Abstract
A 47-year-old man developed a painful right red eye for 72 hours with a 20/25 decreased visual acuity. He had no medical history. Slit-lamp examination revealed a painful nodular scleritis at the equator of the globe in the infero-temporal quadrant. There was a moderate intraocular inflammation in the anterior segment. Fundus examination revealed a grade 1 hyalitis and a focal retinitis with vasculitis and arterio-veinous occlusion toward the scleritis zone. Syphilis and HIV serology were positive and the scleritis resolved 5 days after a penicillin G medication. Syphilitic scleritis are relatively uncommon.
Syphilis is primarily a sexually transmitted infection caused by a spirochete: Treponema pallidum. Ocular manifestations of syphilis can affect any eye tissue but usually the infection is located in the uveal tract thus leading to uveitis. Overall, 2.5–5% of uveitis cases seen in clinical centers of reference are caused by syphilis.Citation1 We report here a case of syphilis presenting as scleritis, which is relatively uncommon and rarely found in the literature.Citation2–6
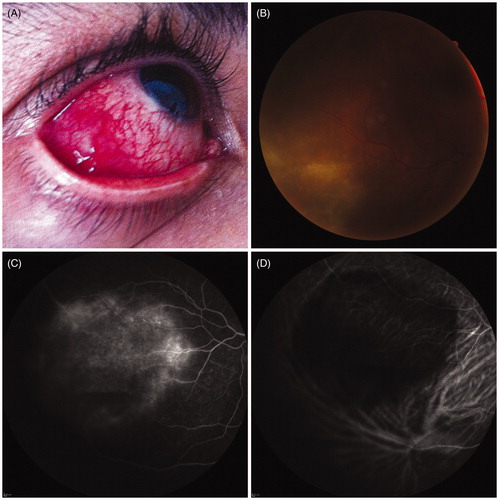
A 47-year-old man with no significant medical or surgical history presented with redness and pain in his eye for the past 72 h. He complained of blurred vision in his right eye and best corrected visual acuity was 20/25 OD and 20/20 OS. The slit-lamp examination unveiled a painful nodular scleritis located at the equator of the globe in the infero-temporal quadrant (). Upon examination the cornea showed some fine white keratic precipitates and a moderate intraocular reaction in the anterior chamber with grade 1+ cells. Intraocular pressure was 14 mmHg OU. The dilated fundus examination revealed a grade 1+ hyalitis and a focal area of retinitis associated with vasculitis and arteriovenous occlusions above the area of the scleritis associated with mild disc edema in his right eye (B). For the left eye, the dilated fundus examination was normal. Fluorescein angiography (FA) showed early pinpoint leaks and a large area of hyperfluorescence with a leakage of the optic disc during the late transit phase of the FA (C). Infracyanine green angiography (ICG) unveiled a large hypofluorescent area during the early and late transit phase of the ICG (D). Optical coherence tomography (SD-OCT) revealed the presence of echoes within the vitreous cavity and peripapillary nerve fiber layer thickening consistent with the edema of the optic disc. Macular volume was normal without any sign of macular edema.
Figure 1. (A) Initial presentation: a painful nodular scleritis is present at the equator of the globe (B) Fundus picture: retinis and arteriovenous occlusive aspect (C) Fluorescein angiography early transit phase revealing a diffuse leakage with occluded vessels and some pinpoints (D) ICG angiography early transit phase revealing a large hypo-fluorescent zone toward the scleritis.
These findings were consistent with scleritis and underlying retinitis, vasculitis, and mild vitritis of the infero-temporal periphery. We started intravenous acyclovir therapy to treat a potential herpetic infection associated with NSAID eyedrops. Anterior chamber paracentesis was performed to look for PCR positivity along with a systemic workup. At day 2, the anterior chamber sample was negative for HSV and CMV (real-time PCR). At day 3, the serological responses for syphilis and HIV were both positive. MRI and lumbar puncture were performed to exclude neurosyphilis. The MRI was normal, the cerebrospinal fluid (CSF) was clear, and no syphilis antibodies were found. The patient’s CD4 cell count was normal (>500 cells/mm3). We implemented IV penicillin G therapy and the scleritis resolved 5 days later. Visual acuity improved to 20/20 OD, the inflammation in the anterior and posterior chambers of the right eye had regressed, and the dilated fundus examination revealed damages consisting of vessel occlusion with a white matter without neovascularization or pigmented lesions.
Syphilis is called the “great imitator” because many signs and symptoms mimic other diseases, so it may present as scleritis as well as the more common uveitis, vascularitis, or optic neuritis. A high level of clinical suspicion is required to make the appropriate diagnosis of ocular syphilis due to its variable clinical presentation. This is why syphilis must be systematically included as part of the uveitis and scleritis workup.
The incidence of syphilis in scleritis cases is unknown and very few studies are available in the literature. Since 2000, the incidence of syphilis has dramatically increased in Europe and the United States. Worldwide, there are an estimated 12 million new cases per year, with 90% of them occurring in developing countries. These increases in reported cases concern most often homosexual males and persons co-infected with HIV.Citation7 In our reported case, the patient had a high-risk sexual behavior with an HIV-positive man. Severe ocular manifestations of HIV are commonly seen and this could explain this atypical ocular scleritis case.Citation8,Citation9
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433–441
- Wilhelmus KR, Yokoyama CM. Syphilitic episcleritis and scleritis. Am J Ophthalmol. 1987;104:595–597
- Casey R, Flowers CW Jr, Jones DD, Scott L. Anterior nodular scleritis secondary to syphilis. Arch Ophthalmol. 1996;114:1015–1016
- Moloney G, Branley M, Kotsiou G, Rhodes D. Syphilis presenting as scleritis in an HIV-positive man undergoing immune reconstitution. Clin Exp Ophthalmol. 2004;32:526–528
- Win PH, Gonzales CR, Young T, et al. Syphilitic scleritis and choroidal malignant melanoma of the same eye. Semin Ophthalmol. 2007;22:193–195
- Lee SB, Kim KS, Lee WK, et al. Ocular syphilis characterised by severe scleritis in a patient infected with HIV. Lancet Infect Dis. 2013;13:994
- Puech C, Gennai S, Pavese P, et al. Ocular manifestations of syphilis: recent cases over a 2.5-year period. Graefes Arch Clin Exp Ophthalmol. 2010;248:1623–1629
- Lynn WA, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. 2004;4:456–466
- Gaudio PA. Update on ocular syphilis. Curr Opin Ophthalmol. 2006;17:562–566

