To the editor,
A number of biochemical and hematological markers have been used to assess systemic inflammation in the clinical setting, particularly traditional inflammatory markers such as C-reactive protein (CRP) levels, erythrocyte sedimentation rate (ESR), white blood cell (WBC) counts, and procalcitonin (PCT) levels [Citation1]. PCT, the precursor of calcitonin, has gained widespread interest as a biomarker of bacterial infection [Citation2, Citation3], as it has good specificity for severe bacterial infections in patients with clinically suspected sepsis [Citation4, Citation5] and can discriminate infections from general inflammation [Citation6, Citation7]. The diagnostic sensitivity of CRP, an acute-phase protein synthesized and released into the peripheral blood by the liver in response to inflammation [Citation8], has been frequently compared with that of PCT. Uzzan et al. reported the global odds ratios for diagnosis of infection complicated by systemic inflammation were higher using PCT than using CRP [Citation9]. However, PCT and CRP were not fully compared with other suggestive inflammation related markers, such as the mean platelet volume (MPV) or the neutrophil to lymphocyte ratio (NLR). Characteristically, MPV and NLR are readily available and cost-effective parameters that can be obtained by automatic hematologic analyzer. MPV, an index representing platelet activation and production rate in the bone marrow [Citation10], has also been discussed as a potential clinical marker in a number of active inflammatory disease groups [Citation11–14]. NLR has proven to be a useful measure of systemic inflammation [Citation15]. Also, numerous cancer survival studies also suggest that it is a significant predictor of overall and disease specific survival in patients [Citation16, Citation17]. This study aimed to seek the diagnostic significance of MPV, NLR, and CRP compared to that of the PCT level in pneumonia patients.
We retrospectively analyzed 154 unduplicated pneumonia patients who were tested for PCT for diagnostic purposes at Korea University Guro Hospital, a tertiary teaching hospital, from January 2009 to September 2013. We also obtained MPV, MPV to platelet count (PC) ratio (MPV/PC), NLR, and CRP for each patient on the same day as the PCT measurement. We classified patients into normal (<0.05 ng/ml) and abnormal PCT groups (≥0.05 ng/ml), according to the level of PCT cut-off based on manufacturer’s recommendations [Citation18]. PCT level was determined by the VIDAS BRAHMS PCT assay system (bioMérieux, Marcy L'Etoile, France), which uses a one-step immunoassay sandwich method with fluorescent detection (enzyme-linked florescent immunoassay [ELFA]), or by Elecsys BRAHMS PCT assay (Roche Diagnostics GmbH, Mannheim, Germany) as read on the Cobas e601 automatic electrochemiluminescence immunoassay analyzer. CRP levels were measured by HiSens hsCRP LTIA (HBI Co., Ltd., Anyang, Korea) as read on the TBA-200FR NEO automated clinical chemistry analyzer (Toshiba Medical Systems Corporation, Tochigi-ken, Japan). MPV, MPV/PC, and NLR were mainly measured on the LH 750 or LH 780 automatic hematology analyzer (Beckman Coulter, Miami, FL). Statistically, each parameter was compared between the two groups using Student’s t-tests. Correlation analysis of the two parameters was performed by using the Pearson correlation test. A p value of less than 0.05 was considered significant. Statistical analyses were performed using IBM SPSS Statistics Version 20 (IBM Corporation, Armonk, NY).
We noticed that the abnormal PCT group showed significantly higher MPV/PC, NLR, and CRP values than the normal PCT patients (). The association between PCT and MPV/PC was statistically significant (r = 0.282, p = 0.004), as was the association between PCT and CRP (r = 0.313, p = 0.001) (). In addition, we identified significant positive associations between CRP and MPV or CRP and MPV/PC ratio or CRP and NLR (). Our analysis has some inherent limitations of retrospective study included pneumonia patients over a long period (January 2009 to September 2013), and does not exclude other conditions, such as diabetes or vascular or hematologic disease, which could influence the MPV or NLR values. Each bacterial or viral culture result of pneumonia patients was not considered in the present study. However, the observation that MPV/PC ratio, NLR, and CRP are elevated in patients with high PCT patients compared with that in patients with normal PCT levels. Furthermore, the positive association between PCT and MPV/PC is a novel finding and mirrors the established positive association between PCT and CRP. Recently, Cho et al. reported that the mean MPV was significantly increased in patients with increased PCT level [Citation19]. However, we identified that MPV was not different between normal PCT (<0.05 ng/ml) pneumonia group and high PCT (≥0.05 ng/ml) pneumonia group. Only MPV/PC ratio, CRP and NLR showed statistical differences in pneumonia patients between normal and abnormal level of PCT. This study thus demonstrates that MPV/PC, rather than MPV, has a clinical utility to support a possible role for activated platelets with considering PC in the diagnosis of systemic inflammation. MPV/PC ratio has already been evaluated for some of clinical applications [Citation20–22], including its use as a new parameter for the prediction of long-term mortality in patients with myocardial infarction [Citation20]. Interestingly, while the MPV/PC ratio shows a significant statistical increase in hepatocellular carcinoma patients versus disease-free controls [Citation21], a low MPV/PC ratio is an independent, unfavorable predictive factor for overall survival of advanced non-small cell lung cancer [Citation22]. A positive correlation of CRP with MPV, MPV/PC, and NLR showed that these platelet indices or NLR might be useful parameters to evaluate inflammation, infection or other related diseases. Especially, MPV/PC value has a significance comparable PCT level in pneumonia patients. In future, further well-designed large scale prospective study would be helpful to evaluate the exact clinical meaning of platelet indices such as MPV, MPV/PC or NLR using as an acute or chronic phase reactant.
