Serpiginous choroiditis is a choroiditis that shows centrifugal serpiginous extension outward from the optic disc,Citation1,Citation2 and is speculated to primarily affect the choriocapillaris and retinal pigment epithelium.Citation1 Photoreceptor inner segment and outer segment junction (IS/OS) loss and increased reflectance of the choroid have been reported on spectral-domain optical coherence tomographyCitation3; however, there have been no reports on detailed choroidal morphology.
Indocyanine green angiography (ICGA) is a useful method to assess the activity of choroidal lesions in serpiginous choroiditis.Citation1,Citation2 However, ICGA may rarely cause anaphylactic shocks. Therefore, alternative noninvasive tools are needed for patients allergic to contrast agents, because serpiginous choroiditis often recurs with a chronic clinical course.
Laser speckle flowgraphy (LSFG) can be used for noninvasive evaluation of circulation of ocular tissues and calculation of the mean blur rate (MBR), a quantitative index of relative blood flow velocity.Citation4 Because the MBR is believed to originate mainly from the choroid, the value is associated with choroidal circulation hemodynamics.Citation4 Composite map images of the MBR can be used for noninvasive visualization of choroidal vasculature, and the resolution is comparable to that of ICGA.Citation5 Although LSFG does not provide an absolute value for the blood flow, this technique has the advantage of allowing precise and repeated measurements of choroidal circulation at various intervals during the time course of diseases.Citation4
We have recently revealed that the MBR decreased in the acute stage of the choroidal inflammatory diseases, including Vogt-Koyanagi-Harada diseaseCitation6 and acute zonal occult outer retinopathy,Citation7 whereas it increased in acute central serous chorioretinopathyCitation8 due to a noninflammatory (i.e. sympathetic or adrenergic) etiology. Thus, investigation into the pattern of the MBR changes during the time course of a disease appears meaningful not only to evaluate its activity but to elucidate its pathogenesis. Here we report new observations by using LSFG and enhanced-depth imaging optical coherence tomography (EDI-OCT) in a patient with serpiginous choroiditis.
A 40-year-old woman was referred to our hospital for assessment of a choroidal abnormality detected at another hospital despite no subjective symptoms. The patient had no remarkable medical or family history.
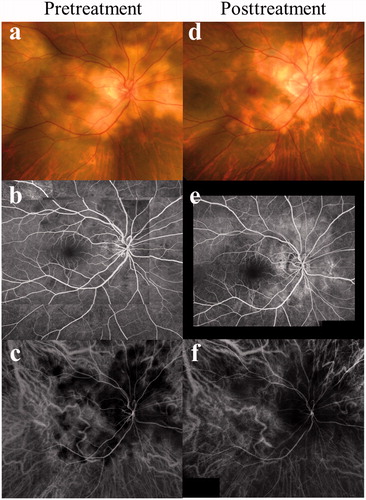
Visual acuities were 1.2 OD and 1.5 OS. Her left eye was normal. There were no abnormal findings in the anterior chamber or anterior vitreous of the right eye, but funduscopic examination showed yellow-white patchy geographic choroiditis plaques with a serpiginous distribution outward from the optic disc (). Fluorescein angiography showed initial faint hypofluorescent patches with poorly defined borders and late staining within the choroiditis plaques (). ICGA showed hypofluorescence from the initial phase corresponding to the plaques (). These angiographic findings were compatible with the active phase of serpiginous choroiditis.Citation2 Serological test results and antibody titers for syphilis, toxoplasmosis, cytomegalovirus, herpes simplex virus, and herpes zoster virus were negative. QuantiFERON was also negative and chest x-ray showed no abnormalities. Serum angiotensin-converting enzyme was within normal limit. The patient was diagnosed with acute-stage serpiginous choroiditis OD, and oral prednisolone therapy (30 mg/day) was initiated and tapered for 8 months. Seven months after treatment (during 10 mg/day of prednisolone), visual acuity remained unchanged and the exudates had scarred resulting in serpiginous-shaped atrophy with no macular involvement (). Fluorescein angiography revealed hyperfluorescence corresponding to the scar lesions (). On ICGA, the hypofluorescent regions decreased compared to those at the initial visit (). The patient has never suffered any recurrences so far (for 11 months since the first visit).
