Abstract
Background: The use of renal replacement therapy (RRT) modality in the intensive care unit (ICU) depends primarily on provider preference and hospital resource. This study aims to describe the prevalence of RRT use and the trends in RRT modality use in the ICU over the past 7 years. Methods: All ICU admissions, including medical, cardiac, and surgical ICUs from 1 January 2007 to 31 December 2013, were included in this study. RRT use was defined as the use of intermittent hemodialysis (IHD) or continuous renal replacement therapy (CRRT) within a given ICU day. The RRT use was reported as the proportion of ICU days on each RRT modality divided by the total ICU days with RRT usage. Results: Over the course of this study (72,005 ICU admissions), 272,271 ICU days were generated. RRTs were used in 4110 ICU admissions (5.7%) and on 21,159 ICU days (7.8%). RRT use was 10,402 (49%) for IHD, and 10,954 (52%) for CRRT. The trend of IHD and CRRT use did not change from year 2007 to 2013. On ICU days with RRT, the choice of RRT modality was associated with the number of vasopressor use (p < 0.001). CRRT was more preferred on the ICU days with the increasing number of vasopressor use. Conclusions: RRTs were used in about 6% of ICU admission. The use of IHD and CRRT was similar and did not change over 7 years. The choice of RRT modality mainly depended on the number of vasopressors used on ICU days with RRT.
Background
Acute kidney injury (AKI) is very common in critically ill patients, occurring in patients admitted to intensive care units (ICUs) ranges from 30% to 60%.Citation1–4 The management of patients with AKI is principally supportive, and renal replacement therapy (RRT) is indicated in patients with severe AKI.Citation5
In 1977, continuous renal replacement therapy (CRRT) was used for the treatment of multi-organ failures due to inadequacies of conventional intermittent hemodialysis (IHD).Citation6–8 For the past decades, many studies have demonstrated a number of physiological advantages of CRRT over conventional IHD, including hemodynamic stability, correction of hypervolemia, better solute removal.Citation9–11 However, the physiologic superiority has not been translated into clinically superiority. In 2007, a systematic review and meta-analysis of randomized controlled trials (RCTs) of 15 studies with 1550 patients showed that the RRT modality, IHD versus CRRT, did not affect important patient outcomes.Citation12 Kidney Disease: Improving Global Outcomes (KDIGO) has subsequently recommended no preference of modality of RRT, but emphasized the importance of adequacy of RRT, which were the delivering a dialysis efficiency (Kt/V) of 3.9 per week when using IHD and an effluent volume of 20–25 mL/kg/h for CRRT.Citation13 As a result, the choice of RRT modality use primarily depends on physician preference and hospital resource. However, the data on the prevalence and the temporal trend of RRT use for the management of severe AKI for the past decade have not been carefully established.
Thus, we conducted this study to describe the temporal changes in the utilization of RRT modality in the ICU setting over the course of 7 years.
Methods
Study population and setting
This is a descriptive study investigating the use of various RRT modalities in the ICU setting at a tertiary referral hospital system. All adult ICU admissions (age 18 years or older) from 1 January 2007 to 31 December 2013 were examined at two Mayo Clinic hospitals in Rochester, MN. Patients without authorization were excluded. The Mayo Clinic Institutional Board Review approved this study.
The Mayo Clinic Rochester hospital system consists of the Rochester Methodist (342 inpatient beds) and Saint Marys (946 inpatient beds) campuses. Because of the geographic distance between Mayo Clinic and the nearest non-Mayo Clinic ICU, critical care services around Rochester are provided exclusively to the local population by the Mayo Clinic Rochester hospital system. This system consists of a total of 167 beds (2012 and 2013) with varying types and adult ICU capacities (Supplemental available online at http://informahealthcare.com/doi/suppl/[doinumber]). Critical care specialists with internal medicine, anesthesiology, and/or surgery background manage and co-manage patients in all ICUs.
Table 1. Clinical characteristics.
