Abstract
Aims and objectives: Renal involvement in patients of chronic liver disease (CLD) is one of the dreaded complications associated with a steep rise in mortality and morbidity. Derangements in various homeostatic mechanisms in CLD leading to direct renal injury or circulatory compromise have been associated with renal impairment. Method: Consecutive cirrhotic patients (n = 100) were included in the study. Structural and functional renal failure was identified and patients were classified into various renal syndromes pre renal, intra-renal and hepatorenal syndrome (HRS). Results: At the time of presentation, 37 patients had renal dysfunction. Thirty patients had pre-renal type of renal failure, six patients had intrinsic renal disease and one patient had structural renal disease. Patients with pre-renal type were further classified into volume responsive pre-renal failure and volume non responsive HRS. Five patients had features suggestive of HRS. Patients with decompensation such as portal hypertension (PHTN), jaundice, upper gastro-intestinal bleed and hepatic encephalopathy had significantly higher incidence of renal derangements as compared to their counterparts. Infection in the form of SBP and/or sepsis predisposed patients to develop renal dysfunction. Conclusion: Renal impairment in patients with advanced liver disease is not an uncommon phenomenon and is more commonly associated with a more advanced disease. Presence of PHTN and various signs of decompensation increase the chances of renal derangements in these patients. In view of rising incidence of CLD and higher survival (due to better treatment options available), one should be vigilant for the renal derangements in these patients.
Introduction
Renal involvement in patients of chronic liver disease (CLD) is one of the most dreaded complications associated with a steep rise in mortality and morbidity. A few conditions which accounts for the structural renal disease involving either glomerulus or the collecting system like glomerulonephritis, renal tubular acidosis, interstitial nephritis, etc. can be associated with liver involvement where basic pathology lies in kidney and is independent of hepatic involvement. Spectrum of functional renal disorder encompasses pre-renal azotemia accounting for most of the cases, ischemic acute tubular necrosis and hepatorenal syndrome (HRS). Functional renal failure (FRF) results from reduction of renal blood flow and glomerular filtration rate (GFR) of variable degrees that usually follows other abnormalities of renal function, such as sodium and solute-free water retention, manifested clinically by the development of ascites and dilutional hyponatremia.Citation1,Citation2 CLD itself is a state of imbalance between inflow and outflow of blood.Citation3 In advanced stages of CLD, when fibrosis ensues, obstruction to the flow of blood develops in portal and hepatic vasculature which is accounted for development of portal hypertension (PHTN) and ascites latter in the course.Citation4–6 This results in marked impairment of the systemic arterial circulation, characterized by arterial vasodilatation and compensatory activation of the endogenous vasoconstrictor systems. These activated vasoconstrictors cause an effect on the kidney circulation proportional to their degree of activation. Renal perfusion, which is already compromised in these patients due to loss of renal autoregulation and decreased cardiac output, is further negotiated. Any condition demanding for an increase in circulating systemic volume or a decrease in systemic pressure due to vasodilation (e.g., renal or gastrointestinal fluid losses, diarrhoea, or excessive administration of diuretics, infection) or loss of circulating volume (e.g., gastro-intestinal bleed) enhances the state of renal hypoperfusion.
Derangements in various homeostatic mechanisms marked by abnormal hepatic and other parameters due to CLD have been associated with renal impairment in these patients and studies on renal failure in CLD are scarce in our population. We assessed the incidence and causal relationship of various factors for different types of renal failure in cirrhotic patients in our study.
Materials and methods
The study included 100 adults patients with cirrhosis as evidenced by clinical examination substantiated by any of the following: serological or radiological evidence, and histo-pathology, if possible, who presented in Medicine OPD or were admitted to medicine wards of Pt. B.D. Sharma PGIMS, Rohtak after taking written informed consent.
Cirrhosis was considered of alcoholic etiology when daily ethanol consumption was >80 g/day in men and >60 g/day in women, with negative viral and immunological markers. Patients with age <18 and >75 years, acute liver cell failure and with history of use of some nephrotoxic drug within last 6 months were excluded. Patients with known renal disorder or transplanted kidney, any previous history of cognitive and mental dysfunction or any known psychiatric illness were excluded. The study protocol was duly approved by PG board of studies and ethical committee, University of health sciences, Rohtak (India).