FIGURE 1. Photographs of the right eye at the initial visit (a–c) and 7 months after systemic prednisolone therapy (d–f) in a patient with serpiginous choroiditis. (a) Panorama fundus photograph showing yellow choroiditis plaques with a serpiginous distribution outward from the optic disc. (b) Fluorescein angiography of the venous phase showing initial faint hypofluorescent patches with ill-defined margin within the choroiditis plaques. (c) Indocyanine green angiography (ICGA) of the initial phase showing hypofluorescence corresponding to the plaques. (d) Choroiditis plaques developed serpiginous-shaped scar lesions sparing the macula. (e) Fluorescein angiography revealed hyperfluorescence corresponding to the scar lesions (d). (f) On ICGA, the hypofluorescent areas decreased compared to those at the initial visit (c).
LSFG measurements using LSFG-NAVI (Softcare, Fukuoka, Japan) were conducted 3 consecutive times for each circle before treatment and 7 months after initiation of systemic prednisolone therapy. All measurements were performed in the patient's sitting position. The current study was approved by the ethics committee of Hokkaido University Hospital. Informed consent was obtained after an explanation of the nature and possible consequences of the study, which followed the standard of care outlined in the Declaration of Helsinki. To evaluate the changes in the relative blood flow velocity, circles were set at a lesion site (circle 1; ) and a normal-appearing retinal site (circle 2; ) within the macular area of the patient's right eye. The positions of circles were determined manually by comparing the fundus photograph and the LSFG color map images. The MBR was automatically calculated in each circle using the LSFG Analyzer software (v 3.0.47; Softcare). To evaluate changes in average MBR, the changing rate of average MBR against the initial baseline value was utilized, as previously described,Citation7,Citation8 since MBR is a quantitative index of the “relative” blood flow velocity.
FIGURE 2. Laser speckle flowgraphy (LSFG) (a, b) and enhanced-depth imaging optical coherence tomography (EDI-OCT) (c, d) findings at pretreatment (a, c) and 7 months after treatment (b, d). (a) Panorama color map of LSFG showing decreased mean blur rate (MBR) over a wider area (arrowheads) than the hypofluorescent area observed on ICGA (). Blue and red indicate decreased and increased MBR, respectively. (b) The area of decreased MBR diminished in the posterior pole compared to that of the initial visit (a). (c) Horizontal EDI-OCT through the fovea showing markedly increased choroidal thickness and a hyperreflective lesion at subretinal pigment epithelium level (arrow) with shallow serous retinal detachment corresponding to the peripapillary choroiditis plaques. (d) Central choroidal thickness dramatically decreased with resolution of pigment epithelial detachment. (e) The graph shows the changes in the average MBR and subfoveal choroidal thickness during systemic corticosteroid therapy. The average MBR showed 27.4% increase in a lesion site (circle 1 shown in ) and 9.7% increase in a normal-appearing retinal site (circle 2 shown in ) at 7 months after treatment, compared to the pretreatment level (100%). Subfoveal choroidal thickness decreased from 713 µm to 330 µm.
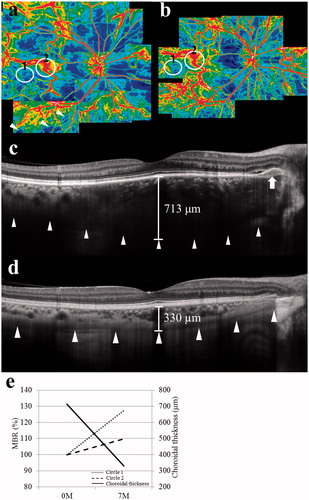
Color map image revealed decreased MBR over a wider area (, arrowheads) than the hypofluorescent regions observed on ICGA (). Seven months after treatment, the areas of decreased MBR (blue) apparently diminished in the posterior pole (). The average MBR at circles 1 and 2 was 6.3 ± 0.6 and 20.7 ± 0.5 before treatment and 7.9 ± 0.05 and 22.7 ± 2.3 after treatment. When the changing rates of the macular flow were compared with the mean MBR levels before treatment (100%), 27.4% increase in circle 1 and 9.7% increase in circle 2 were noted after treatment (). Ocular perfusion pressure (OPP) was 36.7 and 33.4 mmHg before and after treatment, respectively.
Before treatment, horizontal EDI-OCT through the fovea showed a marked increase in subfoveal choroidal thickness together with an intact IS/OS line at the fovea. Three of the authors (A.T., Y.H., and M.S.) measured the markedly thickened choroid with the average value of 713.3 ± 4.5 µm. Further, there was a hyperreflective lesion at the subretinal pigment epithelium level (, arrow) with shallow serous retinal detachment corresponding to the peripapillary choroiditis plaques. Seven months after treatment, subfoveal choroidal thickness dramatically decreased to 330 µm OD with resolution of these subretinal lesions ().
