Abstract
Purpose: Information regarding the nature, availability and distribution of rehabilitation services for children with disabilities across developing countries is scarce, and data that do exist are of variable quality. If planning and development are to progress, information about service provision is vital. The aim was to establish the scope and nature of rehabilitation support available to children with disabilities (0–15 years) and their families in rural Kenya. Method: A comprehensive sample comprising service provision in the health and special education sectors was established. Non-governmental and community-based organisations were also included. A survey of rehabilitation services was conducted through examination of service-related documentation and key informant interviews with the heads of services. Results: Rehabilitation comprised hospital-based occupational therapy, physiotherapy and orthopaedic technology; and seven special education establishments plus an education assessment resource centre. There was one non-government organisation and one community-based organisation relevant to children with disabilities. Activities focused on assessment, diagnosis and raising community awareness. Provision was challenged by inadequate staffing, resources and transport. Government funding was supplemented variously by donations and self-sufficiency initiatives. Rehabilitation approaches appeared to be informed by professional background of practitioner, rather than the needs of child. Service documentation revealed use of inconsistent recording methods. Conclusions: The data highlight the challenges of rehabilitation, demanding greater investment in personnel and their training, more material resources, improved access to the community and better recording mechanisms.
There needs to be greater investment in rehabilitation provision in developing countries.
Consideration of community-based initiatives is required to support better access for all.
In order to argue the case for improved resources, better skills and mechanisms for recording, monitoring and evaluating practice are needed.
Implications for Rehabilitation
Introduction
The World Health Organisation’s (WHO) survey of 29 African countries reported wide variation in rehabilitation services across the continent, with poor coordination of delivery, limited access to such services at community level and a continuing need for development work [Citation1]. More recently, reports of health-based rehabilitation services have revealed serious limitations in coverage and capacity [Citation2–5]. When rehabilitation services do exist, they tend to be clustered around urban-based institutions [Citation5,Citation6] and are inadequately scoped to meet the needs of all service users [Citation2]. Non-governmental organisations have arisen, usually to cater for specific areas of need that have been neglected [Citation7]. For example, the Association for Physically Disabled Kenya, established in 1958, offers a range of support including mobile clinic facilities and assistive technology to aid mobility [Citation8]. However, such organisations are experiencing financial pressures and resource limitations that also affect government-funded services [Citation7]. One of the problems affecting the information about rehabilitation support is the lack of technical capacity to collect and record service-related data [Citation9,Citation10].
Nevertheless, it has been established that rehabilitation services in low-income countries compare unfavourably with those in high-income countries [Citation7]. Restricted rehabilitation services have been attributed to a dearth of appropriately qualified personnel [Citation11–14] and an absence of professional organisations [Citation2]. Reporting on provision in Ghana, Tinney et al. [Citation4] stated that there were no occupational therapists or physiatrists, very few speech and language therapists, prosthetists, orthotists and physical therapists, because of a lack of funding and limited government support. There have been reported discrepancies in rehabilitation personnel employed in low-income countries compared to middle-income ones. For example, 0.4–0.6 psychologists per 100 000 people contrasted with 1.8 in upper-middle-income countries and 14 in high-income countries [Citation15]. Workforce deficiencies have been revealed by the World Federation of Occupational Therapists, which reported that Kenya has 0.2 occupational therapists per 10 000 of the people, which makes Kenya below the international average of 2 per 10 000 and that of 5 in the UK [Citation16].
The reduced presence or even the absence of certain disciplines makes rehabilitation a complex endeavour, which affects multi-disciplinary care, onward referral and follow-up. Personnel working under such conditions frequently require knowledge and practitioner skills that extend beyond the traditional focus of the single, professional discipline [Citation7]. Educational programmes for the rehabilitation professions are not present in all developing countries, and when they do exist, vary in terms of curricular content and professional competencies targeted [Citation17,Citation18]. This may result in professionals who are ill equipped to deal with both the realities of service user needs and the contexts of rehabilitation provision [Citation19]. The WHO [Citation7] suggests that by training a workforce of mid-level workers who carry out multipurpose rehabilitation practice, some of the difficulties associated with “absent” professions might be circumvented. Another level of training is also recommended by the WHO – that of community-based workers, which has the potential to cross professional boundaries and include social and environmental activities, whilst also improving geographical access [Citation3].