A detailed history and clinical examination was undertaken in all subjects included in the study. History regarding any previous/concomitant illness intake of drugs; prescription as well as recreational history, was elicited and recorded if deemed relevant. Ascites was diagnosed by clinical features and confirmed by ultrasonography or diagnostic paracentesis. All patients underwent routine laboratory investigations including baseline evaluation which included complete blood counts, urine routine examination, coagulation profile, liver and renal function tests. Ascitic fluid analysis was done wherever present, for total proteins, total leukocytes with differential leukocyte count, SAAG, and culture.
Severity of CLD was assessed using MELD score as all patients were of advanced stages using formula:
MELD score was calculated for every patient and patients were distributed into five groups accordingly.
Group I consisted of 5 patients with MELD score <9.
Group II consisted of 40 patients with MELD score 10–19.
Group III consisted of 31 patients with MELD score 20–29.
Group IV consisted of 19 patients with MELD score 30–39.
Group V consisted of 5 patients with MELD score >40.
FRF was assessed using urinary output and serum creatinine (SCr). The renal failure indices (RFIs) were calculated for the patients with renal dysfunction in the form of fractional excretion of sodium (FeNa), RFI, urinary creatinine to serum creatinine ratio (UCr/SCr) and blood urea nitrogen to SCr ratio (BUN/SCr). Structural renal dysfunction was assessed with urine routine examination and 24 h proteinuria. Depending upon the renal parameters, RFIs and urinary examination, patients were classified into various renal syndromes pre-renal, intra-renal and HRS.Citation7,Citation8
Sepsis was defined as systemic inflammatory response syndrome that has a proven or suspected microbial etiology.Citation9 Spontaneous bacterial peritonitis (SBP) was diagnosed on the basis of an elevated ascitic fluid absolute PMN count (i.e., ≥250 cells/mm3) without an evident intra-abdominal source of infection that requires surgical treatment and ascitic fluid culture.Citation10
Statistical analysis
Continuous variables were expressed as mean ± standard deviation. Categorical variables were presented as numbers (percentage). At the end of the study, the data collected were analyzed by using ANOVA for the five different groups. Non-parametric test was used wherever data were skewed. Chi-square test was used to analyze the qualitative data and student’s independent t-test was used for analyzing the different parameters in subgroup analysis. Multivariate logistic regression analysis was done to assess the independent parameters associated with renal dysfunction.
Results
The mean age of patients was 46.12 ± 11.33 years, with a range of 20–70 years. Ninety-six patients were males with only four females. The major etiology was found to be alcohol (n = 88) and all the patients in this group were males. Other etiologies included cryptogenic (n = 5), hepatitis B (n = 4), hepatitis C (n = 2) and alcohol with hepatitis B (n = 1). The prevalence of alcoholic liver disease in this study was probably because most of the patients were males. Of all the patients, icterus was present in 59 patients; 60 patients had clinically evident ascites with almost half of the patients having fluid thrill whereas, UGI bleed was present in 41 patients and 26 patients had features of hepatic encephalopathy (HE).
Severity of CLD was assessed using MELD score. Mean MELD score was found to be 23.13 ± 10.26 with a minimum and maximum score of 6 and 59, respectively. MELD score was calculated for every patient and patients were distributed into five groups accordingly. shows the comparison in demographic, etiological profile and means arterial pressure (MAP) of the groups where no significant difference was found.
Table 1. Demographic and Etiological Profile of patients in various groups.
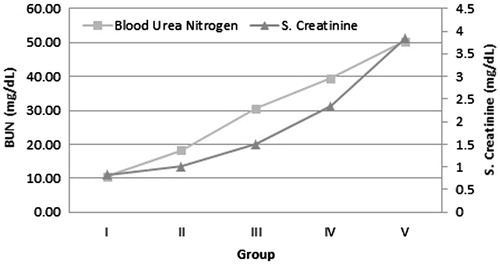
Various laboratory and radiological parameters were compared in the five groups and a significant difference was found in 12 variables including total albumin, serum bilirubin, prothrombin time, INR, blood urea, BUN, SCr, serum sodium, urine output, GFR, portal vein diameter (PVD) and spleen size as shown in .
Table 2. Comparison of various parameters in various groups.
