Abstract
Purpose: To evaluate the short-term efficacy of intravitreal adalimumab (IVA) for the treatment of eyes with active noninfectious uveitis.
Methods: Consecutive eyes with active noninfectious uveitis were injected with IVA at 0, 2, then every 4 weeks for total of 26 weeks.
Results: Six out of 7 patients (12 of 13 eyes) completed 26 weeks of treatment. One patient (1 eye) failed treatment. Seven out of 12 eyes had improvement of ≥2 ETDRS lines. Three out of three eyes had resolution of anterior chamber cells. And 9 of 10 eyes with vitreous haze had zero haze at 26 weeks. Five out of 8 eyes with macular edema had complete resolution. Median fluorescein angiography score improved from 14 to 4 on last follow-up.
Conclusions: IVA was effective in controlling the inflammation, decreasing the macular edema, and improving the best corrected visual acuity in the majority of eyes in this series.
Uveitis is an immune-mediated inflammation against infections and/or autoantigens in the eye that may result in permanent vision loss if not adequately treated.Citation1,Citation2 In many cases with noninfectious uveitis, systemic corticosteroids and immunosuppressive therapy are required for control of the inflammation. The 3 widely used classes of immunosuppressive agents include antimetabolites, T-cell inhibitors, and alkylating agents, all being slow acting with a clinical response between 52 and 76%.Citation3,Citation4 Long-term treatment may be complicated by side effects, such as renal and hepatic toxicity, hypertension, and hematologic abnormalities. Recent studies attest to the important role of tumor necrosis factor alpha (TNFα) and interleukins in the pathogenesis of ocular inflammation.Citation5 TNFα may induce the expression of chemokines, adhesion molecules, and cytokines that are involved in the inflammatory process. Inhibition of TNFα activity results in suppression of infiltrating macrophages, hence preventing tissue destruction in active uveitis.Citation6 Studies involving animal models of uveitis and clinical studies have demonstrated the presence of TNFα in the serum and aqueous humor of subjects with active uveitis.Citation7–9 Two commercially available anti-TNFα agents (infliximab and adalimumab) are currently used as off-label treatment of noninfectious uveitis.Citation10,Citation11 Infliximab was shown to effectively control inflammation in up to 80% of refractory uveitis with fairly few serious adverse events.Citation12,Citation13 Adalimumab was effective in around 80% of patients with inflammation and cystoid macular edema (CME) in the setting of active noninfectious uveitis.Citation14–16 The use of intravitreal anti-TNFα deserves further investigation, especially in cases where the inflammation is localized to the eye or where systemic immunosuppressive therapy is not tolerated. Due to the significant role of TNFα in active uveitis, we aim to study the short-term efficacy of intravitreal adalimumab injections in a pilot study of subjects with active noninfectious uveitis. This followed a successful trial in 2 blind eyes of 2 patients with acute panuveitis where intraocular inflammation decreased after intravitreal adalimumab (Mansour A, unpublished data).
Materials and Methods
Study Design
We conducted an open-label, single-center, prospective, nonrandomized, interventional case series of 7 consecutive patients (13 eyes) with active noninfectious uveitis. The study protocol was approved by the institutional review board with adherence to the tenets of the Declaration of Helsinki. The study was registered (www.clinicaltrials.gov under the number NCT00855608). The off-label use of the drug, potential risks, and benefits were discussed with the patients, and written informed consents were obtained. Inclusion and exclusion criteria are discussed in . Baseline assessments included medical and ocular history, best corrected visual acuity (BCVA) measurement with the ETDRS chart, applanation tonometry, slit-lamp examination, fundus examination, electroretinography (ERG), optical coherence tomography (OCT), and fluorescein angiography (FA). Baseline OCT was obtained using the Cirrus HD OCT Optical (Carl Zeiss Medical, Dublin, CA). Blood tests, including complete blood count (CBC) and testing for serum glutamate pyruvate transaminase (SGPT), chest radiography, purified protein derivative (PPD) skin test, and pregnancy test were performed when applicable. Patients diagnosed with latent tuberculosis, defined as a PPD skin conversion consisting of an induration of ≥10 mm without radiographic or clinical evidence of disseminated or pulmonary disease, were required to receive anti-tuberculosis prophylaxis at least 3 weeks before the first dose of adalimumab. Patients with pars planitis were required to undergo magnetic resonance imaging of the brain to rule out demyelinating disease.
