Abstract
Purpose: National and International guidelines recommend cognition and mood assessment for all stroke survivors. However, there is no consensus on preferred screening tool or method of assessment. We aimed to describe clinical practice in cognitive and mood assessment across Scottish stroke services. Method: We used a questionnaire based survey. After local piloting, we distributed the questionnaire using mixed methodologies (online and paper) across all Stroke Managed Clinical Networks in Scotland. We also distributed the questionnaire to specialist societies representing stroke physicians, nurses and allied health professionals and through the UK Stroke Forum delegate pack. Results: We received 174 responses from nurses, physiotherapists, psychologists, occupational therapists and medical staff. Medical staff made up the largest group of respondents (61, 35%). Of the respondents 148 (85%) routinely assess cognition and 119 (72%) mood. A variety of tools were used (cognitive n = 45 tools; mood n = 17); Mini Mental State Examination (n = 103, 59% of respondents) and the Hospital Anxiety and Depression Scale (n = 76, 44%) were the most commonly employed tools. Conclusion: Response rate was modest but included all mainland Scottish regions with active stroke services. Although the majority of responders are assessing cognition and mood there is substantial heterogeneity in measures used and certain commonly used tools are not validated or appropriate for use in stroke. We suggest development of evidence based, standardised assessment protocols.
Screening stroke survivor’s for cognitive and mood issues is recommended but there is little guidance on the preferred assessment strategy
Across Scottish stroke services there is a lack of consensus in assessment and management of cognition and mood post stroke
Sixty-two different cognitive/mood assessment tools were found to be in use across the country
Careful consideration must be given when inspecting assessment tools and use of caution when interpreting results
Implications for Rehabilitation
Introduction
Cognitive and mood problems are common in stroke survivors. Cognitive deficits occur in 30–44% [Citation1] and mood disorders affect 33% [Citation2]. Disorders in these areas have a negative impact across recovery [Citation3–8]. Stroke survivors with cognitive or mood deficits may have better outcomes if diagnosis is made at an early stage and appropriate management started promptly [Citation3,Citation4].
Assessment of cognition and mood is recommended in national guidelines [Citation9], although no direction is offered as to the preferred strategy. Many cognitive screening tools are described, with no consensus on preferred tool for stroke survivor assessment or the optimal method of application. Recent analysis of cognitive and mood assessment in stroke research has suggested substantial heterogeneity in assessment tool choice [Citation10]. Screening and assessment tools that are validated and popular in non-stroke settings may not be appropriate in stroke survivors, who are more likely to have language, physical and cognitive impairments or to be medically unwell in the acute phase [Citation5,Citation11,Citation12].
We aimed to describe usual clinical practice in cognitive and mood assessments across various Scottish stroke care settings.
Method
Piloting
Questionnaire design and piloting was based on published guidance [Citation13–15] and our previous work on cognitive/mood assessment in stroke [Citation16]. We developed the questionnaire to assess key themes: Do practitioners assess mood/cognition? When and how are these assessments performed? How do these assessments inform management? A particularly challenging scenario is assessment of patients with communication impairments and we added a specific question on this.
We performed pilot work in two sites (Glasgow Western Infirmary and Glasgow Royal Infirmary) using a two-stage method. A draft template was circulated to representatives from stroke medicine; nursing and clinical psychology and discussed with individuals (in a focus group setting and through written comments collated by the authors). Content was revised using a modified Delphi process. The revised questionnaire was distributed to a wider group and allowed free-text comments on phrasing and formatting. Comments were collated and decisions on final content were made based on authors’ consensus.
Distribution
Our final questionnaire was a one page (A4) paper document with categorical and qualitative responses. We hosted the questionnaire on an open-access web-site (http://www.surveymonkey.com/s/N7QXYW9). Responses were anonymous but we requested respondents’ discipline and principle work place.
We used mixed methodologies of distribution to ensure comprehensive coverage. Our target group was all staff involved in direct stroke patient management across acute, rehabilitation and outpatient care. We contacted all Scottish, Stroke Managed Clinical Network (MCN) co-coordinators (n = 12) to distribute the questionnaire across their network. We emailed specialist groups (Scottish Stroke Nurses Forum, Scottish Stroke Neuropsychologists, British Geriatric Society, Scotland, British Association Stroke Physicians, Stroke Allied Health Professionals and Association of Chartered Physiotherapists Interested in Neurology) and distributed paper copies through the UK Stroke Forum delegate pack. Reminder emails and letters were sent round MCN co-coordinators who did not respond after 1 month. We checked responses against a list of hospitals providing stroke care using Scottish stroke care audit data (http://www.strokeaudit.scot.nhs.uk/).
Analysis
For categorical data, we described absolute and percentage values, comparing responses across groups using Chi-square analysis or ANOVA as appropriate (SPSS statistics 19, IBM). Qualitative data were grouped into shared themes by hand coding the free text responses.
Our study had the necessary ethical and data governance approvals from the manager and scientific officer for the West of Scotland Research Ethics Committee. This work was supported by Chest, Heart and Stroke Scotland.
