term prognosis. There are only few reports on the association of CAKUT with PSGN. We found that 2.6% of PSGN children had CAKUT. The worse outcome was noted in children with single kidney and bilateral renal impairment.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sanna-Cherchi S, Ravani P, Corbani V, et al. Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int. 2009;76:528–533
- Quirino IG, Dias CS, Vasconcelos MA, et al. A predictive model of chronic kidney disease in patients with congenital anomalies of the kidney and urinary tract. Pediatr Nephrol. 2014;29:2357–2364
- Wühl E, van Stralen KJ, Verrina E, et al. Timing and outcome of renal replacement therapy in patients with congenital malformations of the kidney and urinary tract. Clin J Am Soc Nephrol. 2013;8:67–74
- Neild GH. What do we know about chronic renal failure in young adults? II. Adult outcome of pediatric renal disease. Pediatr Nephrol. 2009;24:1921–1928
- Tasic V. Postinfectious glomerulonephritis. In: Geary DF, Schaefer F, eds. Comprehensive Pediatric Nephrology. St. Louis, MO: Mosby; 2008:309–317
- Clark G, White RH, Glasgow EF, et al. Poststreptococcal glomerulonephritis in children: Clinicopathological correlations and long-term prognosis. Pediatr Nephrol. 1988;2:381–388
- Popović-Rolović M, Kostić M, Antić-Peco A, Jovanović O, Popović D. Medium- and long-term prognosis of patients with acute poststreptococcal glomerulonephritis. Nephron. 1991;58:393–399
- Potter EV, Lipschultz SA, Abidh S, Poon-King T, Earle DP. Twelve to seventeen-year follow-up of patients with poststreptococcal acute glomerulonephritis in Trinidad. N Engl J Med. 1982;307:725–729
- García R, Rubio L, Rodríguez-Iturbe B. Long-term prognosis of epidemic poststreptococcal glomerulonephritis in Maracaibo: Follow-up studies 11–12 years after the acute episode. Clin Nephrol. 1981;15:291–298
- Kambham N. Postinfectious glomerulonephritis. Adv Anat Pathol. 2012;19:338–347
- Lee MN, Shaikh U, Butani L. Effect of overweight/obesity on recovery after post-infectious glomerulonephritis. Clin Nephrol. 2009;71:632–636
- Herrera J, Rodríguez-Iturbe B. End-stage renal disease and acute glomerulonephritis in Goajiro Indians. Kidney Int Suppl. 2003;83:S22–S26
- Hoy WE, Kincaid-Smith P, Hughson MD, et al. CKD in aboriginal Australians. Am J Kidney Dis. 2010;56:983–993
- Sheridan RJ, Roy S 3rd, Stapleton FB. Reflux nephropathy complicated by acute post-streptococcal glomerulonephritis. Int J Pediatr Nephrol. 1983;4:119–121
- Fujinaga S, Hirano D, Nishizaki N, et al. Unfavorable outcome in a child with megaureter-megacystis syndrome complicated by mild acute poststreptococcal glomerulonephritis. Pediatr Int. 2010;52:895–896
- Naito-Yoshida Y, Hida M, Maruyama Y, Hori N, Awazu M. Poststreptococcal acute glomerulonephritis superimposed on bilateral renal hypoplasia. Clin Nephrol. 2005;63:477–480
- Brenner BM, Lawler EV, Mackenzie HS. The hyperfiltration theory: A paradigm shift in nephrology. Kidney Int. 1996;49:1774–1777