Abstract
Subacute sclerosing panencephalitis is a rare disease of central nervous system caused by defective measles virus. Chorioretinitis with macular involvement is the mostly observed ocular finding in the disease. Other reported ocular findings in the disease are cortical blindness, hemianopsia, nystagmus, extraocular muscle paresis and optic atrophy. We present a rare case of subacute sclerosing panencephalitis with isolated bilateral optic neuritis as the only ocular finding without macular involvement.
Subacute sclerosing panencephalitis (SSPE) is a chronic progressive viral infection of the central nervous system, with degenerative changes caused by the rubeola virus. The age at presentation in the literature is given as 8–11 years, with onset usually occurring 6 years after measles infection after a 6- to 8-year incubancy period.Citation1
Clinical findings and course of the disease vary in each case but initial symptoms commonly are decrease in school performance, progressive mental detoriation, myoclonic jerks, focal and generalized seizures, ataxia, and visual disturbances mostly due to chorioretinitis.Citation2,Citation3 The disease is fatal, usually resulting in death in 1–3 years.Citation1,Citation3 Higher remission rates are reported in adults with SSPE, but among those who progress, survival is shorter, with 5% dying within 3 months and only 20% alive more than 4 years after diagnosis.Citation1
Although it is not a part of the diagnostic criteria, ocular involvement is common in SSPE. Cortical blindness, hemianopsia, nystagmus, extraocular muscle paresis, papilledema, optic atrophy, macular chorioretinitis, and pigment alterations are reported in the literature.Citation4–6 They generally appear concomitant with neurological signs but may occationally preceed neurological findings. Chorioretinitis is reported as the most frequent ocular finding in the disease.Citation4–6 Here we report a case of SSPE without any of the other reported ocular findings of the disease other than bilateral optic neuritis and with no observation of chorioretinal involvement during the follow-up despite neurologic detoriation.
The authors adhered to the Declaration of Helsinki and all state laws in our country, and parents of the patient were asked to give consent before she was enrolled in the study.
We present an 11-year-old girl with seizures and myoclonic jerks for 3 months who had received a diagnosis of SSPE in a pediatric neurology clinic. She was admitted to our hospital due to a gradual loss of vision in her eyes for 3 days. The family didn't notice whether her peripheral vision was intact or not. No further information was detected about her color vision or night vision. She was hospitalized for further investigation. She was using carbamazepin 2 × 400 mg po and isoprinosine 3 × 1 po treatment on admission, which was started by her pediatric neurologist.
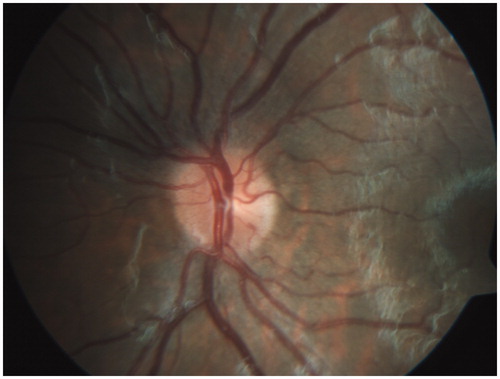
She had a history of generalized skin eruption at 3 years of age but the cause was not known by the family. She was co-operative but seemed depressive in behavior and had difficulty in understanding straightforward requests. She was unable to perform simple calculations. Neurological examination was normal for upper and lower extremity muscle tones, deep tendon reflexes were normoactive, and extrapyramidal system examination and cereballar tests were normal. Pupils were both dilated and unreactive to light. Visual acuity was estimated as at the level of perceiving hand motion bilaterally. Color vision was abnormal in both eyes, which was tested by Ishihara pseudoisochromatic plates. The anterior segment was normal in both eyes. On funduscopy the discs bilaterally appeared edematous (, ) and VEP p100 latencies were found to be prolonged on both sides. No macular or chorioretinal findings were observed on fundus examination during hospitalization.