Results
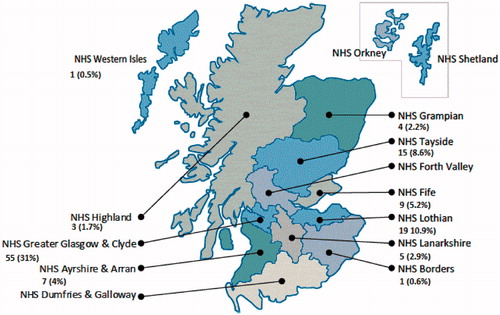
We received 174 responses, this comprised 10/14 (71%) Scottish Health Boards. Respondents represented all mainland Scottish health boards (); Absolute number of returns was highest from Greater Glasgow and Clyde Health Board (55, 32% of all respondents). Respondents comprised medical staff (61, 35%), occupational therapists (27, 16%), other health professionals (27, 16%), nurses (23, 13%), psychologists (13, 7%), physiotherapists (12, 7%) and speech therapists (11, 6%). Of respondents more routinely assessed cognition (n = 148, 85%) than mood (n = 119, 72%, p < 0.001). Proportions of respondents performing cognitive/mood assessment were collated ( and ). Respondents reporting routine assessment of cognition varied by health board, there was no geographical difference in number of respondents reporting cognitive assessment (p = 0.879) but there was for mood assessment (p < 0.001). Glasgow and Greater Clyde Health Board had the highest number of respondents assessing mood (n = 36, 21%).
Table 1. Cognitive/mood assessment modalities used across various clinical settings.
Table 2. Respondents reporting cognitive and mood assessment described by professional group.
A variety of tools were used for stroke survivor assessments (cognitive n = 45 tools; mood n = 17) ( and ). Folstein’s Mini Mental State Examination (MMSE) [Citation17] (n = 103, 59% of respondents) and the Hospital Anxiety and Depression Scale (HADS) [Citation18] (n = 76, 44%) were the most commonly used. There was no difference in use of these measures across health boards (MMSE p = 0.078, HADS p = 0.762) or professions (MMSE p = 0.535, HADS p = 0.953; ). Informal and bespoke methods were also prevalent, “observation” (n = 22, 13%) and “informal questioning” (n = 25, 14%).
Table 3. Cognitive assessment.
Table 4. Mood assessment.
From this sample, assessments were more commonly performed in hospital settings; cognition was mostly assessed during first/acute admission (n = 116, 67% of respondents, p < 0.001) while mood was more commonly assessed in rehabilitation settings (n = 100, 58%, p < 0.001). There was heterogeneity in management strategies for suspected cognitive/mood deficits (n = 14 strategies described). For patients with possible cognitive/mood problems the most common management strategy was onward specialist referral (cognition n = 62, 36%; mood n = 71, 41%). If stroke survivors had a communication problem, the commonest approach was to seek advice from other specialties and have joint assessment and rehabilitation sessions (n = 60, 34%). For mood, adapting the test to the patient (n = 44, 25%) was the preferred approach.
Discussion
We have demonstrated substantial heterogeneity in assessment and management of mood/cognition in stroke survivors. Use of 62 different assessment tools in a geographically small area clearly has implications for audit across services; research and service planning. Although the majority of respondents were assessing cognition and mood, not all were performing this routinely or across all settings. As with any questionnaire, we recognize that respondents are more likely to have an interest in cognition/mood and may not be representative of all healthcare professionals. We suspect that cognitive/mood assessment across all stroke services may be lower than suggested in this survey.
The use of non-validated, bespoke or informal assessments is a concern. Certain commonly used cognitive measures, although validated in other settings, may not be appropriate for stroke survivors. Folstien’s MMSE does not perform consistently well in the stroke [Citation19–21] and ignores executive functioning, a common deficit in stroke populations; Hodkinson’s Abbreviated Mental Test has not been validated in stroke and the properties of Addenbrooke’s Cognitive Examination in stroke survivors is sensitive to timing of assessment [Citation11,Citation22]. For mood measures, there is a lack of research in the acute stroke setting [Citation23] and we have no validated established norms for most tests in stroke populations [Citation21,Citation24]. The Hospital Anxiety and Depression Scale has been validated in stroke [Citation25–27] but not the acute setting and the Geriatric Depression Scale has not been validated within stroke populations. International guidance documents for stroke cognitive and mood assessment are available [Citation28]. The tools recommended in these texts (i.e. Montreal Cognitive Assessment) were not commonly used in our sample.
As well as heterogeneity in assessment tools used, we have also demonstrated heterogeneity in application and intervention. The many different approaches reported for a commonly encountered, specific clinical scenario (the stroke survivor with aphasia) perhaps suggests the need for cognitive and mood assessment strategies specifically tailored to stroke survivors with language problems [Citation29].
