A 72-year-old woman presented at our department complaining of blurry vision, redness, foreign body sensation, and intermittent epiphora in her left eye, with progressive onset of symptoms over the previous 2 weeks. The patient had a past ophthalmic history of uncomplicated cataract extraction in both eyes, while her medical history referred to a recently diagnosed metastatic breast cancer, 3 years after a modified radical mastectomy and adjunct radiotherapy. The patient also had a systemic history of diabetes mellitus, type-2, efficiently controlled with metformin tablets, and hypertension treated with Ca2+ channel blockers. For her metastatic disease, she was receiving weekly intravenous infusions of docetaxel (40 mg/m2), (Taxotere by Sanofi-Aventis), with 4 out of 12 scheduled sessions completed before the onset of eye symptoms. She also complained of repeated nosebleeds over the last week, a well-known docetaxel-related side effect.
Best-corrected visual acuity (BCVA) at presentation was measured: 20/20 OD and 20/30 OS. On ophthalmic examination, an erosive conjunctival lesion covered by a white cheesy material was detected on the palpebral conjunctiva of the lower eyelid. Despite the evident punctal stenosis, the lacrimal duct was found to be patent on syringing. A marked inflammatory reaction, extending from the palpebral onto the bulbar conjunctiva and limbus, was also noted. Moreover, on biomicroscopy, we identified a corneal opacity adjacent to the limbus, corresponding to an edematous area of dense stromal infiltration. The affected conjunctival and corneal area was intensively stained with fluoroscein and Bengal rose staining, a strong indicator of epithelial degeneration (). The anterior chamber was quiet and clear, while dilated fundus examination was normal.
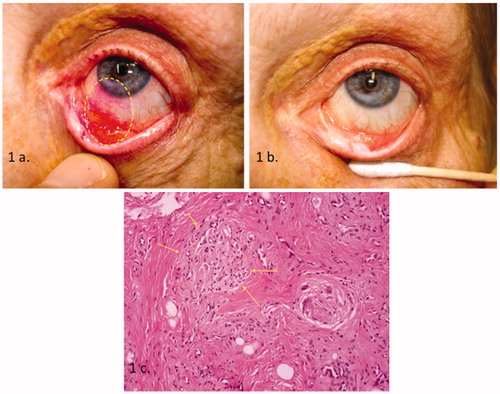
FIGURE 1. (a) Photograph of the affected eye shows an area of chronic inflammation with a high ratio of epithelial cell depletion. Corneal involvement is also shown as stromal infiltration (rose bengal staining-dotted ellipsoid). (b) The same eye photographed while patient was on topical steroids. A significant improvement of conjunctival injection is noted. However, a “cheesy” material overlying the erosive lesion as well as the corneal infiltration is still apparent. (c) Histologic examination of the lid biopsy shows chronic inflammation and fibrosis. Foreign body-type granulomas are also present (arrows) (×200 hematoxylin–eosin).
In regard to her systemic disease, the patient was considered fairly stable, apart from her blood count, which showed moderate neutropenia (ANC ∼1300/μL) and anemia (Ht: 30%, Hgb: 10.2 g/dL). We initially suspected herpes simplex virus (HSV) infection on the grounds of a chronic disease-related immunodeficiency and, therefore, prescribed topical and oral acyclovir (2 g/day) for a week, without any significant improvement. Conjunctival and corneal smears were negative for common pathogens and fungi in both rapid- and slow-growing cultivations. We also considered ocular tuberculosis as a possible causative factor. However, QuantiFERON-gold TB test and chest radiograph were proven nondiagnostic for the disease. In addition, polymerase chain reaction (PCR) also did not confirm HSV and Mycobacterium tuberculosis.
In the meantime, corneal edema extended centrally, affecting the patient's sight further. BCVA was measured: 20/20 OD and 20/40 OS. Topical steroids seemed to eliminate the inflammatory reaction and slightly alleviate symptoms () but flare-ups occurred immediately after tapering of medication. Interestingly, though, corneal neovascularization was never detected over the course of the inflammation.
We subsequently decided to obtain biopsies from the lower eyelid in order to rule out metastasis and primary malignancies. Histologic examination revealed nonspecific chronic inflammation with fibrosis and foreign body type granulomas (). A few weeks after discontinuation of chemotherapy, the inflammation subsided, while the patient developed peripheral corneal and palpebral scarring in the previously affected areas. Visual acuity improved, reaching 20/25 in the affected eye. The patient's condition remained completely unchanged on follow-ups at 3 and 6 months post-treatment, while ocular symptoms improved significantly.