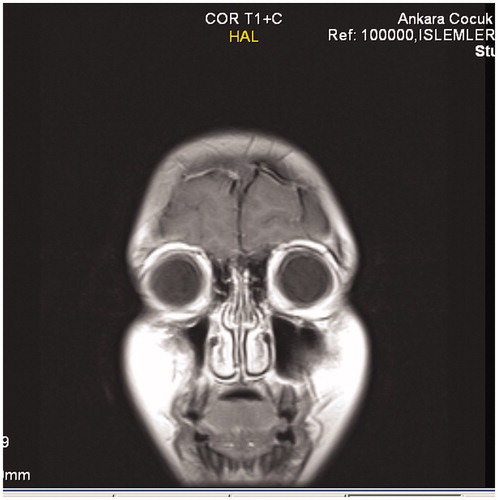
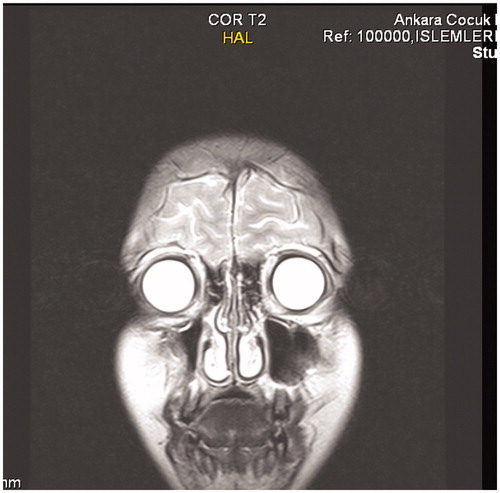
Routine blood tests, including hemogram and sedimentation rate, were normal. EEG findings of the patient were compatible with SSPE as periodical high-amplitude sharp and slow waves not suppressed by intravenous diazepam; cranial MRI revealed subcortical and cortical edema in 3 cerebral foci in left occipital lobe, right parietal lobe, and frontal lobe (, ). The opening CSF pressure in her LP was calculated as 140 mmH2O, which is important for excluding the the diagnosis of idiopathic intracranial hypertension. Rubeola IgG antibody titers in CSF were determined as 1.99 (>1.1 RU/mL by ELISA). EEG findings and high CSF rubeola IgG level confirmed the present diagnosis of SSPE, and IVIG treatment 0.4 g/kg/day for 5 days was started immediately. The patient's systemic and ocular status remained unchanged during 7 days of hospitalization. Supportive care was carried out by our neurology department. The patient showed no improvement in her general condition and was finally taken by her parents to be nursed at home. Her condition deteriorated so that 2 months after her first visit she was unable to walk or feed herself and had bilateral myoclonic jerks.
After 1 year of follow-up, there was no macular or chorioretinal involvement observed on fundus examination. Bilateral papillitis was still present in the last visit with the same visual acuity of perception of hand motion in both eyes. Neurological status continued to worsen.
Since eyes are developed from the optic vesicule of prosencephalone in the embryonic period, SSPE-like diffuse central nervous system diseases may affect ocular neuroectodermal structures.Citation7 Ocular involvement in SSPE is seen in 50% cases and chorioretinitis is reported as the most frequent finding.Citation5,Citation8 Cortical blindness, hemianopsia, nystagmus, extraocular muscle paresis, papilledema, optic atrophy, macular chorioretinitis, and pigment alterations are also reported and generally are observed before the neurological signs appear.Citation4 Disc edema had been reported in 20% of SSPE patients studied.Citation4 Ophthalmic manifestations of SSPE have previously been reported in small series or in case reports.Citation9–15 A case with bilateral optic nerve involvement was reported by Tandon et al.,Citation11 which was a young girl who initially presented with bilateral papillitis and subsequently developed macular retinitis. Nelson et al. presented autopsy results of two teenage girls who died due to SSPE, and reported postmortem demonstration of the retinal lesions even in one of the cases without any visual complaints during the illness and no retinal lesions demonstrated during life, except for some pallor of the optic discs.Citation9 It has been suggested that there is possibly measles virus-acquired virulent neurotropism in the retina before involvement of the central nervous system.Citation16
Our patient had a visual disturbance that started after her seizures had begun, which is not the typical time course reported in the literature. Another different aspect of our case is that SSPE cases may present with isolated optic nerve involvement as bilateral optic neuritis without any chorioretinal or macular changes. Of course, subcortical and cortical edema demonstrated in our patient's MRI may be another factor in her visual disturbance. It should also be remembered that cortical blindness, which is reported occasionally, may also contribute to the visual loss in these patients.Citation4 But the point we want to emphasize in this case report is the optic nerve involvement without any chorioretinal changes, which is quite different than most of the case reports in the literature.
