Dear Editor,
We report the case of an 82-year-old male with vitreoretinal lymphoma and B-cell central nervous system (CNS) lymphoma who developed multiple discrete subretinal pigment epithelial (sub-RPE) deposits several months prior to tissue diagnosis. His past medical history was remarkable for hypertension, hypercholesterolemia, chronic obstructive pulmonary disease (COPD), hearing loss, and a remote ocular history of laser trabeculoplasty and mild nuclear sclerosis. He presented to our institution with a 6-month history of blurry vision in both eyes.
On initial examination, his visual acuity was 20/30 in the right eye and 20/40 in the left eye with 2+ nuclear sclerosis and 2+ vitritis OU. Optical coherence tomography (OCT) was unremarkable (). Prior to initiation of any therapy, he underwent diagnostic pars plana vitrectomy in the left eye due to a high clinical suspicion for vitreoretinal lymphoma. This revealed no evidence of malignancy on flow cytometry, and a lack of B lymphocytes in the specimen. No further workup was pursued at that time. He was offered systemic corticosteroids as treatment for the vitritis, but declined.
FIGURE 1. Infrared, optical coherence tomography and color images of an 82-year-old patient diagnosed with primary vitreoretinal lymphoma. (A–C) Drusenoid deposits are visible on infrared imaging that evolved over the course of 6 months and prior to the diagnosis of lymphoma. (D) A vertical line scan through the whitish sub-RPE deposit seen in color photograph (E).
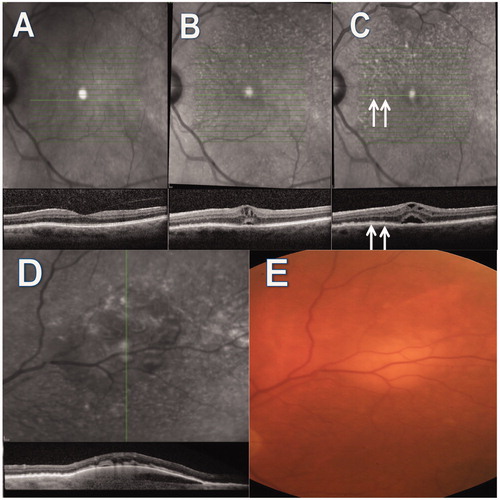
On follow-up examination 3 months later, his visual acuity had declined to 20/40 OD and 20/150 OS, with significant progression of his nuclear sclerosis. OCT revealed new cystoid macular edema (CME) as well as small sub-RPE deposits on infrared OCT images with the appearance of fine drusenoid deposits. These deposits were very difficult to appreciate clinically (or in color photograph ) due to cataract progression but were easily seen on infrared images (). He was treated with an oral corticosteroid taper for the CME and vitritis. Two months later his exam demonstrated increased sub-RPE deposits (, arrows denote correspondence between hyperreflective lesions and sub-RPE deposits) and a new large pigment epithelial detachment with sub-retinal fluid and sub-RPE infiltrate (). Again, due to high clinical suspicion for lymphoma, magnetic resonance imaging (MRI) of the brain was obtained (6 months following his initial vitrectomy). This study was unremarkable. Cerebrospinal fluid analysis was also unremarkable (though flow cytometry was not performed on this sample). Diagnostic vitrectomy was recommended for his right eye, but the patient and family wanted time to consider this option.
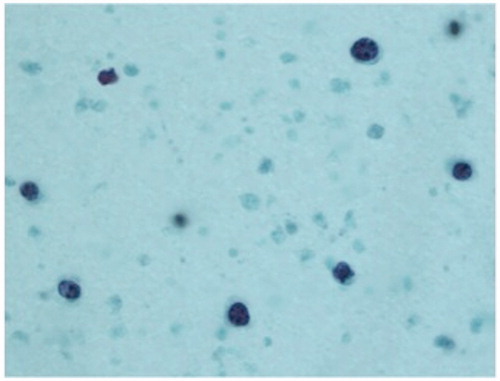
One month later, the patient was hospitalized for mental status changes and follow-up MRI of the brain revealed multiple bilateral enhancing white matter lesions consistent with primary CNS lymphoma. At that time, after consulting with the family and the neuro-oncology team, the decision was made to perform vitrectomy on his right eye, which confirmed the diagnosis of B-cell lymphoma on cytology and flow cytometry. contains an image from the cytologic sample. The patient and family declined additional treatment, and he expired 2 months later.
FIGURE 2. Cytologic specimen from an undiluted vitreous sample in a patient with primary vitreoretinal lymphoma and central nervous system lymphoma, demonstrating atypical lymphoid cells with pleomorphic nuclei and scant cytoplasm. Flow cytometry of this specimen was CD19 and CD20 positive with kappa light chain expression consistent with B-cell lymphoma.
Primary vitreoretinal lymphoma can be difficult to diagnose and, as in this case, despite high clinical suspicion, there is often a delay between initial symptoms and eventual diagnosis.Citation1 Sub-RPE deposits in vitreoretinal lymphoma have been well described and several similar cases have been published with OCT images revealing both discrete and confluent sub-RPE deposits, but in almost all of these cases the tissue diagnosis was made prior to the development of the retinal findings.Citation2–6 We believe that since these deposits are highly specific for vitreoretinal lymphoma,Citation4 this case may add to the discussion regarding the necessity of tissue diagnosis prior to treatment of vitreoretinal lymphoma and CNS B-cell lymphoma,Citation7 and ultimately may aid clinicians in making this difficult diagnosis earlier in the disease coarse, leading to earlier treatment, and hopefully decreased mortality in this disease.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Levasseur SD, Wittenberg LA, White VA. Vitreoretinal lymphoma: a 20-year review of incidence, clinical and cytologic features, treatment, and outcomes. JAMA Ophthalmol. 2013;131:50–55. doi:10.1001/jamaophthalmol.2013.569
- Fardeau C, Lee CPL, Merle-Béral H, et al. Retinal fluorescein, indocyanine green angiography, and optic coherence tomography in non-Hodgkin primary intraocular lymphoma. Am J Ophthalmol. 2009;147:886–894.e1. doi:10.1016/j.ajo.2008.12.025
- Liu TYA, Ibrahim M, Bittencourt M, et al. Retinal optical coherence tomography manifestations of intraocular lymphoma. J Ophthalmic Inflamm Infect. 2012;2:215–218. doi:10.1007/s12348-012-0072-z
- Davis JL. Intraocular lymphoma: a clinical perspective. Eye (Lond). 2013;27:153–162. doi:10.1038/eye.2012.250
- Vasconcelos-Santos DV, De Puy E Souza GH, de Faria BB, et al. Subretinal pigment epithelial infiltrates in primary vitreoretinal lymphoma. J Ophthalmic Inflamm Infect. 2011;1:171. doi:10.1007/s12348-011-0034-x
- Thinda S, Agarwal A. Primary central nervous system lymphoma with ocular involvement. JAMA Ophthalmol. 2013;131:494. doi:10.1001/jamaophthalmol.2013.594
- Arcinue CA, Hochberg F, Neumann R, Foster CS. Diagnostic Criteria for primary ocular lymphoma. Ophthalmology. 2013;120:646–646.e2. doi:10.1016/j.ophtha.2012.09.053