The strengths of our survey were the clear research questions and study design based on literature recommendations and robust piloting. Our multi-modal questionnaire distribution will have ensured that most Scottish stroke staff had the opportunity to reply. The principle limitation was the modest response rate from certain regions. However, we achieved responses from most health boards and so we hope we have captured a reasonable snapshot of current practice which may also give insight to usual practice in stroke units across the UK. We followed best practice in achieving maximal response rate [Citation13,Citation16], but did not have the resource to offer financial incentives.
Despite this modest response, our survey gives the first National descriptions of usual practice within Scotland. We propose that evidence based, consensus guidance is offered on the optimal cognitive and mood assessment strategies. Projects such as the Cochrane Collaboration’s diagnostic test accuracy work should inform this guidance or at least highlight where original research is still needed.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgements
We are grateful to all who completed the survey.
References
- Patel M, Coshall C, Rudd AG, Wolfe CD. Natural history of cognitive impairment after stroke and factors associated with its recovery. Clin Rehabil 2003;17:158–66
- Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke 2005;36:1330–40
- Sinyor D, Amato P, Kaloupek DG, et al. Post-stroke depression: relationships to functional impairment, coping strategies, and rehabilitation outcome. Stroke 1986;17:1102–7
- Zinn S, Dudley TK, Bosworth HB, et al. The effect of poststroke cognitive impairment on rehabilitation process and functional outcome. Arch Phys Med Rehabil 2004;85:1084–90
- Nys GM, van Zandvoort MJ, de Kort PL, et al. The prognostic value of domain-specific cognitive abilities in acute first-ever stroke. Neurology 2005;64:821–7
- Larson EB, Kirschner K, Bode RK, et al. Brief cognitive assessment and prediction of functional outcome in stroke. Top Stroke Rehabil 2003;9:10–21
- Galski T, Bruno RL, Zorowitz R, Walker J. Predicting length of stay, functional outcome, and aftercare in the rehabilitation of stroke patients. The dominant role of higher-order cognition. Stroke 1993;24:1794–800
- Jongbloed L. Prediction of function after stroke: a critical review. Stroke 1986;17:765–76
- Scottish Intercollegiate Guidelines Network (SIGN). Guideline 118 (with updates). Management of patients with stroke. Rehabilitation, prevention and management of complications and discharge planning. SIGN and Healthcare Improvement Scotland; 2011
- Lees R, Fearon P, Harrison JK, et al. Cognitive and mood assessment in stroke research: focused review of contemporary studies. Stroke 2012;43:1678–80
- Morris K, Hacker V, Lincoln NB. The validity of the Addenbrooke's Cognitive Examination-Revised (ACE-R) in acute stroke. Disabil Rehabil 2012;34:189–95
- Hobson JP, Leeds L, Meara RJ. The feasibility of cognitive screening of patients with ischaemic stroke using the preliminary neuropsychological battery. Psychol Health 2003;18:655–65
- Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ 2008;179:245–52
- Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004;6:e34 doi: 10.2196/jmir.6.3.e34
- Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Health Care 2003;15:261–6
- Lees R, Fearon P, Harrison JK, et al. Cognitive and mood assessment in stroke research: focused review of contemporary studies. Stroke 2012;43:1678--80
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70
- Agrell B, Dehlin O. Mini mental state examination in geriatric stroke patients. Validity, differences between subgroups of patients, and relationships to somatic and mental variables. Aging (Milano) 2000;12:439–44
- Nys GM, van Zandvoort MJ, de Kort PL, et al. Restrictions of the Mini-Mental State Examination in acute stroke. Arch Clin Neuropsychol 2005;20:623–9
- Blake H, McKinney M, Treece K, et al. An evaluation of screening measures for cognitive impairment after stroke. Age Ageing 2002;31:451–6
- Pendlebury ST, Mariz J, Bull L, et al. MoCA, ACE-R, and MMSE versus the national institute of neurological disorders and stroke-canadian stroke network vascular cognitive impairment harmonization standards neuropsychological battery after TIA and stroke. Stroke 2012;43:464–9
- Townend B, Whyte S, Desborough T, et al. Longitudinal prevalence and determinants of early mood disorder post-stroke. J Clin Neurosc 2007;14:429--34
- Agrell B, Dehlin O. Comparison of six depression rating scales in geriatric stroke patients. Stroke 1989;20:1190–4
- Johnson G, Burvill PW, Anderson CS, et al. Screening instruments for depression and anxiety following stroke: experience in the Perth community stroke study. Acta Psychiatr Scand 1995;91:252–7
- Sagen U, Vik TG, Moum T, et al. Screening for anxiety and depression after stroke: comparison of the hospital anxiety and depression scale and the Montgomery and Asberg depression rating scale. J Psychosom Res 2009;67:325–32
- Tang WK, Ungvari GS, Chiu HF, et al. Screening post-stroke depression in Chinese older adults using the hospital anxiety and depression scale. Aging Ment Health 2004;8:397–9
- Hachinski V, Iadecola C, Petersen RC, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke 2006;37:2220–41
- Thomas SA, Walker MF, Macniven JA, et al. Communication and Low Mood (CALM): a randomized controlled trial of behavioural therapy for stroke patients with aphasia. Clin Rehab 2013;27:398--408