Figure 1. Associations between the procalcitonin level and mean platelet volume, mean platelet volume/platelet count ratio, neutrophil to lymphocyte ratio, and C-reactive protein in 102 pneumonia patients (The 52 patients were excluded for lower than 0.05 ng/ml procalcitonin level).
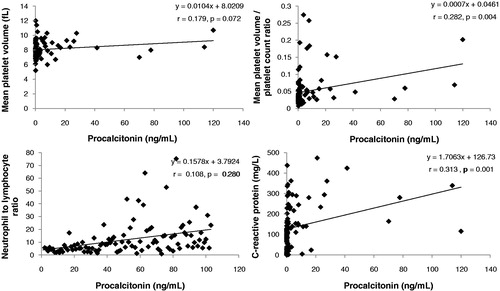
Figure 2. Associations between C-reactive protein level and mean platelet volume, mean platelet volume/platelet count ratio, and neutrophil to lymphocyte ratio in 154 pneumonia patients.
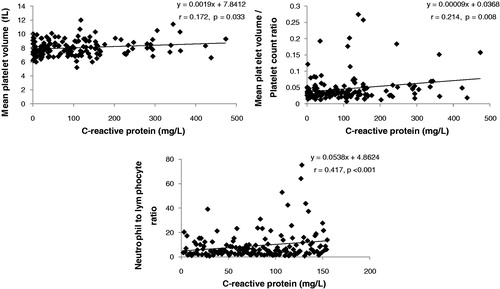
Table I. Comparison of parameters according to the level of procalcitonin in 154 pneumonia patients.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Michail M, Jude E, Liaskos C, Karamagiolis S, Makrilakis K, Dimitroulis D, Michail O, Tentolouris N. The performance of serum inflammatory markers for the diagnosis and follow-up of patients with osteomyelitis. Int J Low Extrem Wounds 2013;12:94–99
- Schuetz P, Christ-Crain M, Muller B. Biomarkers to improve diagnostic and prognostic accuracy in systemic infections. Curr Opin Crit Care 2007;13:578–585
- Schuetz P, Christ-Crain M, Muller B. Procalcitonin and other biomarkers to improve assessment and antibiotic stewardship in infections–Hope for hype? Swiss Med Wkly 2009;139:318–326
- Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet 1993;341:515–518
- Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: A systematic review and meta-analysis. Clin Infect Dis 2004;39:206–217
- Kofoed K, Andersen O, Kronborg G, Tvede M, Petersen J, Eugen-Olsen J, Larsen K. Use of plasma C-reactive protein, procalcitonin, neutrophils, macrophage migration inhibitory factor, soluble urokinase-type plasminogen activator receptor, and soluble triggering receptor expressed on myeloid cells-1 in combination to diagnose infections: A prospective study. Crit Care 2007;11:R38
- Sakr Y, Sponholz C, Tuche F, Brunkhorst F, Reinhart K. The role of procalcitonin in febrile neutropenic patients: Review of the literature. Infection 2008;36:396–407
- Zeng L, He X, Liu J, Wang L, Weng S, Wang Y, Chen S, Yang GY. Differences of circulating inflammatory markers between large- and small vessel disease in patients with acute ischemic stroke. Int J Med Sci 2013;10:1399–1405
- Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: A systematic review and meta-analysis. Crit Care Med 2006;34:1996–2003
- Ekiz F, Yuksel O, Kocak E, Yilmaz B, Altinbas A, Coban S, Yuksel I, Uskudar O, Koklu S. Mean platelet volume as a fibrosis marker in patients with chronic hepatitis B. J Clin Lab Anal 2011;25:162–165
- Canpolat F, Akpinar H, Eskioglu F. Mean platelet volume in psoriasis and psoriatic arthritis. Clin Rheumatol 2010;29:325–328
- Kayahan H, Akarsu M, Ozcan MA, Demir S, Ates H, Unsal B, Akpinar H. Reticulated platelet levels in patients with ulcerative colitis. Int J Colorectal Dis 2007;22:1429–1435
- Milovanovic M, Nilsson E, Jaremo P. Relationships between platelets and inflammatory markers in rheumatoid arthritis. Clin Chim Acta 2004;343:237–240
- Yazici S, Yazici M, Erer B, Erer B, Calik Y, Ozhan H, Ataoglu S. The platelet indices in patients with rheumatoid arthritis: mean platelet volume reflects disease activity. Platelets 2010;21:122–125
- Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med 2012;5:2
- Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg 2009;137:425–428
- Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 2005;91:181–184
- bioMérieux PCT booklet. Available from http://www.biomerieux-diagnostics.com/upload/PCT_BOOKLET_GB.pdf [last accessed 18 Dec 2013]
- Cho SY, Yang JJ, Nam YS, Suh JT, Park TS, Lee HJ. Mean platelet volume in patients with increased procalcitonin level. Platelets 2013;24:246–247
- Azab B, Torbey E, Singh J, Akerman M, Khoueiry G, McGinn JT, Widmann WD, Lafferty J. Mean platelet volume/platelet count ratio as a predictor of long-term mortality after non-ST-elevation myocardial infarction. Platelets 2011;22:557–566
- Cho SY, Yang JJ, You E, Kim BH, Shim J, Lee HJ, Lee WI, Suh JT, Park TS. Mean platelet volume/platelet count ratio in hepatocellular carcinoma. Platelets 2013;24:375–377
- Inagaki N, Kibata K, Tamaki T, Shimizu T, Nomura S. Prognostic impact of the mean platelet volume/platelet count ratio in terms of survival in advanced non-small cell lung cancer. Lung Cancer 2013;in press