Data collection
Clinical characteristics and the use of vasopressors were collected using automated retrieval from the institutional electronic medical record system. End-stage renal disease was identified based on the International Classification of Disease (ICD-9) code of 585.5, 585.6, 996.73, 996.68, 996.56, 792.5 and 458.21. The use of RRT within a given ICU day (12:00 am to 11:59 pm) during an ICU stay was reviewed. RRT use was defined as the use of IHD or CRRT including continuous veno-venous hemofiltration (CVVH), continuous venovenous hemodialysis, continuous venovenous hemodiafiltration, and slow continuous ultrafiltration, regardless of duration. The number of ICU days on any RRT and the number of ICU days on each RRT modality were collected. The use of each RRT modality was reported using the following formula:
To investigate the association between the choice of RRT modality and the number of vasopressors used, the use of vasopressor within ICU days with RRT was reviewed. Vasopressor was defined as the continuous intravenous administration of epinephrine, norepinephrine, phenylephrine, dopamine, or vasopressin, regardless of duration and dosage.
An electronic data extraction algorithm was developed to search for the use of dialyses and vasopressors within a given ICU day using data from a custom relational research database, which contains a near real-time copy of clinical data from the electronic medical record.Citation14 This database stores pertinent fluid input/output and Medication Administration Record data within an average of 15 min from entry into the medical record and serves as the data repository for data rules development.Citation14
To validate the accuracy of the electronic data extraction algorithm, 300 ICU patients were randomly select and comprehensive medical record review was performed for the use of RRT and vasopressors within a given ICU day. For RRT use, the algorithm has 100% sensitivity and 100% specificity (Table S2a available online at http://informahealthcare.com/doi/suppl/[doinumber]). For vasopressor use, the algorithm has 97% sensitivity and 100% specificity (Table S1b available online at http://informahealthcare.com/doi/suppl/[doinumber]).
Statistical analysis
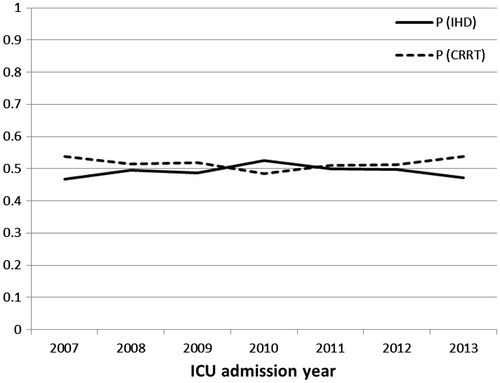
Continuous variables were reported as mean ± standard deviation (SD) for normally distributed data and median with interquartile range (IQR) for skewed data. Categorical variables were reported as counts and percentages. We calculated the proportion of ICU days on each RRT modality divided by the total ICU days with RRT usage: P (IHD), P (CRRT). The trend in the use of each RRT modality in each year from 2007 to 2013 was graphically represented and visually inspected. The association between the choice of RRT modality and the number of vasopressors used on ICU days with RRT was assessed using the chi-squared test. All analyses were performed using JMP statistical software (version 10, SAS, Cary, NC).
Results
From 2007 to 2013, there were 72,005 ICU admissions and 272,271 ICU days. The clinical characteristics, ICU and hospital outcomes are summarized in . The mean age was 63 ± 17 years. Fifty-eight percent were male and 6% had end-stage renal disease before ICU admission. The median SOFA score was 4 (IQR 2–7). The median ICU length of stay was 2 (IQR 2–4) days. Four percent and 7% died in ICU and hospital, respectively.
RRTs were used in 4110 of ICU admissions (5.7%) and on 21,159 ICU days (7.8%). The ICU and in-hospital mortality were 16% and 24%, respectively. The use of RRT ranged from 5.3% to 6.2% of ICU admission and 7.1% to 8.8% of ICU days over 7 years (). Out of 21,159 ICU days with RRT use, IHD was used for 10,402 (49%) and CRRT for 10,954 (52%). The trend of IHD and CRRT use did not substantially change from 2007 to 2013 ( and ). Among non-ESRD patients, out of 12,359 ICU days with RRT use, IHD was used for 4370 (35%) and CRRT for 8124 (66%). In contrast, among ESRD patient, out of 8800 ICU days with RRT use, IHD was used for 6032 (69%) and CRRT for 2830 (32%).