At the time of presentation, 37 patients had renal dysfunction with RFIs indicating a pre-renal type of renal failure in 30 patients, whereas intrinsic renal disease in six patients and structural renal damage was found in only one patient. Patients with pre-renal type were further classified into volume responsive pre-renal failure and volume non responsive HRS. Five patients had features suggestive of HRS. The frequency of renal dysfunctions with advancing grades of MELD score also increased ().
Table 3. Distribution of renal dysfunction and its types in various groups.
Patients with PHTN as marked by PVD of ≥13 mm and/or ascites had higher incidence of renal dysfunction. Patients with other forms of decompensation such as jaundice, upper gastro-intestinal bleed and HE were prone to develop renal derangements as compared to their counterparts. Infection in the form of SBP and/or sepsis predisposed patients to develop renal dysfunction ().
Table 4. Complication of cirrhosis and renal dysfunction.
In a sub-group analysis in patients with or without renal dysfunction as depicted in , there was no significant difference in age and sex distribution. MELD score was significantly higher in patients with renal dysfunction. A total of 12 variables were evaluated in context of renal dysfunction. Significant statistical differences were obtained in most of the variables studied including total leukocyte count, serum protein, total albumin, serum bilirubin, prothrombin time, INR, serum sodium, and PVD.
Table 5. Various parameters in renal dysfunction.
In logistic regression analysis, MELD, PVD and INR were found to be three independent variables associated with development of renal dysfunction in patients with CLD ().
Table 6. Logistic regression analysis results.
Discussion
The prevalence of CLD has been increasing since last few years which can both be attributed to early diagnosis and an increased incidence.Citation11 One of the major concerns associated with CLD is its unrelenting course, as no therapies have been found to prevent its progression to advanced stages which are marked by fibrosis and cirrhosis as final outcome. Advancement of liver disease is generally associated with various consequences such as PHTN, upper GI bleed, ascites and SBP. Deranged liver physiology has a profound effect on the homeostatic mechanisms of the body affecting various other organs, including lungs and kidneys.
Importance of renal involvement in CLD has long been recognized by many workers.Citation12,Citation13 Renal dysfunction has been recently emphasized by Choi et al. in a retrospective study, where they concluded that renal derangement in CLD was not an uncommon phenomenon.Citation14 Renal failure in patients with CLD, particularly with advanced liver disease, seems to be common; however, the exact incidence is unknown and is probably underestimated. This may be explained by the fact that patients with cirrhosis tend to have falsely low SCr levels due to decreased hepatic creatinine synthesis and decreased skeletal muscle mass.Citation15 ARF in patients with cirrhosis frequently accompanies complications such as bacterial peritonitis, sepsis or hypovolemia from gastrointestinal bleeding, excessive diuretic therapy or administration of nephrotoxic drugs/contrast agents.Citation16 The probability of the occurrence of HRS in patients with cirrhosis and ascites at 1 and 5 years is 18% and 39%, respectively, with mortality approaching 100% in type 1 HRS without specific therapy. The median survival time in these patients without liver transplantation was only 12 days after diagnosis in one study.Citation17 However, this seems to have improved with terlipressin and albumin therapy. The development of ARF in patients with advanced liver disease has significant prognostic importance.Citation18 In patients with cirrhosis admitted to hospital with acute upper gastrointestinal hemorrhage, development of ARF forms an independent predictive factor for death.Citation19 There is considerable evidence that ARF in cirrhosis is primarily related to disturbances in circulatory function, mainly a reduction in systemic vascular resistance as a result of primary arterial vasodilatation in the splanchnic circulation, triggered by PHTN.Citation20 Furthermore, an intrinsic defect in cardiac performance termed cirrhotic cardiomyopathy lead to attenuated cardiac function, also contribute to renal dysfunction in cirrhotics particularly when exposed to stressful events like sepsis.Citation21 A very few studies have been undertaken in Indian context regarding the relationship between CLD and renal functions. In view of these facts, the study was planned to evaluate the renal function in 100 patients of CLD and the various factors affecting them.
