Abstract
Purpose: To present a case of a full-thickness macular hole closure in a patient with Behcet uveitis
Design: A 23-year-old-male patient with Behcet Disease had clinically inactive uveitis with topical steroids, oral azathiopurine and cyclosporine until he developed a retinal infiltrate in the left eye which evolved into a full-thickness macular hole during the follow-up.
Methods: Strict control of inflammation and subsequent vitrectomy was planned. Meanwhile another attack of panuveitis developed in the left eye and subcutaneous Interferon alfa-2b interferon treatment was initiated.
Results: After 2 months, the patient was clinically inactive with complete closure of the macular hole.
Conclusions: Strict control of inflammation may result in closure of the macular hole and avoid the need for vitrectomy.
Behçet disease (BD) is a chronic inflammatory multisystem disorder of unknown cause. The disease is mainly characterized by ocular, oral, cutaneous, genital, vascular, and neurological manifestations.Citation1 Ocular pathologies, mostly bilateral panuveitis, are present in 60–80% of BD patients and are major causes of morbidity that may finally lead to blindness.Citation2 Among various associated ocular pathologies, development of a macular hole (MH) was reported in 2.6% and 3.4% of patients with BD in two large-scale studies.Citation3,Citation4 MH in BD may ultimately require vitreoretinal surgery, but a recently published study concluded that surgical intervention does not seem to have a potential beneficial effect on visual function.Citation5 This case report presents closure of a full-thickness MH, with strict control of inflammation, in a patient with Behçet uveitis.
A 23-year-old male patient with a 2-week history of blurred vision in the right eye was referred to our clinic. His medical history revealed recurrent oral aphthous ulcers for 1 year and a genital ulcer, which was present 2 months ago. On initial examination bilateral best-corrected visual acuity was 10/10. Slit-lamp biomicroscopic examination of the right eye revealed 2+ cells in the anterior chamber and 3+ in the vitreus. The left eye had trace amount of cells in the anterior chamber and vitreus. Fundus examination was unremarkable in the right eye, but small intraretinal hemorrhages with adjacent exudation in the nasal quadrant were observed in the left eye. Fundus fluorescein angiography showed diffuse dye leakage, signs of periphlebitis and cystoid macular edema in the left eye. Behçet disease was diagnosed based on the International Study Group for Behçet's Disease criteria.Citation1
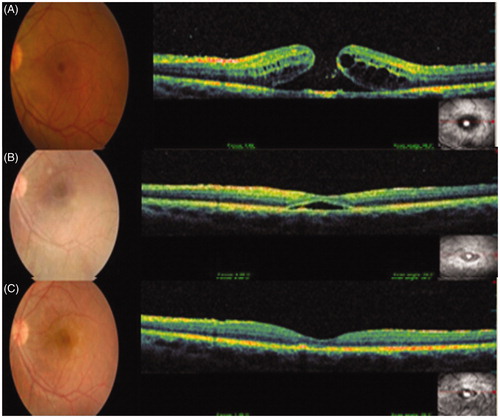
Both eyes were prescribed hourly topical corticosteroids and cycloplegics TID in addition to oral azathiopurine (Imuran; Glaxo SmithKline, 2.5 mg/kg/day). The topical treatment was tapered gradually. During the follow-up, a retinal infiltrate developed in the right eye, which prompted the addition of oral cyclosporine A (Sandimmun Neoral; Novartis Pharma, 5 mg/kg/day) and oral corticosteroids (Deltracortril; Pfizer, 1 mg/kg/day, tapered gradually) to the ongoing treatment. Three months after the first ocular manifestation, a panuveitis attack was observed in the left eye. The dosage of oral corticosteroids was increased to 1.5 mg/kg/day and the inflammation was brought under control. In the follow-up, visual acuity in the left eye decreased to 2/10 due to the development of a full-thickness macular hole (). Strict control of inflammation and subsequent vitrectomy were advised by the vitreoretinal surgeon. While the patient was waiting for vitrectomy, another panuveitis attack developed in the left eye. Due to the inadequacy of the ongoing treatment, subcutaneous interferon alfa-2b treatment at a daily dosage of 5 × 106 units (Intron A; Schering Plough) was initiated and tapered accordingly (5 × 106 2×/week after 1 month).Citation6 The patient was clinically inactive with complete closure of the macular hole after 2 months. Best-corrected visual acuity increased to 7/10 in the left eye ().
Figure 1. Color fundus photograph and spectral domain–optical coherence tomography (OPKO/OTI Spectral OCT/SLO, OPKO Health, Inc. Miami, Florida) images of the left eye show (A) a full-thickness macular hole before, (B) macular hole closure with subretinal fluid accumulation 1 month after, and (C) complete macular hole closure 4 months after the initiation of interferon alfa-2a therapy.
Antero-posterior traction, tangential traction, and degeneration of the inner retinal layers have been suggested as possible mechanisms of idiopathic macular holes.Citation7 The same principles can be applied for macular holes observed as a complication of posterior pole involvement in uveitis disease. Recurrent inflammation associated with edema and cystoid degeneration of the macula is suggested to contribute to macular hole development by causing disruption of retinal layers. Changes on the vitreoretinal interface, abnormal vitreoretinal tractions, and development of an epiretinal membrane secondary to inflammation are also thought to contribute to macular hole development by causing antero-posterior and tangential traction.Citation8
Several hypothetic mechanisms have been proposed as explanations to spontaneous closure of a macular hole. These include spontaneous release of vitreous traction, shrinkage of a developed epiretinal membrane, glial cell or RPE cell proliferation, and bridging of retinal tissue over the macular hole.Citation9 Although inconclusive, the following mechanisms can be adapted to this case as possible explanations to the macular hole closure: induction of glial or RPE cell proliferation at the base of the hole secondary to the severe inflammation in the last attack might have caused an approximation of hole borders; control of inflammation might have resulted in the resolution of cystoid macular edema and release of vitreous traction with subsequent flattening of the macula. Overall, strict control of inflammation in Behçet uveitis patients might promote the closure of the hole and avoid the need for vitrectomy.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet. 1990:335:1078–1080
- Mochizuki M, Akduman L, Nussenblatt RB. Behcet's disease. In: Pepose JS, Holland GN, Wilhelmus KR, eds. Ocular Infection and Immunity. St Louis: Mosby; 1996:663–675
- Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, et al. Uveitis in Behçet disease: an analysis of 880 patients. Am J Ophthalmol. 2004;138:373–380
- Benchekroun O, Lahbil D, Lamari H, et al. [Macular damage in Behçet's disease]. J Fr Ophtalmol. 2004;27:154–159
- Al-Dhibi H, Abouammoh M, Al-Harthi E, et al. Macular hole in Behçet's disease. Indian J Ophthalmol. 2011;59:359–362
- Zouboulis CC, Orfanos CE. Treatment of Adamantiades-Behçet disease with systemic interferon alfa. Arch Dermatol. 1998;134:1010–1016
- Smiddy WE, Flynn HW Jr. Pathogenesis of macular holes and therapeutic implications. Am J Ophthalmol. 2004;137:525–537
- Kahloun R, Ben Yahia S, Mbarek S, et al. Macular involvement in patients with Behçet's uveitis. J Ophthalmic Inflamm Infect. 2012;2:121–124
- Inoue M, Arakawa A, Yamane S, et al. Long-term outcome of macular microstructure assessed by optical coherence tomography in eyes with spontaneous resolution of macular hole. Am J Ophthalmol. 2012;153:687–691