Table 2. Proportion of ICU with dialysis use divided by total ICU admission and proportion of total ICU day on dialysis over total ICU day.
Table 3. The proportion of specific dialysis modality use in ICUs from 2007 to 2013.
Of ICU days with RRT use, 51% were on vasopressor. The choice of RRT modality was significantly associated with the use and number of vasopressor use (p < 0.001 both). Of ICU days with RRT but without vasopressor use, IHD was used on 70% versus CRRT on 30%. In contrast, of ICU days with RRT and vasopressor use, IHD was used on 27% versus CRRT on 72% (). CRRT was increasingly preferred on the ICU days with the increasing number of vasopressor use ().
Table 4. The correlation between the choice of dialysis modality and vasopressor use on ICU days with dialysis.
Discussion
RRTs were used in about one-twentieth of ICU admission. The use of IHD and CRRT was comparable and did not change over 7 years of our study. Overall, the choice of RRT modality was correlated with the number of vasopressors used on ICU days with RRT, when CRRT was more preferred on the ICU days with the increasing number of vasopressor use.
Despite the releases of the systematic review and meta-analysis in 2007Citation12 and KDIGO clinical practice guideline for AKI in 2012 showing no superiority of clinical outcomes of CRRT over IHD, the trends in the use of RRT modality, IHD and CRRT, had not been changed between 2007 and 2013. This was likely due to the evidence of physiological benefits of CRRT.Citation9–11 Interestingly, even the meta-analysis revealed no differences in hemodynamic stability and hypotensive events between the two modalities, IHD and CRRT, intensivists and critical care nephrologists preferred CRRT to IHD correlated with higher vasopressor uses as demonstrated in our current study. This finding reflected that many clinicians had still believed in the CRRT’s physiological advantages when patients encountered severe AKI with hemodynamic instability requiring vasopressor agents despite the higher costs of providing CRRT than IHD.Citation15 In addition, for patients who are at risk of or who have increased intracranial pressure including neurosurgical patients, patients with encephalitis or acute liver failure, studies have demonstrated the benefits of prevention of the surge in intracranial pressure.Citation16–18
The future trend of the use of RRT modality in ICUs may change as a number of results of recent published studies favoring CRRT on the clinical outcomes. In 2014, Wald et al.Citation19 reported the findings of their retrospective cohort study conducted between July 1996 and December 2009. Compared with IHD, the investigators found that initiation of CRRT was associated with a 0.75-fold lower likelihood of chronic dialysis. Although there is currently no definite evidence from RCTs showing superiority of CRRT on clinical outcomes,Citation20,Citation21 this has been suggested likely because of the lack of sufficiently powered, multicenter RCTs.Citation6
This study has several limitations. First, this is a single-center, retrospective study in the USA. This limits the generalizability of some results, especially to other countries. For example, in the Australian ICU, the use of conventional IHD has been discouraged since 2001.Citation22 Second, we did not investigate the trend of each type of CRRT since CVVH has been used in our institution for the majority of cases with severe AKI (greater than 95%). Lastly, due to the descriptive nature of this study, the results are only reflective of the preference of RRT use; not appropriate use or patient outcomes. Thus, a multi-center, prospective study is ultimately required to address these limitations.
In summary, RRTs were used in about one-twentieth of ICU admission. The uses of the two modalities, IHD and CRRT, were similar and had not changed over 7 years. The choice of RRT modality mainly depended on the number of vasopressors used on ICU days with RRT, when CRRT was more preferred on the ICU days with the increasing number of vasopressor use.
Supplementary material available online
supplemental_document.pdf
Download PDF (18.2 KB)Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Notes
* Institution: This work was performed at Mayo Clinic in Rochester, MN.