The mean age of patients in the present study was 46 years which shows a declining trend in age of presentation of these patients and was in coherence with the recent studies. With male predominance, the major etiology for CLD was found to be alcohol which is also supported by the recent studies which show a rising trend in alcoholic liver disease.Citation22
Most of the patients presented in a decompensated state, ascites was evident in 61 patients with almost half of the patients having fluid thrill, whereas UGI bleed was present in 41 patients and 26 patients had features of HE. Anemia was prevalent amongst all the groups attributable to decreased production due to nutritional deficiencies, increased destruction due to splenomegaly and blood loss due to associated upper GI losses. In the present study, there was a decreasing trend in serum protein and total albumin and an increasing trend in the prothrombin time marking the decreased production of coagulation factors, amongst the five groups. A decreased production of albumin and coagulation factors pointed out advanced liver disease. An increasing trend in serum bilirubin was noticeable amongst the groups. PHTN is an essential feature of advanced CLD. PVD, splenomegaly and ascites are amongst the easily available parameters to assess PHTN in these patients. An increasing trend was noticeable in PVD, spleen size and prevalence of ascites. Renal parameters were found to follow an increasing trend, whereas GFR and urinary output followed a decreasing trend. Renal derangements were assessed using SCr, urinary output, proteinuria/hematuria and RFIs; a total 37 patients were found to have renal dysfunction. The higher incidence of renal dysfunction in this population can be explained due to lack of awareness amongst the patients and paucity of resources for management, late presentation in the course of the disease can be another cause as mostly patients presented in a decompensated state with massive ascites, jaundice, UGI bleed and HE for the first time.
It could be noted that all patients in group V had renal impairment whereas in group I, none of the patient exhibited any renal abnormality. Thus, the inference was that the patients with much advanced disease as indicated by higher MELD score have higher propensity to develop renal dysfunction. As severity of CLD increased as per MELD score, there was a statistically significant rise in SCr and blood urea nitrogen (). Another important finding was, when assessed for the type of renal dysfunction using RFIs, patients with HRS and ATN were found to be majorly distributed in group IV and V. Patients with HRS and ATN had higher MELD score. This was consistent with the previous data. Schepke et al. conducted a study where they found that patients with HRS had higher MELD score and shorter survival.Citation23 Pre-renal type of renal failure was the most common type of renal dysfunction present in the subgroup analysis, with total 67.57% developing pre-renal azotemia. Distribution of pre-renal azotemia was almost even in all the groups when compared. “True hypovolemia” in the presence of splanchnic pooling of blood, is usually the main cause of renal failure generally, induced by hemorrhage, gastrointestinal losses, renal fluid losses with use of diuretic and sepsis which are common to all the groups. Patients with advanced disease have higher tendency to develop such complications because of associated PHTN. Vascular compartment contraction decreases the renal blood flow leading to decreased creatinine clearance in the initial stages of renal impairment marked by volume responsive pre-renal azotemia but as the disease process continues there are higher chances of developing volume non-responsive renal failure in the form of HRS. An acute event of greater severity such as massive GI blood losses or sepsis may precipitate decreased renal blood flow, leading to HRS or ATN. Renal injury if further ensues, there is likelihood of development of ischemic intra-renal pathologies affecting the tubules leading to ischemic tubular necrosis.Citation24 All the three types of renal failure mentioned above constitute the FRF. Another type of renal involvement is the structural disease which involves liver and kidney concomitantly and is marked by proteinuria/hematuria or active urinary sediments. In the present study, only one patient was found to have significant proteinuria, due to hepatitis C related glomerular involvement.
PHTN is the most common complication of CLD. Development of PHTN indicates progression of disease process and a trigger for decompensation. PHTN is usually assessed by easily available parameter such as portal venous diameter (PVD), which in our study was assessed using ultrasonography. A PVD ≥13 mm correlates well with PHTN.Citation25 PHTN plays a pivotal role in development of renal impairment in CLD patients. Of 46 patients with PVD ≥13 mm, 26 developed renal dysfunction which was statistically significant.