TABLE 1. Inclusion and exclusion criteria for participation in study.
The eye was prepped and rinsed with 5% povidone–iodine solution. After subconjunctival lidocaine 1% injection, 0.03 mL (1.5 mg) of fresh adalimumab (Humira, Abbott Laboratories, Abbott Park, IL) was injected intravitreally using a 30-gauge needle 3.5 mm from the limbus. The fundus was assessed at this time and 30 min after the injection. Patients were followed up every 2 days the first week, reinjected at 2 weeks, then reinjected monthly for a total of 7 injections. The last assessment was 1 month after the seventh injection. Patients with deterioration in BCVA of two or more lines or worsening of the ocular inflammation by 2+ cells/haze or more at any time during follow-up were withdrawn from the study. Patients with no or minimal improvement (<2+ cells/haze, fluorescein leakage, and vascular staining) and stable ERG received a higher dose of subsequent injections (2.5 mg/0.05 mL). Follow-up visits involved BCVA, applanation tonometry, slit-lamp examination of the anterior and posterior segments, dilated indirect ophthalmoscopy, and OCT, all carried out by the same personnel at every visit. Fluorescein angiography was done prior to the intravitreal injection at every visit. Blood tests and ERG were repeated every 3 months. The laboratory evaluation included CBC and SGPT to rule out any systemic side effect of adalimumab.
BCVA was measured according to the ETDRS protocol adapted by the Age Related Eye Disease Study. A change of ±0.2 logMAR (±10 letters) was chosen as the standard for worsening or improvement in visual acuity. Inflammatory activity of the anterior and posterior chamber was scored according the SUN classification.Citation17 Anterior chamber cells and vitreous haze were given a grade from 0 to 4. Worsening of the inflammatory activity was defined as a two-step increase in the grade of inflammation. FA transits were graded by a masked grader according to the angiography scoring for uveitis working group.Citation18 During treatment with intravitreal adalimumab (IVA), no change in systemic, topical, or local corticosteroids nor systemic immune suppressive therapy was permitted. In case of uncontrolled inflammation requiring addition of corticosteroids or immune suppressive therapy, the patient was removed from the study.
Outcome Measures
The main outcomes measured at 26 weeks included the change in the grade of inflammatory cells/haze in the vitreous (1+ to 4+), the median change from baseline in FA score and in central retinal thickness (CRT), and change in ERG results. Other endpoints pertaining to visual acuity included the median change from baseline in BCVA, and the proportion of patients who gained 2 or more lines of BCVA.
Statistical Analysis
Clinical data obtained were analyzed using SPSS version 20.0 (IBM/SPSS Inc., Chicago, IL). Descriptive statistics were reported as median and interquartile range (IQR) for continuous variables, and the number and percentage for categorical ones. The Wilcoxon signed rank test was used to analyze the difference between the last visit to the baseline measurements of visual acuity (logMAR), total FA score, and CRT. All eyes were analyzed together, then the worst eyes were stratified together and analyzed similarly. p Value <0.05 was considered to be statistically significant.
Results
Seven consecutive patients with active noninfectious uveitis participated in the study between September 2012 and September 2013. Six patients had inflammation in both eyes and were treated bilaterally. There were 5 males and 2 females with a median age of 37.5 years (range 19–48). The median duration of uveitis prior to enrollment was 48 months (range: 4–96). lists the demographic and diagnostic details of the patients. Thirteen eyes were included in the study protocol and the baseline assessment is detailed in . Six of 7 patients were on no systemic or topical therapy at initiation of the study. One patient was on taper regimen of systemic corticosteroids and cyclosporine over 2 months. During the last 4 months of the study none of the patients were on any other kind of treatment. Six patients completed the protocol successfully and received a total of seven injections in each eye over 26 weeks. One eye of 1 patient failed the treatment and was removed from the study due to worsening of both inflammation and visual acuity after the fourth injection (that patient was subsequently treated with systemic and local corticosteroids with return to baseline BCVA).
