Scedosporium apiospermum is a common soil fungus with a worldwide distribution. Environmental isolations have been made from sewage sludge, polluted water, and manure of poultry and cattle. Ocular infection is infrequently associated with it. We report a case of post-traumatic fungal corneal ulcer that developed endophthalmitis due to Scedosporium apiospermum.
A 32-year-old, healthy, nondiabetic male patient presented to us with complaints of pain, redness, and decrease in vision in his left eye (OS) for 1 month. There was a history of injury with vegetable matter 1 month back. The patient had received a short course of oral fluconazole (200 mg) and was on topical natamycin (5%) hourly, moxifloxacin (0.5%), and atropine eyedrops (1%).
On examination, his best corrected visual acuity (BCVA) in OS was perception of light positive (PL) with accurate projection of rays. Minimal lid edema was noted. Anterior segment examination of the OS showed the presence of a 5 × 7.5 corneal ulcer involving the visual axis with endo exudates and 1.5-mm hypopyon (). There was no view of the fundus. BCVA in the right eye (OD) was 6/6, N6. Anterior and posterior segment examination of the OD was within normal limits. A corneal scraping was done. Fungal filaments were noted in the KOH mount. Ultrasound examination of the left eye showed few dot echoes in the vitreous with attached retina. The patient was started on topical natamycin (half hourly), fortified amphotericin-B (0.25%, half hourly), and oral ketoconazole (200 mg twice a day). The patient presented 4 days later with increase in size of the ulcer and increased exudates in anterior chamber. Ultrasonography showed few dot echoes. The patient was advised to undergo therapeutic penetrating keratoplasty (TPK) in the OS.
Figure 1. (A) Clinical photograph of the left eye showing corneal ulcer with hypopyon. (B) Ultrasound of the left eye showing significant vitreous echoes with attached retina.
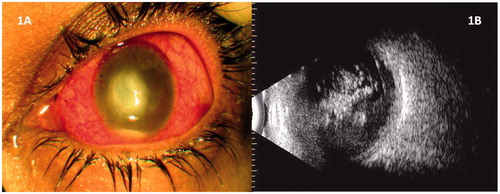
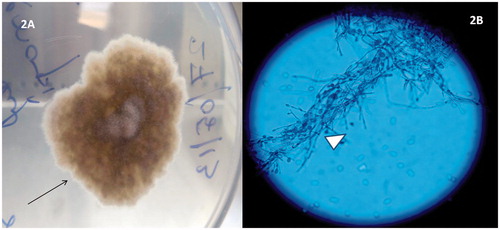
A 9-mm corneal graft was used. Amphotericin-B (5 µg in 0.1 mL) was injected intracamerally at the end of the procedure. Following surgery, the patient was put on the same regimen that had been used in the preoperative period. However, there was progressive increase in anterior chamber exudation in the immediate postoperative period. A yellowish glow could be noted in the pupillary axis. A repeat ultrasound of OS showed significant increase in vitreous echoes with an attached retina (). The patient underwent 23-G pars plana vitrectomy. Undiluted vitreous aspirate was obtained and sent for microbiology. A core vitrectomy was done. The patient received intravitreal vancomycin (1 mg in 0.1 mL) and amphotericin B (5 µg in 0.1 mL) at the end of the surgery. Scedosporium apiospermum growth was obtained in culture (). The patient received 3 more doses of intravitreal amphotericin B in the postoperative period. At final follow-up 6 weeks following vitrectomy, BCVA in the OS was no PL and the eye had become phthisical.
Figure 2. (A) Sabouraud dextrose agar showing growth of Scedosporium apiospermum (black arrow). (B) Lactophenol blue mount showing fungal filaments characteristic of Scedosporium apiospermum (white arrowhead).
Scedosporium apiospermum—the anamorph (asexual state) of the ascomycete Pseudallescheria boydii—is a significant opportunist with high levels of anti-fungal resistance. Previously it was mainly known to be associated with traumatic, subcutaneous infections, and asymptomatic pulmonary colonization, but in recent years, new disease entities have evolved. With a frequency of 9%, S. apiospermum is among the most common filamentous fungi colonizing the lungs of cystic fibrosis patients.Citation1 S. apiospermum is a rare cause of endophthalmitis with very few cases of exogenous endophthalmitis being reported in the English literature.
Ikewaki et al.Citation2 have reported a case of peribulbar fungal abscess and endophthalmitis due to S. apiospermum following posterior subtenon injection of traimcinolone acetonide. The patient responded well to treatment and there was no recurrence of the disease at 6 months follow-up. Zarkovic et al.Citation3 have reported a case of traumatic endophthalmitis due to S. apiospermum. The patient was successfully treated with a combination of intravitreal and systemic voriconazole. The patient achieved a BCVA of 6/12 at 10 months follow-up. A case of S. apiospermum keratomycosis with secondary endophthalmitis has been described by Leck et al.Citation4 Although infection was controlled, vision was finally lost due to secondary glaucoma. Ksiazek et al.Citation5 have described a case of fungal panophthalmitis following S. apiospermum keratitis. The eye had to be ultimately eviscerated.
Our patient presented to us initially with keratomycosis of 1-month duration. The patient had already received anti-fungal treatment for 1 month. However, there was gradual deteroriation in the clinical profile and the patient had to undergo TPK followed by vitrectomy. S. apiospermum was obtained from the vitreous sample. Due to logistic reasons we could not perform a drug sensitivity profile. Inspite of all active management, the eye became phthisical at final follow-up. There have been few reports in which the patients have done well with prompt antifungal theraphy.Citation2,Citation3 However, Leck et al.Citation4 and Ksiazek et al.Citation5 have reported poor outcomes even after instituting prompt anti-fungal therapy. To conclude, S. apiospermum is a rare cause of endophthalmitis with poor outcomes. Fungal infection should always be suspected in any case of keratitis with a history of vegetable matter trauma. Outcomes of fungal keratitis have improved with the advent of newer anti-fungal drugs. However, cases with intraocular spread are associated with poor outcomes. Prompt treatment can sometimes be associated with good outcomes.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Cimon B, Carrere J, Chazalette JP. Fungal colonization and immune response to fungi in cystic fibrosis. J Mycol Med. 1995;5:53–56
- Ikewaki J, Imaizumi M, Nakamuro T, et al. Peribulbar fungal abscess and endophthalmitis following posterior subtenon injection of triamcinolone acetonide. Acta Ophthalmol. 2009;87:102–104
- Zarkovic A, Guest S. Scedosporium apiospermum traumatic endophthalmitis successfully treated with voriconazole. Int Ophthalmol. 2007;27:391–394
- Leck A, Matheson M, Tuft S, et al. Scedosporium apiospermum keratomycosis with secondary endophthalmitis. Eye (Lond). 2003;17:841–843
- Ksiazek SM, Morris DA, Mandelbaum S, Rosenbaum PS. Fungal panophthalmitis secondary to Scedosporium apiospermum (Pseudallescheria boydii) keratitis. Am J Ophthalmol. 1994;118:531–533