Decompensation in any form was found to be associated with higher incidence of renal dysfunction. Ascites another consequence of PHTN and marker of decompensation was found in more than half of the patients in the study. Approximately 50% of the patients with ascites developed renal derangements, thus implying that the presence of ascites promotes renal derangement. In a large prospective multicentric study conducted by Montoliu et al. to assess the incidence of renal dysfunction in patients with cirrhosis and ascites, they found that approximately 50% of the cirrhotic patients with ascites developed some type of FRF during the follow-up period; renal failure was associated with worse prognosis.Citation26 Gines et al. conducted a large prospective study which included 234 non-azotemic patients of cirrhosis with ascites to assess the incidence of HRS in patients of cirrhosis with ascites and found that 18% developed type 1 HRS at 1 year and 39% at 5 years.Citation17 Ascites an outcome of splanchnic vasodilation, PHTN and activation of various sodium conserving mechanisms in the wake of reduced circulating volume leads to stimulation of renin angiotensin aldosterone system, sympathetic nervous system and arginine vasopressin which further compromises the renal blood flow in these patients.Citation27,Citation28
Fifty-four percent of patients with jaundice, another form of decompensation, developed renal derangements in one form or another. Watt et al. in their study found that jaundice more commonly preceded HRS.Citation29 More than half of the patients presenting with upper GI bleed had renal derangements at presentation which can be attributed to volume contraction of the systemic vascular compartment leading to a compromise in renal perfusion. Renal failure was more commonly found in patients with HE, which was earlier concluded by Watt and colleagues in their retrospective study, where they found that patients with renal dysfunction had higher incidence of HE.Citation29
Infections such as peritonitis, pneumonitis, urinary tract infection and gastro-enteritis were found to be another important precipitant of renal dysfunction in the study population. Sixteen percent of patients developed infection-related renal failure and our data were close to the data from a prospective study by Montoliu et al. on 263 cirrhotic patients with ascites, where they found that infection related renal failure affected 37 (14.1%) patients.Citation26 Bacterial infections account for one-third of the cases of acute renal failure in advanced liver disease and is due to the fact that the pro-inflammatory response in a host with cirrhosis is significantly enhanced.Citation30,Citation31 The myriads of inflammatory cytokines, such as tumour necrosis factor α and interleukin 6, released by the bacteria can induce various changes in the microcirculation of many organs including the kidneys, which include development of microthrombi, endothelial dysfunction and capillary leak resulting in hypoperfusion cellular injury of the involved organ.Citation32
One of the most dreaded form of infection, SBP was found in 12 (∼20%) patients, of which 10 developed renal dysfunction. The incidence of renal dysfunction was found to be higher in our study as compared to previous studies done by Follo et al. and Jung et al.Citation30,Citation33 Studies have demonstrated that bacterial translocation from the intestinal lumen to the mesenteric lymph nodes—may play an important role in impairing circulatory function in advanced liver disease, eliciting an inflammatory response and splanchnic vasodilation resulting in further pooling of blood in splanchnic compartment and reduced renal blood flow indirectly, thus leading to renal dysfunction.Citation34,Citation35
When various parameters were assessed in patient with and without renal dysfunction, TLC was higher in patients with renal dysfunction indicating infection related renal failure. Mean serum protein and total albumin were significantly lower in patients with renal dysfunction as compared to those without it. Decreased albumin is one of the key components for ascites formation and further renal compromise in these patients. Intravenous albumin has long been used for management of renal dysfunction especially, HRS. Sort et al. found that plasma volume expansion with intravenous albumin reduces the incidence of renal impairment in cirrhotic patients admitted with SBP. It also reduces in-hospital and 3-month mortality.Citation36 This signifies the importance of hypoalbuminemia and its impact on renal impairment in CLD patients. The mean PT, INR, and serum bilirubin were higher in patients with renal dysfunction. The patients having renal dysfunction had lower albumin and increased prothrombin time when compared with patients having normal renal functions, indicating indirectly that severity of renal failure will have a negative correlation with serum albumin and prothrombin levels. In a prospective study on renal failure in CLD patients, Wu et al. found that patients with ARF had higher mean bilirubin.Citation37 All the findings signified that renal dysfunction occurs commonly in patients with advanced liver disease.
In multivariate logistic regression analysis, the only independent predictor factors for development of renal dysfunction were MELD score, PVD and INR. MELD score marks the severity of liver disease, whereas PVD was an indirect marker of PHTN, an essential component for development of renal dysfunction whereas deranged INR marks coagulopathy, a marker of advanced liver disease.