The findings of macular pigmentary changes with “hole” formation and focal areas of chorioretinitis should alert the clinician to the possibility of SSPE.Citation10 But children with visual and neurologic disturbances that are associated either with isolated optic nerve edema or as part of a combined picture of optic nerve edema and macular pigmentary changes (especially chorioretinitis) should be investigated for the diagnosis of SSPE by EEG and CSF examination of rubeola IgG levels.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Gutierrez J, Issacson RS, Koppel BS. Subacute sclerosing panencephalitis: an update. Dev Med Child Neurol. 2010;52:901–907
- Solbrii MV. Viral infections of the nervous system. In: Bradley WG, Daroff RB, Fenichel GM, Marsden CD, eds. Neurology in Clinical Practise. Newton MA: Butterworth Heinemann; 2000:1366–1376
- Robertson WC Jr, Clorc DB, Markesberry WR. Review of 38 cases of subacute sclerosing panencephalitis: effect of amantadine on the natural course of the disease. Ann Neurol. 1998;8:422
- Green SH, Wirtschafter JD. Ophthalmoscopic findings in subacute sclerosing panencephalitis. Br J Ophthalmol. 1973;57:780–787
- Thorpe CG, Kocen RS. Subacute sclerosing panencephalitis presenting as transient homonymous hemianopia. J Neurol Neurosurg Psychiatry. 1983;46:186–187
- Landers MB, Klintworth GK. Subacute sclerosing panencephalitis (SSPE). Arch Ophthalmol. 1971;86:l56–l63
- Onder F, Or M, Gucuyener K, et al. A case of subacute sclerosing panencephalitis with chorioretinitis as the early manifestation. Retina-Vitreus. 1995;3:200–205
- Zagami AS, Lethlean AK. Chorioretinitis as a possible very early manifestation of subacute sclerosing panencephalitis. Aust N Z J Med. 1991;21:350–352
- Nelson DA, Weiner A, Yanoff M, DePeralta J. Retinal lesions in subacute sclerosing panencephalitis. Arch Ophthalmol. 1970;84:613–621
- Johnston HM, Wise GA, Henry JG. Visual deterioration as presentation of subacute sclerosing panencephalitis. Arch Dis Child. 1980;55:899–901
- Tandon, R Khanna S, Sharma MC, et al. Subacute sclerosing panencephalitis presenting as optic neuritis. Indian J Ophthalmol. 1999;47:250–252
- Hiatt RL, Grizzard HT, McNeer P, et al. Ophtalmologic manifestations of subacute sclerosing panencephalitis (Dawson's encephalitis). Trans Am Acad Ophthalmol Otolaryngol. 1971;75:344–350
- Serdaroğlu A, Gücüyener K, Dursun I, et al. Macular retinitis as a first sign of subacute sclerosing panencephalitis: the importance of early diagnosis. Ocul Immunol Inflamm. 2005;13:405–410
- Yuksel D, Sonmez PA, Yilmaz D, et al. Ocular findings in subacute sclerosing panencephalitis. Ocul Immunol Inflamm. 2011;19:135–138
- Colpak AI, Erdener SE, Ozgen B, et al. Neuroophthalmology of subacute sclerosing panencephalitis: two cases and a review of the literature. Curr Opin Ophthalmol. 2012;23:466–471
- Garg RK. Subacute sclerosing panencephalitis. J Neurol. 2008;255:1861–1871