Abstract
Background: Acute kidney injury (AKI) is a serious complication in pregnancy, resulting in significant maternal morbidity/mortality and fetal loss. Although the incidence of pregnancy-related acute kidney injury (PRAKI) has decreased in developed countries, it is still common in developing nations. Methods: A prospective observational study was done between January 2010 and December 2014 to report the incidence, clinical spectrum, maternal and fetal outcome of AKI in pregnancy. Results: Total number of patients: 130; mean age: 25.4 ± 4.73 years. The incidence of AKI in pregnancy was 7.8%. Most of the AKI was noted in postpartum period (68%). Etiology of AKI was sepsis (39%), pre-eclampsia (21%), placental abruption (10%), acute diarrheal disease complicating pregnancy (10%), thrombotic microangiopathy (TMA) (9%), postpartum hemorrhage (2%) and glomerular diseases (9%). Renal biopsy (n = 46) done in these patients showed renal cortical necrosis (16), TMA (11), acute tubular injury (9), acute tubulointerstitial disease (1) and glomerular disease (9). Live births occurred in 42% of patients with vaginal delivery in 34% cases. Thirty-four patients were managed conservatively, while 96 required dialysis. Complete recovery occurred in 56% and about 36% had persistent renal failure at 3 months. Mortality rate observed was 8%. In univariate analysis, low mean platelet count, higher peak serum creatinine, dialysis dependency at presentation and histopathologically presence of cortical necrosis and TMA predicted the progression to chronic kidney disease. Conclusion: AKI in pregnancy was common in postpartum period and sepsis being the commonest cause.
Introduction
Pregnancy-related acute kidney injury (PRAKI) is still responsible for 15–20% of acute kidney injury (AKI) in developing countries.Citation1 Though there is decreased incidence of obstetric AKI due to improved antenatal care, PRAKI related to postpartum sepsis, pregnancy-induced hypertension and its complications still remain a therapeutic challenge. Obstetric renal failure has a bimodal occurrence in developing countries with first peak between 8 and 16 weeks of gestation in association with septic abortions, while late peak is associated with obstetric complications such as pre-eclampsia–eclampsia, abruption placentae, uterine hemorrhage, and puerperal sepsis.Citation2 AKI due to thrombotic microangiopathy (TMA) is increasingly reported recently.
Materials and methods
We conducted a prospective observational study at our tertiary care hospital over 5 years from January 2010 to December 2014. All consecutive patients with PRAKI referred to our institution were included and followed up for 3 months for the occurrence of chronic kidney disease (CKD). Patients with pre-existing renal disease were excluded from the study. A pre-designed proforma was used. Detailed clinical history regarding the number of pregnancies, outcome of previous pregnancies and presence of renal disease or hypertension was noted. Laboratory investigations included urine analysis, blood biochemistry and hemogram with peripheral smear. Sepsis screen including bacterial culture sensitivity on blood, urine or vaginal swabs, work up for disseminated intravascular coagulation, serum complements, anti-nuclear antigen and anti-neutrophilic cytoplasmic antibodies was done whenever required. The indications for renal biopsy were persistent renal failure for more than 3 weeks and features suggestive of underlying renal disease. Etiology of AKI, dialysis dependency, maternal outcome and fetal outcome was noted.
Definition
AKI: serum creatinine increased about 1.5 times from the baseline or when the urine output decreased to less than 400 mL for more than 6 h or both.
Oliguria: urine output less than 400 mL/24 hours.
Anuria: urine output less than 50 mL/24 hours.
Pre-eclampsia: Blood pressure: systolic ≥140 mmHg or diastolic ≥90 mmHg, after 20 weeks of gestation in a previously normotensive woman and proteinuria more than 300 mg in 24 h.
Eclampsia: generalized convulsions and/or loss of consciousness occurring during pregnancy or postpartum in pre-eclampsia.
HELLP syndrome: hemolysis (characteristic peripheral blood smear, serum lactate dehydrogenase ≥600 U/L, total serum bilirubin ≥1.2 mg/mL), elevated liver enzymes (serum aspartate aminotransferase ≥70 U/l), and low platelet count (<100,000/cu mm).
Complete recovery: serum creatinine less than 1.2 mg/dL.
Chronic kidney disease: serum creatinine of more than 1.5 mg/dL at 3 months.
Statistical analysis
All the variables were expressed as mean and median (range) wherever appropriate. Univariate analysis of variables that predict progression to CKD was done by Fisher’s exact and two-tailed Student’s t tests. Statistical analysis was done with SPSS software 16 (SPSS Inc., Chicago, IL) and p-value <0.05 was considered statistically significant.