Working conditions and opportunities for development help to maintain people in their professional roles [Citation4,Citation19]. A desire for improvement in these areas has prompted professional migration from low-income to higher income countries [Citation20]. Working conditions implicates not only funds, but also equipment. Tinney et al. [Citation4] identified outdated facilities and machinery in the five fabrication centres in Ghana, making a range of musculoskeletal aids, such as lumbar corsets, metal orthotics, custom shoes, cervical collars, simple prosthetics, wooden crutches and back boards. In their scoping review of rehabilitation in Tanzania, Njelesani et al. [Citation5] reported gaps in available resources. Special education facilities are not without problems with report of insufficient number of classrooms, inadequate learning support materials and poor physical condition of buildings [Citation21–23].
Utilisation of services is affected not only by resource availability, but also by factors that interplay with user demand. For example, costs of access, lack of information and cultural barriers may present as barriers to utilisation [Citation24]. The financial burden is felt more keenly amongst families from lower income groups [Citation7,Citation25]. Inadequate social support systems and the extra expenses associated with meeting the needs of the child with a disability have been acknowledged factors in caregiver stress, which in turn may affect care-seeking behaviour [Citation26]. The social stigma of caring for such a child may add to the caregiver’s load, particularly when the child’s condition is viewed as the result of curses or evil spirits [Citation27–30]. Furthermore, the added cost brought about by distance from the homestead to rehabilitation facilities may indirectly reduce consumer demand [Citation31], as has been documented in utilisation of services for epilepsy [Citation32]. Moïsi et al. [Citation33] suggested that the lower uptake of services by low-income families residing in rural areas of Kenya, Burkina Faso, Congo and Tanzania was due to poor public transportation. Ensor and Cooper [Citation24] commented that attempts to improve the status quo frequently focus on staff skills, treatment protocols, availability of supplies and health facilities, i.e. the supply end of the rehabilitation equation; but do not address many of the barriers affecting service utilisation, i.e. the demand end, such as transport availability and cost.
The current study aimed to gather information about rehabilitation support for children with disabilities in Kilifi District, a rural part of Kenya. The most recent WHO definition of “rehabilitation” is employed, which refers to “a set of measures that assist individuals who experience or are likely to experience disability, to achieve and maintain optimal functioning in interactions with their environments” [Citation7, p. 96]. There was one overarching research question: What is the rehabilitation service situation in Kilifi District for children with disabilities and their families? A subsidiary question was: How does rehabilitation provision meet the needs of such children?
Methods
Design and setting
A descriptive and record-based survey of rehabilitation provision and utilisation was carried out as the initial stage of a situation analysis. Health and educational services within the Kilifi Health Demographic and Surveillance System [KHDSS] were included, which has a population of 260 000, with 48 182 living in Kilifi Township [Citation34]. It is the second poorest district in Kenya, with most of the rural population living as subsistence farmers. Based on the WHO estimate of a prevalence of disability as 15%, 39 000 people in KHDSS area are estimated as having a disability [Citation34]. This is an area where previous studies on malaria, neurological impairment and participatory rural appraisal have been conducted [Citation35–38]. For example, the prevalence of severe and moderate disability in children of 6–9-years-old was reported to be 6.1% [Citation38]. Special educational services are located mainly in Bahari Division, just north of Kikambala where Kilifi District Hospital is located.
Sample
A comprehensive sample of rehabilitation services for children 0–15-years-old with disabilities across the health and special educational sectors was established, starting with those services already known to the research unit and identifying additional support through the use of snowballing techniques. This yielded three health-based rehabilitation services at Kilifi District hospital, two special schools and five units attached to mainstream provision. A further 28 community-based organisations were identified and the local branch of one non-government organisation (NGO). All services agreed to participate in the survey.
Ethics
Study approval was given by the National Ethical Review Committee of Kenya and at the University of East Anglia. Informed consent was obtained from both service providers and users listed on current caseloads.
Data collection and analysis
Data collection was conducted during the period 2007–2008. Based on work by the United Nations (UN) Statistics Division and the conceptualisation of disability according to the International Classification of Functioning and Disability (WHO), two lists of variables were generated for the survey ().