TABLE 2. Demographics of enrolled patients.
TABLE 3. Parameters of enrolled patients at baseline compared to 26 weeks.
Seven of 12 eyes gained two or more ETDRS lines by the end of the study while 5 eyes gained zero to one line of vision. The median logMAR improved from 0.3 at baseline to 0.0485 on last visit (p = 0.003). There was a mean gain of 11.9 letters on last follow-up for the 13 eyes. Visual improvement was noted as early as the 2-week visit, as illustrated in .
TABLE 4. The progression of parameters over 26 weeks.
Five of the 8 eyes with cystoid macular edema on the first visit had resolution of the edema by last visit and the median time to resolution was 6 weeks (range: 2–26) (). The median CRT improved from 317 μm at baseline to 277 μm on the last visit (p = 0.021) (, ). All 3 eyes with anterior chamber cells grade of 1+ or more had resolution of the cells by 2 weeks and the 9 eyes with vitreous haze grade of 1+ or more had resolution of the haze with a median time to resolution of 6 weeks (range: 2–26) (, ).
FIGURE 1. Pattern 1 shows a progressive resolution of CME and significant improvement at 2 weeks with complete resolution after the second injection that persisted throughout the study. Pattern 2 shows a two-phase improvement: very fast initial improvement of CME noted at 2 days then reemergence of the fluid at 2 weeks with complete resolution after the second injection that persisted throughout the study.
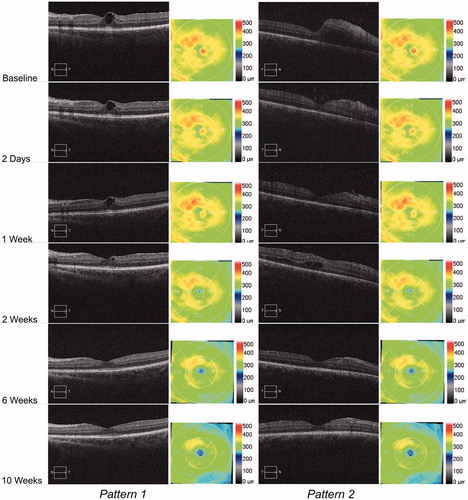
FIGURE 2. (A) Fundus photo of eye number 5 showing significant vitreous haze and inferior vitreous hemorrhage secondary to inferior neo-vessel. (B) Complete resolution of vitreous haze and inferior neo-vessel on last follow-up. (C) Late frame of fluorescein angiography of eye 5 showing diffuse optic disc hyperfluorescence, macular edema with pooling of dye in cystic spaces, diffuse retinal vascular staining, and diffuse capillary leakage in the posterior pole. (D) Complete resolution of leakage on last follow-up.
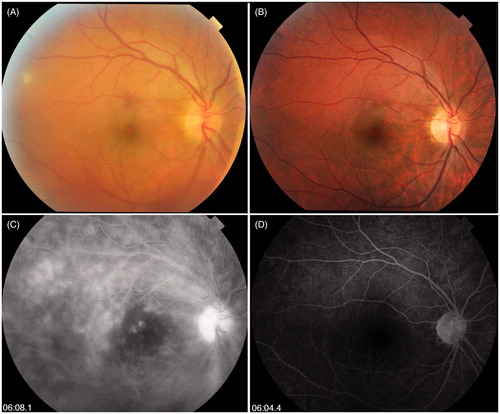
TABLE 5. Median time for resolution of parameters.
The FA score decreased in all eyes compared to baseline and normalized in 2 eyes of 1 patient (, ). The median FA score improved from 14 at baseline to 4 on last visit (p = 0.002) (). Analysis of the individual elements of the FA score showed that the retinal vascular staining (vasculitis) was the first to respond followed by optic disc hyperfluorescence. The difference in the response of the different elements of the FA score is summarized in .
TABLE 6. Difference in the response of various elements of the fluorescein angiography score.
No significant fluctuations in the ERG amplitudes were noted throughout the study, including the eye that failed treatment. No ocular or systemic side effects were encountered during the study. Also, there was no worsening of cataract or change in intraocular pressure.