Results
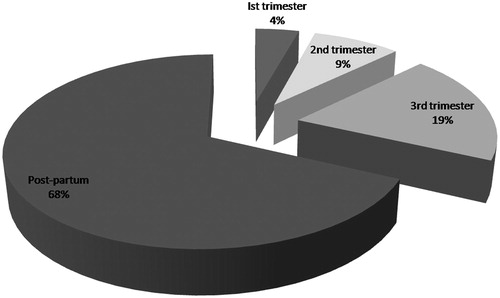
Total number of patients admitted with AKI during the study period was 1668, of which 130 (7.8%) were due to PRAKI. All our patients had institutional delivery. The age of patients ranged from 17 to 42 years with a mean age of 25.4 ± 4.73 years. About 90 patients were in the 20–30 years of age. Primigravida mothers slightly outnumbered multigravida (68 vs. 62) in our study. gives the time period of occurrence of PRAKI. The clinical profile and laboratory parameters of patients are shown in .
Table 1. Clinical profile of patients.
The most common cause of PRAKI in our study was sepsis, occurring in about 51 patients (39%). This included both septic abortion (n = 4) and puerperal sepsis (n = 47). Escherichia coli was the commonest organism isolated from urine, blood and high vaginal swab. About 21 patients had evidence of blood culture proven septicemia. Pre-eclampsia occurred in 21% (27 patients). The mean age of pregnancy at which pre-eclampsia was first detected was seventh month of pregnancy. About seven patients had generalized tonic clonic seizures and five patients had evidence of HELLP syndrome. Evidence of TMA with presence of fibrin thrombi in glomerular capillaries in histopathology was seen in 11 patients. Renal biopsy was done in 46 patients. Etiology and renal biopsy findings are summarized in . Two patients presented as rapidly progressive glomerulonephritis during pregnancy. Both had crescentic glomerulonephritis in biopsy, with lupus nephritis class IV in one and pauci-immune necrotising glomerulonephritis with p-ANCA (peri-nuclear anti-neutrophilic cytoplasmic antibodies) positive vasculitis in other.
Table 2. Etiology and renal biopsy findings.
About 96 (74%) patients required hemodialysis. Indications of hemodialysis include oligoanuria, metabolic acidosis, hyperkalemia, acute pulmonary edema and serum creatinine >3 mg/dL. Mean duration of dialysis dependency was 14 ± 2 days and mean number of dialysis sessions was 8 ± 1. Complete recovery occurred in 73 (56%) and about 46 (35%) had only partial recovery at 3 months of follow up. Only one patient who had septic abortion remained dialysis dependent with others being independent of dialysis at 3 months. The outcomes of patients are shown in . Death occurred in 10 (8%) patients, of which 8 had sepsis and 2 had pre-eclampsia/eclampsia.
Table 3. Maternal renal, fetal and obstetric outcomes.
In univariate analysis, low mean platelet count, higher peak serum creatinine, dialysis dependency at presentation and histopathologically presence of cortical necrosis and TMA predicted the progression to CKD (). Factors like age, total leucocyte count and presence of sepsis did not predict CKD progression.
Table 4. Risk factors for progression to CKD.
Discussion
AKI in pregnancy is a serious complication, involving the prognosis of the mother and the child. The incidence of PRAKI has decreased in developed countries to only 1–2.8%, while in developing countries it is around 4.2–15%.Citation3 The incidence in our study was 7.8%. Mean age of patients in this study was 25.4 ± 4.73 years, while most of the studies showed mean age of 26–30 years.Citation4 Primigravida was commonly affected (52%) in contrast to other studies, where multigravida constituted around 68–74%.Citation5
In this study, PRAKI was more frequent in the postpartum period (68%) similar to Sivakumar et al.Citation6 with 74.5% in postpartum, while most of the studies showed predominant incidence in the third trimester. Oliguria was present in 66%. Silva et al.Citation7 observed oliguria in 65% and significantly associated with HELLP syndrome, hyperbilirubinemia and death.
