Abstract
Purpose: The authors report a case of endophthalmitis after intravitreal injection of ranibizumab.
Methods: After searching for extensive laboratory tests to isolate the etiologic agent
Results: The agent was determined as Leuconostoc mesenteroides, gram-positive cocci, vancomycin resistant.
Discussion: Considerations regarding this bacterium were done by calling attention to its rarity, difficulty of isolation, and action on secondary comorbidities as opportunistic pathogen.
Leuconostoc mesenteroides has been reported as a cause of infection in patients with neutropenia and cancer, nosocomial urinary tract infection, prosthetic valve endocarditis, liver transplantation, and AIDS.Citation1 This bacteria is a gram-positive cocci, vancomycin-resistant, and usually opportunistic pathogen. In this case study, we describe an endophthalmitis after intravitreal injection of ranibizumab in a patient with cancer.
Case Report
An 89-year-old white man had a routine uncomplicated intravitreal injection of ranibizumab in the right eye to treat wet age-related macular degeneration. After 48 h, he presented with ocular pain and hyperemia of the right eye. He had a history of prostate cancer for 2 years. The patient began treatment with ranibizumab for age-related macular degeneration with choroidal neovascularization in this eye, 3 months prior to this intravitreal injection, having performed the third injection per month.
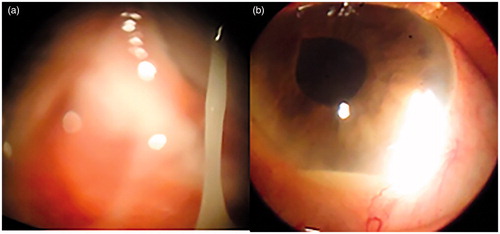
Examination of the eye revealed visual acuity of light perception, hypopyon, and purulent discharge (Figure 1a,b). The intraocular pressure was normal (12 mmHg) and fundus could not be seen due to vitreous opacification. A diagnosis of endophthalmitis was made and vitreous biopsy was carried out urgently, which included intravitreal injection of vancomycin and amikacin at the end of the procedure. Blood and urine cultures and PCR test were performed. Initial microbiologic examination of vitreous samples revealed gram-positive cocci and he was treated with systemic gatifloxacin. He also received topical mofloxacin and cycloplegics drops. After 72 h, cultures of blood and vitreous revealed Leuconostoc mesenteroides that was sensitive to ceftazidime, gentamicin, ciprofloxacin, amikacin, gatifloxacin, and mofloxacin and resistant to vancomycin. He needed more 2 intravitreal injections of amikacin with 48 h of interval to improve the symptoms. His eye evolved to Phthisis bulbi after 2 months. After a couple days, the result of the PCR test revealed the same microorganism (Leuconostoc) with no other evidence of co-infection.
Discussion
Until recently, the Leuconostoc (environmental organisms), which are usually found on vegetables and food products, were widely considered nonpathogenic and of limited clinical importance.Citation2 Buu-Hoi et al. reported the first cases of Leuconostoc infection in humans. The Leuconostoc infection occur naturally on various foods, and gastrointestinal colonization has been demonstrated for patients with previous gastrointestinal disease, surgery, and antibiotic therapy, suggesting that the gastrointestinal tract can be a potential reservoir for infection.Citation2,Citation3 The frequency of its infection may be underestimated. Leuconostoc species are difficult to detect with routine methods and can be misidentified easily as Lactobacillus, alphahemolytic Streptococci, Pediococcus, Enterococcus, or Lactococcus.Citation2
The skin and digestive tract are assumed to play important roles as routes of entry into the body. Leuconostoc species can cause bacteremia, catheter-related infections, meningitis, urinary tract infections, osteomyelitis, or liver dysfunction, among other problems. Risk factors for infection by Leuconostoc species are placement of central venous catheters, a history of use of vancomycin, liver failure, chronic renal insufficiency treated with hemodialysis, extensive burns, and compromised immunity.Citation3,Citation4
In our case, the nosocomial transmission was ruled out because it was the only case of infection caused by Leuconostoc in our ophthalmological surgical center. The same surgeon made a total of 6 intravitreal injections of ranibizumab in the same morning of the patient's procedure. Our hospital had done 500 intravitreal injections of ranibizumab since 2008 and had only this case of endophthalmitis.
The elderly patient had a previous history of prostatic cancer associated with chemotherapy, which is compatible with risk factors of Leuconostoc infection. The authors think that the hypothesis of an endogenous endophthalmitis would be possible, because he had a positive bacteremia for Leuconostoc, but with less chance because no other signs of systemic infection has occurred. Another alternative is that the patient had endophthalmitis caused by fecal contamination from his hands. Anyway, the source of microorganism originates from the gastrointestinal tract.
In summary, Leuconostoc infection is important to remember as a potential cause of endophthalmitis and is listed in the group of vancomycin-resistant microorganisms.Citation4 Age-related macular degeneration (ARMD) is the leading cause of blindness in developed countries. Since 2005, the advent of antivascular endothelial growth factor (anti-VEGF) drugs for the treatment of the neovascular ARMD has changed the management of this disease. The prognosis of this disease has improved and the intravitreous injections have low incidence of adverse events, but each intravitreous injection increases the risk of complications a little more.Citation5
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Quiros JCB, Munoz P, Cercenado E, et al. Leuconostoc species as a cause of bacteremia: two cases reports and literature review. Eur J Clin Microbiol Infect Dis. 1991;10:505–509
- Facklam R, Elliott JA. Identification, classification, and clinical relevance of catalase-negative, gram-positive cocci, excluding streptococci and enterococci. Clin Microbiol. 1995;8:479–495
- Hoi B, Branger AC, Acar JF. Vancomycin-resistant streptococci or Leuconostoc spp. Antimicrob Agents Chemother. 1985;28:458–460
- Kumudhan D, Mars S. Leuconostoc mesenteroids as a cause of post-operative endophthalmitis: case report. Eye. 2004;18:1023–1024
- Jager RD, Aiello LP, Patel SC, Cunningham ET Jr. Risks of intravitreous injection: a comprehensive review. Retina. 2004;24:676–698