Thus, renal impairment in patients with advanced liver disease was not an uncommon phenomenon and was more commonly associated with a more advanced disease. Presence of PHTN and various signs of decompensation increase the chances of renal derangements in patients with CLD. In view of rising incidence of CLD and increasing treatment options available, thus raising the life expectancy in these patients, it is essential to be vigilant about the renal parameters in patients with liver disease.Citation38
Renal dysfunction has a negative impact in the natural history of cirrhosis with ascites, efforts to prevent its appearance should be performed, especially in those patients with high risk of developing it. The prognosis of a patient with advanced liver disease developing FRF is poor which is in part related to the associated liver failure.Citation26 Compared to patients with advanced cirrhosis but without FRF, who have an 80% survival over 8 years, the 50% survival of these patients is reduced to 40 months and development of HRS further decreases the survival.Citation39 Earlier diagnosis and implementation of currently established beneficial therapies such as vasoconstrictors (norepinephrine, terlipressin, ornipressin, octreotide, midodrine) and volume expanders usually in the form of albumin and isotonic saline, or renal support with renal replacement therapy or ECAD with MARS, and TIPS may help to potentially reduce the severity of kidney injury and increasing survival outcomes. Liver transplantation is the ultimate treatment of choice.
Renal dysfunction is an important and devastating complication, when develops in patients of CLD and is associated with a very poor outcome. Data have been scarce regarding the renal impairment in CLD and factors precipitating it, in our scenario. Furthermore, long-term studies are required to assess the factors associated with renal dysfunction and various precipitants of renal impairment in these patients.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Ginès P, Fernández-Esparrach G, Arroyo V, Rodés J. Pathogenesis of ascites in cirrhosis. Semin Liver Dis. 1997;17(3):175–189
- Guevara M, Ortega R, Ginès P, Rodés J. Pathogenesis of renal vasoconstriction in cirrhosis. In: Ginès P, Arroyo V, Rodés J, Schrier R, eds. Ascites and Renal Dysfunction in Liver Disease [Internet]. Oxford: Blackwell Publishing Ltd.; 2005:327–340
- Wanless IR, Crawford J. Cirrhosis. In: Odze R, Goldblum J, eds. Surgical Pathology of the GI Tract, Liver, Biliary Tree, and Pancreas. Philadelphia, PA: WB Saunders; 2009:1115–1146
- Schrier RW, Niederberger M, Weigert A, Ginès P. Peripheral arterial vasodilatation: Determinant of functional spectrum of cirrhosis. Semin Liver Dis. 1994;14(1):14–22
- Unikowsky B, Wexler MJ, Levy M. Dogs with experimental cirrhosis of the liver but without intrahepatic hypertension do not retain sodium or form ascites. J Clin Invest. 1983;72(5):1594–1604
- Cárdenas A, Bataller R, Arroyo V. Mechanisms of ascites formation. Clin Liver Dis. 2000;4(2):447–465
- Lin J, Denker BM. Azotemia and urinary abnormalities. In: Longo DL, Kasper DL, Jameson JL, Fauci AS, Hauser SL, Loscalzo J, eds. Harrison’sTM Principles of Internal Medicine. 18th ed. New York: Mc Graw Hill; 2012:334–340
- Arroyo V, Ginès P, Gerbes AL, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Int Ascites Club Hepatol Baltim Md. 1996;23(1):164–176
- Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655
- Runyon BA, AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: An update. Hepatol Baltim Md. 2009;49(6):2087–2107
- Nobili V, Carter-Kent C, Feldstein AE. The role of lifestyle changes in the management of chronic liver disease. BMC Med. 2011;9(1):70
- Clinical Report on Hydro-Peritoneum, based on an analysis of… Am J Med Sci [Internet]. Available at: http://journals.lww.com/amjmedsci/Fulltext/1863/04000/Clinical_Report_on_Hydro_Peritoneum,_based_on_an.2.aspx. Accessed October 28, 2014
- Hecker R, Sherlock S. Electrolyte and circulatory changes in terminal liver failure. Lancet. 1956;271(6953):1121–1125
- Choi YJ, Kim JH, Koo JK, et al. Prevalence of renal dysfunction in patients with cirrhosis according to ADQI-IAC working party proposal. Clin Mol Hepatol. 2014;20(2):185–191