In the present case with serpiginous choroiditis, systemic corticosteroid treatment led to scar formation of subretinal exudates with a substantial increase in choroidal blood flow velocity. During the follow-up, the patient's OPP showed no remarkable change, whereas the relationship between choroidal blood flow and OPP is known to be linear in physiologic conditions. In addition, the effect of corticosteroids per se on MBR values was suggested to be negligible or minimal, if any.Citation7 Accordingly, the increase in MBR in this case was thought to be unaffected by corticosteroid application or by systemic circulation. Therefore, our present data suggest that systemic corticosteroid therapy ameliorated choroidal circulation via suppression of inflammatory reactions in serpiginous choroiditis.
The present observation regarding the LSFG in serpiginous choroiditis was comparable to our previous findings on Vogt-Koyanagi-Harada disease.Citation6 In choroiditis, it is reasonable to think that choroidal blood flow is impaired during the acute stage of inflammation. Furthermore, the present data showing the wider areas with attenuated MBR than the ICGA-based hypofluorescent regions suggest that LSFG can detect choroidal lesions in serpiginous choroiditis with greater sensitivity than ICGA. Therefore, these results indicate that LSFG may be an additional and noninvasive tool for detecting the potential expansion of choroiditis lesions together with quantitative monitoring of disease activity. To the best of our knowledge, this is the first report to reveal the usefulness of LSFG in serpiginous choroiditis.
Our EDI-OCT results first demonstrated that choroiditis plaques in serpiginous choroiditis were located at the subpigment epithelium level. This observation is compatible with a previous clinicopathologic study showing that the most affected layer was choriocapillaris.Citation1,Citation9 However, because LSFG can basically measure blood flow in deeper layers of the choroid,Citation5 markedly increased thickness and decreased circulation in the choroid of this patient suggest that choroidal inflammation extended to not only inner layers but also deeper tissues. This speculation is consistent with and supported by previous histopathologic findings in which moderate diffuse lymphocytic infiltrates were observed throughout the choroid.Citation1,Citation9 Further detailed studies are needed to investigate morphology and function of the choroid in choroiditis, including serpiginous choroiditis.
In conclusion, systemic corticosteroid treatment to a patient with serpigious choroiditis successfully attenuated the disease activity together with circulatory improvement and thickness normalization in the choroid. These changes in choroidal parameters demonstrated the “inflammatory” pattern, in consistence with previous LSFG and EDI-OCT data on Vogt-Koyanagi-Harada disease.Citation6,Citation10
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Lim WK, Buggage RR, Nussenblatt RB. Serpiginous choroiditis. Surv Ophthalmol. 2005;50:231–244
- Khanamiri HN, Rao NA. Serpiginous choroiditis and infectious multifocal serpiginoid choroiditis. Surv Ophthalmol. 2013;58:203–232
- Arantes TEF, Matos K, Garcia CR, et al. Fundus autofluorescence and spectral domain optical coherence tomography in recurrent serpiginous choroiditis: case report. Ocul Immunol Inflamm. 2011;19:39–41
- Sugiyama T, Araie M, Riva CE, et al. Use of laser speckle flowgraphy in ocular blood flow research. Acta Ophthalmol. 2010;88:723–729
- Watanabe G, Fujii H, Kishi S. Imaging of choroidal hemodaynamics in eyes with polypoidal choroidal vasculopathy using laser speckle phenomenon. Jpn J Ophthalmol. 2008;52:175–181
- Hirose S, Saito W, Yoshida K, et al. Elevated choroidal blood flow velocity during systemic corticosteroid therapy in Vogt-Koyanagi-Harada disease. Acta Ophthalmol. 2008;86:902–907
- Saito M, Saito W, Hashimoto Y, et al. Correlation between decreased choroidal blood flow velocity and the pathogenesis of acute zonal occult outer retinopathy. Clin Exp Ophthalmol. 2014;42:139--150
- Saito M, Saito W, Hashimoto Y, et al. Macular choroidal blood flow velocity decreases with regression of acute central serous chorioretinopathy. Br J Ophthalmol. 2013;97:775–780
- Wu JS, Lewis H, Fine Sl, et al. Clinicopathologic findings in a patient with serpiginous choroiditis and treated choroidal neovascularization. Retina. 1989;9:292–301
- Maruko I, Iida T, Sugano Y, et al. Subfoveal choroidal thickness after treatment of Vogt-Koyanagi-Harada disease. Retina. 2011;31:510–517