References
- Susantitaphong P, Cruz DN, Cerda J, et al. World incidence of AKI: A meta-analysis. Clin J Am Soc Nephrol. 2013;8:1482–1493
- Thongprayoon C, Cheungpasitporn W, Akhoundi A, Ahmed AH, Kashani KB. Actual versus ideal body weight for acute kidney injury diagnosis and classification in critically ill patients. BMC Nephrol. 2014;15:176
- Srisawat N, Kellum JA. Acute kidney injury: Definition, epidemiology, and outcome. Curr Opin Crit Care. 2011;17:548–555
- Thongprayoon C, Cheungpasitporn W, Srivali N, Ungprasert P, Kittanamongkolchai W, Kashani K. The impact of fluid balance on diagnosis, staging and prediction of mortality in critically ill patients with acute kidney injury. J Nephrol. 2015. [Epub ahead of print]
- Murray P, Hall J. Renal replacement therapy for acute renal failure. Am J Respir Crit Care Med. 2000;162:777–781
- Ronco C, Bellomo R. Dialysis in intensive care unit patients with acute kidney injury: Continuous therapy is superior. Clin J Am Soc Nephrol 2007;2:597–600
- Kramer P, Wigger W, Rieger J, Matthaei D, Scheler F. [arteriovenous hemofiltration: A new and simple method for treatment of over-hydrated patients resistant to diuretics]. Klin Wochenschr. 1977;55:1121–1122
- Ronco C, Bellomo R. Continuous renal replacement therapy: Evolution in technology and current nomenclature. Kidney Int Suppl. 1998;66:S160–S164
- Bellomo R, Boyce N. Continuous venovenous hemodiafiltration compared with conventional dialysis in critically ill patients with acute renal failure. ASAIO J. 1993;39:M794–M797
- Manns M, Sigler MH, Teehan BP. Intradialytic renal hemodynamics – potential consequences for the management of the patient with acute renal failure. Nephrol Dial Transplant. 1997;12:870–872
- Vanholder R, Van Biesen W, Lameire N. What is the renal replacement method of first choice for intensive care patients? J Am Soc Nephrol. 2001;12(Suppl 17):S40–S43
- Rabindranath K, Adams J, Macleod AM, Muirhead N. Intermittent versus continuous renal replacement therapy for acute renal failure in adults. Cochrane Database Syst Rev. 2007:CD003773
- Section 5: Dialysis interventions for treatment of AKI. Kidney Int Suppl (2011). 2012;2:89–115
- Herasevich V, Pickering BW, Dong Y, Peters SG, Gajic O. Informatics infrastructure for syndrome surveillance, decision support, reporting, and modeling of critical illness. Mayo Clinic Proc Mayo Clinic. 2010;85:247–254
- Klarenbach S, Manns B, Pannu N, Clement FM, Wiebe N, Tonelli M. Economic evaluation of continuous renal replacement therapy in acute renal failure. Int J Technol Assess Health Care. 2009;25:331–338
- Davenport A, Will EJ, Davison AM. Effect of renal replacement therapy on patients with combined acute renal and fulminant hepatic failure. Kidney Int Suppl. 1993;41:S245–S251
- Davenport A, Finn R, Goldsmith HJ. Management of patients with renal failure complicated by cerebral oedema. Blood Purif. 1989;7:203–209
- Bellomo R, Ronco C. Continuous hemofiltration in the intensive care unit. Crit Care. 2000;4:339–345
- Wald R, Shariff SZ, Adhikari NK, et al. The association between renal replacement therapy modality and long-term outcomes among critically ill adults with acute kidney injury: A retrospective cohort study. Crit Care Med. 2014;42:868–877
- Uehlinger DE, Jakob SM, Ferrari P, et al. Comparison of continuous and intermittent renal replacement therapy for acute renal failure. Nephrol Dial Transplant. 2005;20:1630–1637
- Augustine JJ, Sandy D, Seifert TH, Paganini EP. A randomized controlled trial comparing intermittent with continuous dialysis in patients with arf. Am J Kidney Dis. 2004;44:1000–1007
- Silvester W, Bellomo R, Cole L. Epidemiology, management, and outcome of severe acute renal failure of critical illness in Australia. Crit Care Med. 2001;29:1910–1915