Studies showed the incidence of HELLP syndrome varying from 3% to 40%,Citation8 it was seen in 4% in this study. HELLP syndrome was described by Weinstein in 1982, as a serious complication of severe pre-eclampsia. Disseminated intravascular coagulation was seen in 22%. About 10–46% of pregnant women with AKI associated with HELLP syndrome need dialysis.Citation9 Maternal mortality is usually around 1% and perinatal mortality rate ranges between 7% and 34% depending on gestational age and maternal disease severity.Citation10
The causes of AKI in pregnancy are usually due to hyperemesis gravidarum, septic abortion in early pregnancy and pre-eclampsia, HELLP, TMA, acute fatty liver of pregnancy, antepartum hemorrhage, postpartum hemorrhage and sepsis in late pregnancy and postpartum period.Citation11 Sepsis (39%) was the commonest cause in this study, which includes postpartum sepsis in 36% and septic abortion in 3%. Septic abortion was the commonest cause in studies published in 1980–1990s, but its incidence decreased nowadays after legalization of abortion. Kumar et al.Citation12 reported puerperal sepsis in 29% of patients.
Pre-eclampsia related AKI was seen in 21% among which 4% presented with eclampsia. Pre-eclampsia affects approximately 3–5% of pregnancies. This is the commonest cause of AKI in developed countries. AKI occurs in approximately 1% of women with severe pre-eclampsia and 3–15% of women with HELLP syndrome.
Placental abruption and postpartum hemorrhage were seen in 10% and 2%, respectively. Postpartum and antepartum hemorrhage were responsible for PRAKI in 10.59% and 8.29% patients, respectively, in one study.Citation13 In contrast to this study, uterine hemorrhage was the dominant cause of PRAKI in the studies by Naqvi et al.Citation14 (58%). Ten percent were due to acute diarrheal disease, cause of AKI unrelated to pregnancy and miscellaneous causes in 6%.
Thrombotic microangiopathy was seen in 11% and glomerular diseases in 8%. TMA is characterized by thrombocytopenia, hemolysis and variable organ dysfunction, which can include neurological changes and AKI. Thrombotic thrombocytopenic purpura usually present prior to 24 weeks and hemolytic uremic syndrome occurs near term or postpartum. Increasing concentration of procoagulant (factor VIIa, factor VIII, von Willebrand factor, and fibrinogen) factors, decreased fibrinolytic activity, and deficiency of von Willebrand factor-cleaving protease (ADAMTS 13) may contribute to the development of TMA in pregnancy.Citation15 Pregnancy-associated TMA is rare, affecting 1 per 25,000 pregnancies. Seventy-six percent of patients with AKI related to TMA develop ESRD. Nine of 11 patients with TMA progressed to CKD in our study despite plasma exchanges.
Among glomerular disease, lupus nephritis was seen in five (IgA nephropathy, diffuse mesangial proliferation, focal segmental glomerulosclerosis, pauci-immune necrotising glomerulonephritis and infection related glomeruonephritis) each in one. Two patients had crescentic glomerulonephritis in biopsy, with lupus nephritis class IV in one and pauci-immune necrotising glomerulonephritis with antibody to myeloperoxidase (MPO) in other. Only few case reportsCitation16,Citation17 were available in the literature with lupus nephritis, granulomatous polyangiitis and microscopic polyangiitis presenting as rapidly proliferative glomerulonephritis during pregnancy.
Silva et al. showed etiologies of AKI as pregnancy-related hypertension (41.8%), HELLP syndrome (40%), puerperal sepsis (14.5%), abruption placentae (9.1%), hemolytic uremic syndrome (9.1%) and thrombotic thrombocytopenic purpura (5.5%).
In renal biopsy, cortical necrosis was the commonest histology (16) and acute tubular injury was seen in nine patients. The occurrence of cortical necrosis varied from 2% to 31% in previous studies. Obstetric causes account for 56–65.2% of cortical necrosis patients in two Indian studies.Citation18,Citation19
The requirement of hemodialysis was seen in 74% similar to Ansari et al.Citation20 Arora et al.Citation21 and Goplani et al.Citation22 reported a complete recovery of renal function in 42% and 61%, respectively, whereas, in this study, it was 56%. Thirty-five percent progressed to CKD and one patient who had septic abortion remained dialysis dependent. Maternal mortality rate was 8% as against reported incidence of 2–45% in the literature. Eighty percent of death were due to sepsis. Fetal loss occurred in 58% and cesarean section in 43%.