When the data were stratified to include the worst eye only (7 eyes of 7 patients), similar trends were revealed with logMAR, CRT, and FA score analyses. The difference in the median logMAR and FA score on last visit compared to baseline was significant (p = 0.028 and 0.027, respectively). It trended toward improvement in CRT without reaching significance by 26 weeks (p = 0.116).
Discussion
In this small prospective noncomparative interventional case series, IVA showed a trend for improving intraocular inflammation, cystoid macular edema, and visual acuity in 6 out of 7 enrolled patients. One patient failed treatment but was able to regain baseline vision with no permanent effect. All patients had been treated with systemic corticosteroids and immune suppressive therapy, including antimetabolites, T-cell inhibitors, and even systemic anti-TNFα but were intolerant, uncontrolled, or relapsed prior to recruitment for the study (). On the other hand, 4 of our 7 patients had Behçet uveitis, which might have positively affected our results given the relapsing remitting course of the disease and the favorable outcome of Behçet disease-associated uveitis to treatment with systemic anti-TNFα.Citation19
Intravitreal drug delivery has been used successfully in uveitis in case of dexamethasone implant. Intravitreal dexamethosone was found to improve intraocular inflammation and visual acuity in patients with noninfectious intermediate and posterior uveitis with side effects, including increased intraocular pressure and cataract.Citation20 Intravitreal anti-TNFα injection was evaluated for the treatment of refractory diabetic macular edema.Citation21 Those data suggested that both intravitreal adalimumab and intravitreal infliximab had no effect on refractory diabetic macular edema. Moreover, intravitreal injections of infliximab may lead to serious intraocular inflammation.Citation21 On the other hand, IVA did not lead to retinal damage in animal models at a dose of 0.5 mg in one studyCitation22 and up to 5 mg in another study.Citation23 No information is available on the stability and efficacy of reconstituted or aliquoted adalimumab for multiple use to date. As such, adalimumab was neither reconstituted nor aliquoted for the purpose of this study and the medication was used fresh for all patients.
The response elicited in this small case series differed by the type of the inflammatory parameter assessed, reflecting different sensitivities to blocking TNFα. As such, the response was relatively fast for anterior chamber cells, vitreous haze, macular edema, and vascular staining on fluorescein angiography, requiring a median of 2 injections of intravitreal adalimumab to achieve resolution. On the other hand, the least responsive inflammatory element was capillary leakage on fluorescein angiography, requiring all 7 injections to achieve resolution in only 2 out of 13 eyes. This might reflect on the elements of the inflammation that are more susceptible to TNFα in the uveitis setting and as such are more responsive to TNFα blockade. Similar to the results of Androudi et al.,Citation24 we did not detect toxic effects of intravitreal adalimumab by OCT and ERG and reported no local or systemic side effects associated with the treatment.
Finally, it is worth noting that our protocol involved less frequent local treatment with adalimumab compared to the systemic protocol, which is a subcutaneous injection every 2 weeks. Despite that, our results are favorable for visual acuity, macular edema, and inflammation control and propose a notable alternative for patients who cannot tolerate systemic immunosuppressants or in cases where the inflammation is limited to the eye. However, as in systemic adalimumab, local treatment is not expected to induce sustained remission of disease. Furthermore, given the limitations of our study having a small sample size with no control group and no masked evaluators, no conclusions could be inferred from the above other than highlighting the need for a comparative study. Furthermore, future studies for determining the optimal drug concentration, treatment protocol, the half-life of this medication in the vitreous, and possible long-term toxicity is necessary.
Acknowledgments
This paper was presented at a meeting of the American Uveitis Society, November 2013, New Orleans, Louisiana.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
The authors thank Jamil Missaykeh for patient referral, and Hassan Chahine for ERG conduction and analysis.