Docetaxel is a new-age antineoplastic agent, widely used in the treatment of locally extensive or metastatic solid tumors. It belongs to a larger group of antineoplastic drugs, the so-called taxanes, which seem to interfere with the mitotic cycle of the neoplastic cells by promoting microtubulin assembly and inhibiting microtubule dynamics.Citation1 Breast cancer is among the commonest malignancies treated with this agent.Citation2 Weekly administration of docetaxel is associated with less systemic adverse effects, such as fatigue, nausea, myelosuppression, and neuritis, compared to the intermittent (every 21 days) infusions, but it is more frequently related to ocular adverse effects.Citation3
As Esmaeli and colleagues have extensively reported,Citation3–5 watery eyes represent the commonest problem the patients complain about as a result of a drug-related stenosis of the upper lacrimal duct. The drug seems to have cumulative effects since neither symptomatology nor remarkable findings are apparent before week 4 of administration. Fortunately, more than 50% of affected subjects experience a reversible stenosis without receiving any prevention treatment. Improvement of epiphora is frequently noted after cessation of chemotherapy. On the other hand, as Skolnick and Doughman reported,Citation6 erosive conjunctivitis was detected in a single case of a 58-year-old female while she was on weekly docetaxel and, interestingly enough, the condition subsided after forced discontinuation of chemotherapy for systemic reasons. However, and to extend of our knowledge, neither a corneal stromal infiltration nor any persistent fibrotic changes that may seriously affect the vision have ever been reported.Citation7 Nevertheless, similar clinical findings between our case and the one reported by Skolnick and Doughman are still notable. For example, the denuded, fluoroscein-stained conjunctival epithelium and conjunctival injection are present in both cases. Furthermore, the inflammation resolved shortly after discontinuation of chemotherapy.
In our case, although histopathology provides some evidence for the nature of the lesion, it cannot be diagnostic. Unfortunately, Skolnick's report did not include any histopathological study of the lesion and therefore such comparisons are not possible. However, chronic inflammatory reaction and fibrosis, both present in our case, have been suggested by Esmaeli et al. as main causative factors of canalicular stenosis in a series of patients treated with docetaxel.Citation5 The additional presence of foreign body type granulomas in our specimen may be related to intravenous drug administration or to still unknown infectious agents. Epithelial cells are reportedly more sensitive to cytotoxic effects due to their fast turnover, a fact that may explain the mucositis frequently seen in this group of patients.Citation8 The hypothesis that similar mechanisms may similarly affect conjunctival and/or corneal epithelia needs to be clarified.
Although the clear association between administration of docetaxel and keratoconjunctivitis seen in our case is difficult to prove, there is still some clinical and laboratory-derived evidence, enough to increase awareness about this presumed adverse effect. Furthermore, the likelihood of encountering metastases in this group of patients raises serious diagnostic dilemmas between clinicians when longstanding palpebral or conjunctival lesions masquerade as such.
Docetaxel, a widely used antineoplastic drug, has been thoroughly studied in regard to its systemic adverse effects. It is considered very efficacious in controlling certain metastatic malignancies, such as breast cancer. Nowadays, weekly intravenous administration is more preferable because of less severe systemic effects, but it is frequently related to cumulative ocular side effects, such as upper lacrimal duct stenosis. Corneal and conjunctival inflammatory changes could represent a completely new aspect in this sensitive group of patients that may imply involvement of a more complex, drug-related, ocular immune response awaiting further investigation.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Herbst R, Khuri F. Mode of action of docetaxel—a basis for combination with novel anticancer agents. Cancer Treat Rev. 2003;29:407–415
- Martin M, Pienkowski T, Mackey J, et al. Adjuvant docetaxel for node-positive breast cancer. N Engl J Med. 2005;352:2302–2313
- Esmaeli B, Hortobagyi G, Esteva F, et al. Canalicular stenosis secondary to weekly versus every-3-weeks docetaxel in patients with metastatic breast cancer. Ophthalmology. 2002;109:1188–1191
- Esmaeli B, Hidaji L, Adinin RB, et al. Blockage of the lacrimal drainage apparatus as a side effect of docetaxel therapy. Cancer. 2003;98:504–507
- Esmaeli B, Burnstine M, Ahmadi A, et al. Docetaxel-induced histologic changes in the lacrimal sac and the nasal mucosa. Oph Plast Reconst Surg. 2003;19:4305–4308
- Skolnick CA, Doughman DJ. Erosive conjunctivitis and punctal stenosis secondary to docetaxel (taxotere). Eye Contact Lens. 2003;29:134–135
- Schmid K, Kornek G, Scheithauer W, et al. Update on ocular complications of systemic cancer chemotherapy. Surv Ophthalmol. 2006;51:19–40
- Valero V, Holmes F, Walters R, et al. Phase II study of docetaxel: a new, highly effective antineoplastic agent in the management of patients with anthracycline-resistant metastatic cancer. J Clin Oncol. 1995;13:2886–2894