- Sherman DS, Fish DN, Teitelbaum I. Assessing renal function in cirrhotic patients: Problems and pitfalls. Am J Kidney Dis Off J Natl Kidney Found. 2003;41(2):269–278
- Eckardt KU. Renal failure in liver disease. Intensive Care Med. 1999;25(1):5–14
- Ginès A, Escorsell A, Ginès P, et al. Incidence, predictive factors, and prognosis of the hepatorenal syndrome in cirrhosis with ascites. Gastroenterology. 1993;105(1):229–236
- Betrosian AP, Agarwal B, Douzinas EE. Acute renal dysfunction in liver diseases. World J Gastroenterol. 2007;13(42):5552–5559
- Cárdenas A, Ginès P, Uriz J, et al. Renal failure after upper gastrointestinal bleeding in cirrhosis: Incidence, clinical course, predictive factors, and short-term prognosis. Hepatol Baltim Md. 2001;34(4 Pt 1):671–676
- Schrier RW, Arroyo V, Bernardi M, et al. Peripheral arterial vasodilation hypothesis: A proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatol Baltim Md. 1988;8(5):1151–1157
- Mandell M-S. Cardiac evaluation of liver transplant candidates. World J Gastroenterol. 2008;14(22):3445–3451
- Ray G. Trends of chronic liver disease in a tertiary care referral hospital in Eastern India. Indian J Public Health. 2014;58(3):186–194
- Schepke M, Appenrodt B, Heller J, Zielinski J, Sauerbruch T. Prognostic factors for patients with cirrhosis and kidney dysfunction in the era of MELD: Results of a prospective study. Liver Int Off J Int Assoc Study Liver. 2006;26(7):834–839
- Moreau R, Lebrec D. Review article: Hepatorenal syndrome – Definitions and diagnosis. Aliment Pharmacol Ther. 2004;20(3):24–28
- Mandal L, Mandal SK, Bandyopadhyay D, Datta S. Correlation of portal vein diameter and splenic size with gastro-oesophageal varices in cirrhosis of liver. J Indian Acad Clin Med. 2011;12(4):266–270
- Montoliu S, Ballesté B, Planas R, et al. Incidence and prognosis of different types of functional renal failure in cirrhotic patients with ascites. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2010;8(7):616–622
- Fisher EM, Brown DK. Hepatorenal syndrome: Beyond liver failure. AACN Adv Crit Care. 2010;21(2):165–186
- Cárdenas A, Arroyo V. Mechanisms of water and sodium retention in cirrhosis and the pathogenesis of ascites. Best Pract Res Clin Endocrinol Metab. 2003;17(4):607–622
- Watt K, Uhanova J, Minuk GY. Hepatorenal syndrome: Diagnostic accuracy, clinical features, and outcome in a tertiary care center. Am J Gastroenterol. 2002;97(8):2046–2050
- Follo A, Llovet JM, Navasa M, et al. Renal impairment after spontaneous bacterial peritonitis in cirrhosis: Incidence, clinical course, predictive factors and prognosis. Hepatol Baltim Md. 1994;20(6):1495–1501
- Fasolato S, Angeli P, Dallagnese L, et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223–229
- Gustot T, Durand F, Lebrec D, Vincent J-L, Moreau R. Severe sepsis in cirrhosis. Hepatol Baltim Md. 2009;50(6):2022–2033
- Jung ES, Lee JS, Kim MH, Kim NH, Kim KA, Moon YS. [Renal dysfunction after spontaneous bacterial peritonitis in cirrhosis: Incidence and risk factors]. Korean J Gastroenterol Taehan Sohwagi Hakhoe Chi. 2006;48(6):401–407
- Wiest R. Splanchnic and systemic vasodilation: The experimental models. J Clin Gastroenterol. 2007;41(3):S272–S287
- Wiest R, Das S, Cadelina G, Garcia-Tsao G, Milstien S, Groszmann RJ. Bacterial translocation in cirrhotic rats stimulates eNOS-derived NO production and impairs mesenteric vascular contractility. J Clin Invest. 1999;104(9):1223–1233
- Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341(6):403–409
- Wu C-C, Yeung L-K, Tsai W-S, et al. Incidence and factors predictive of acute renal failure in patients with advanced liver cirrhosis. Clin Nephrol. 2006;65(1):28–33
- Thomson SJ, Westlake S, Rahman TM, et al. Chronic liver disease – An increasing problem: A study of hospital admission and mortality rates in England, 1979–2005, with particular reference to alcoholic liver disease. Alcohol Alcohol Oxf Oxfs. 2008;43(4):416–422
- Alessandria C, Ozdogan O, Guevara M, et al. MELD score and clinical type predict prognosis in hepatorenal syndrome: Relevance to liver transplantation. Hepatol Baltim Md. 2005;41(6):1282–1289