Prakash showed changing trends in pregnancy-related acute renal failure over 20 years, where the incidence dropped to 10% from 15%, pre-eclampsia–eclampsia to 14.4% from 23% and maternal mortality to 6.4% from 20%.Citation23 Factors that predicted progression to CKD in this study was thrombocytopenia, higher peak serum creatinine, dialysis dependency at presentation and histopathologically presence of cortical necrosis and TMA. One study showed age over 38 years and advanced stage of AKI according to RIFLE classification as poor prognostic factors. AKI in pregnancy is preventable and timely, aggressive management of obstetrical complications will reduce its incidence.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Aggarwal RS, Mishra VV, Jasani AF, Gumber M. Acute renal failure in pregnancy: Our experience. Saudi J Kidney Dis Transpl. 2014;25:450–455
- Sunil Kumar K, Ramakrishna C, Sivakumar V. Pregnancy related acute renal failure. J Obstet Gynecol India. 2006;56:308–310
- Chugh KS. Etiopathogenesis of acute renal failure in the tropics. Ann Natl Acad Med Sci (India). 1987;23:88–99
- Akhtar A, Zaffar S, Mehmood A, Nisar A. Obstetrical acute renal failure from frontier province: A 3 years prospective study. J Postgrad Med Inst. 2004;18:109–117
- Prakash J, Niwas SS, Parekh A, et al. Acute kidney injury in late pregnancy in developing countries. Ren Fail. 2010;32:309–313
- Sivakumar V, Sivaramakrishna G, Sainaresh VV, et al. Pregnancy-related acute renal failure: A ten-year experience. Saudi J Kidney Dis Transpl. 2011;22:352–353
- Silva JGB, Daher EF, Mota RM, Menezes FA. Risk factors for death among critically ill patients with acute renal failure. Sao Paulo Med J. 2006;124:257–263
- Sibai BM, Kustermann L, Velasco J. Current understanding of severe preeclampsia, pregnancy associated hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, hemolysis, elevated liver enzymes and low platelets and postpartum acute renal failure: Different clinical syndromes or just different names? Curr Opin Nephrol Hypertens. 1994;3:436–445
- Nisescrt S, Dribusch E, Bellmann O, Kauhausen H. Disorders of liver function, thrombopenia and hemodialysis in a special clinical form of hypertension in pregnancy (the so-called HELLP syndrome). Geburtshilfe Frauenheilkd. 1988;48:637–640
- Jayakumar M, Prabahar MR, Fernando EM, Manorajan R, Venkatraman R, Balaraman V. Epidemiologic trend changes in acute renal failure – A tertiary center experience from South India. Ren Fail. 2006;28:405–410
- Najar MS, Shah AR, Wani LA, et al. Pregnancy related acute kidney injury: A single center experience from the Kashmir Valley. Indian J Nephrol. 2008;18:159–161
- Kumar KS, Krishna CR, Kumar VS. Pregnancy related acute renal failure. J Obstet Gynaecol India. 2006;56:308–310
- Godara SM, Kute VB, Trivedi HL, et al. Clinical profile and outcome of acute kidney injury related to pregnancy in developing countries: A single-center study from India. Saudi J Kidney Dis Transpl. 2014;25:906–911
- Naqvi R, Akhtar F, Ahmed E, et al. Acute renal failure of obstetrical origin during 1994 at one centre. Ren Fail. 1996;18:681–683
- Machado S, Figueiredo N, Borges A, et al. Acute kidney injury in pregnancy: A clinical challenge. J Nephrol. 2012;25:19–30
- Milne KL, Stanley KP, Temple RC, Barker TH, Ross CN. Microscopic polyangiitis: First report of a case with onset during pregnancy. Nephrol Dial Transplant. 2004;19:234–237
- Talbot SF, Main DM, Levinson AI. Wegener’s granulomatosis: First report of a case with onset during pregnancy. Arthritis Rheum. 1984;27:109–112
- Pahwa N, Bharani R, Kumar R. Post-partum acute kidney injury. Saudi J Kidney Dis Transpl. 2014;25:1244–1247
- Prakash J, Tripathi K, Malhotra V, Kumar O, Srivastava PK. Acute renal failure in eastern India. Nephrol Dial Transplant. 1995;10:2009–2012
- Ansari MR, Laghari MS, Solangi KB. Acute renal failure in pregnancy: One year observational study at Liaquat University Hospital, Hyderabad. J Pak Med Assoc. 2008;58:61–64
- Arora N, Mahajan K, Jana N, Taraphder A. Pregnancy-related acute renal failure in eastern India. Int J Gynaecol Obstet. 2010;111:213–216
- Goplani KR, Shah PR, Gera DN, et al. Pregnancy related acute renal failure: A single center experience. Indian J Nephrol. 2008;18:17–21
- Prakash J. The kidney in pregnancy: A journey of three decade. Indian J Nephrol. 2012;22:159–167