References
- Caspi R. Autoimmunity in the immune privileged eye: pathogenic and regulatory T cells. Immunol Res. 2008;42:41–50
- Suttorp-Schulten MS, Rothova A. The possible impact of uveitis in blindness: a literature survey. Br J Ophthalmol. 1996;80:844–848
- Galor A, Jabs DA, Leder HA, et al. Comparison of antimetabolite drugs as corticosteroid-sparing therapy for noninfectious ocular inflammation. Ophthalmology. 2008;115:1826–1832
- Pujari SS, Kempen JH, Newcomb CW, et al. Cyclophosphamide for ocular inflammatory diseases. Ophthalmology. 2010;117:356–365
- Murray PI, Sivaraj RR. Anti-TNF-alpha therapy for uveitis: Behçet and beyond. Eye (Lond). 2005;19:831–833
- Robertson M, Liversidge J, Forrester JV, et al. Neutralizing tumor necrosis factor-alpha activity suppresses activation of infiltrating macrophages in experimental autoimmune uveoretinitis. Invest Ophthalmol Vis Sci. 2003;44:3034–3041
- Santos Lacomba M, Marcos Martin C, Gallardo Galera JM, et al. Aqueous humor and serum tumor necrosis factor-alpha in clinical uveitis. Ophthalmic Res. 2001;33:251–255
- Perez-Guijo V, Santos-Lacomba M, Sanchez-Hernandez M, et al. Tumour necrosis factor-alpha levels in aqueous humour and serum from patients with uveitis: the involvement of HLA-B27. Curr Med Res Opin. 2004;20:155–157
- Sugita S, Takase H, Taguchi C, Mochizuki M. The role of soluble TNF receptors for TNF-alpha in uveitis. Invest Ophthalmol Vis Sci. 2007;48:3246–3252
- Imrie FR, Dick AD. Biologics in the treatment of uveitis. Curr Opin Ophthalmol. 2007;18:481–486
- Lim L, Suhler EB, Smith JR. Biologic therapies for inflammatory eye disease. Clin Experiment Ophthalmol. 2006;34:365–374
- Sobrin L, Kim EC, Christen W, et al. Infliximab therapy for the treatment of refractory ocular inflammatory disease. Arch Ophthalmol. 2007;125:895–900
- Tugal-Tutkun I, Mudun A, Urgancioglu M, et al. Efficacy of infliximab in the treatment of uveitis that is resistant to treatment with the combination of azathioprine, cyclosporine, and corticosteroids in Behçet's disease. Arthritis Rheum. 2005;52:2478–2484
- Dobner BC, Max R, Becker MD, et al. A three-centre experience with adalimumab for the treatment of non-infectious uveitis. Br J Ophthalmol. 2013;97:134–138
- Diaz-Llopis M, Garcia-Delpech S, Salom D, et al. Adalimumab therapy for refractory uveitis: a pilot study. J Ocul Pharmacol Ther. 2008;24:351–361
- Díaz-Llopis M, Salom D, Garcia-de-Vicuña C, et al. Treatment of refractory uveitis with adalimumab: a prospective multicenter study of 131 patients. Ophthalmology. 2012;119:1575–1581
- Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–516
- Tugal-Tutkun I, Herbort CP, Khairallah M. Angiography Scoring for Uveitis Working Group (ASUWOG). Scoring of dual fluorescein and ICG inflammatory angiographic signs for the grading of posterior segment inflammation (dual fluorescein and ICG angiographic scoring system for uveitis). Int Ophthalmol. 2010;30:539–552
- Deuter CM, Kötter I, Wallace GR, et al. Behçet's disease: ocular effects and treatment. Prog Retin Eye Res. 2008;27:111–136
- Lowder C, Belfort R Jr, Lightman S, et al. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol. 2011;129:545–553
- Wu L, Hernandez-Bogantes E, Roca JA, et al. Intravitreal tumor necrosis factor inhibitors in the treatment of refractory diabetic macular edema: a pilot study from the Pan-American Collaborative Retina Study Group. Retina. 2011;31:298–303
- Manzano RP, Peyman GA, Carvounis PE, et al. Ocular toxicity of intravitreous adalimumab (Humira) in the rabbit. Graefes Arch Clin Exp Ophthalmol. 2008;246:907–911
- Tsilimbaris M, Diakonis VF, Naoumidi I, et al. Evaluation of potential retinal toxicity of adalimumab (Humira). Graefes Arch Clin Exp Ophthalmol. 2009;247:1119–1125
- Androudi S, Tsironi E, Kalageropoulos C, et al. Intravitreal adalimumab for refractory uveitis-related macular edema. Ophthalmology. 2010;117:1612–1616