Table 1. Summary of variables used in survey.
In order to establish professional capacities of rehabilitation, the “service provider” list was used as a guide for structured interviews with staff employed in the formal aspects of provision, i.e. health-based rehabilitation (n = 10) special education (n = 40). This was carried out by the field worker in a pre-arranged visit to each service, when contact was made with the service head and the staff. Responses were recorded on paper and entered into a prepared Excel spreadsheet. Detail on continuing professional development (CPD), such as length of course, curricular content and learning outcomes was not available. The data were summarised according to host sector, i.e. health or education. Ratios of establishment to CPD events were calculated.
The “service user” list of variables guided the data collection about the children, 0–15 years, to assess how rehabilitation provision meets the needs of children. The head of each health department and school/unit was asked to provide records, either electronically or in hard copy, of all children (0–15 years) currently in receipt of the service. This caseload information was obtained from the hospital-based departments and student registers in the special educational establishments. A flexible approach to data collection was taken to cater for variability in the format and quality of paper records held by each service. Information was entered into a prepared Excel spreadsheet. Any empty fields, ambiguous or incomplete data were identified by the research team and a follow-up visit was used to solicit information verbally from the informants, i.e. the service heads. For example, documentary information on individual cases was frequently sparse, containing little more than name, date of birth and presenting condition. Follow-up visits involved asking the service head or other members of staff according to availability, to review individual cases, to identify the functional difficulties from a given range and to articulate the recommended intervention for each case. Information was recorded in note form and entered into a spread sheet. In order to make sense of the intervention data, analysis was carried out by members of the research team. The interventions were grouped according to homogeneity, until consensus regarding the final nominal categories was reached. In order to determine the user experience of support services, in-depth interviews were conducted with a sample of caregivers for the children. These results are reported in a separate paper in preparation (Hartley et al.).
In order to determine the aims and objectives, perceived challenges and sustainability of each service, semi-structured interviews were conducted with head of each service as key informant (health-based rehabilitation = 3; special education = 7; NGO = 1). Using a topic guide, participants were asked about the type of services on offer; the main aims and objectives; the perceived outputs; participation at individual and community level; and sustainability of service. The interviews were digitally recorded and transcribed. Content analysis was applied to the data [Citation39]. First, the text was read and re-read for familiarisation, with any impressions recorded in note form. Then the data were organised by the topics covered in the interview schedule. Any consistencies and differences were identified across the informant accounts. Themes were identified and connections within and between themes were explicated, before finally interpreting the data. Service information was organised according to health or education sectors and displayed in a series of summary tables.
Results
Service situation
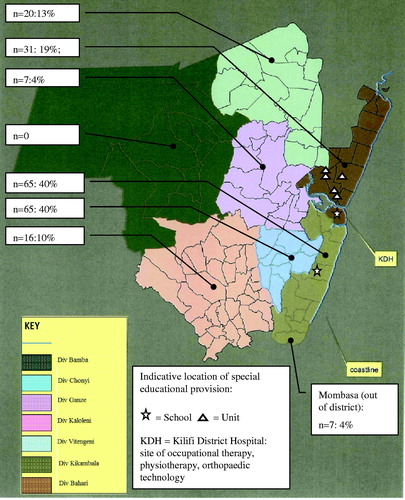
provides a map of Kilifi District showing the various residential divisions. The location of rehabilitation facilities in the health and special education sectors are indicated. Health-based rehabilitation services comprising occupational therapy, physiotherapy and orthopaedic technology were situated in Kilifi District Hospital in Kilifi Town, the south of Bahari and just to the north of Kikambala. There was no speech and language therapy. The special education establishments, comprising two schools and five units attached to mainstream provision were located mainly in Bahari Division with one facility in Kikambala. The number of service users living in each division who were in receipt of health rehabilitation at the time of survey is also shown as a percentage of caseload (n = 162). Similar information regarding where pupils lived was not available from the education sector.
Figure 1. Map of Kilifi District showing the location of rehabilitation facilities and residential location of service users attending rehabilitation at Kilifi District Hospital as a percentage of total caseload (n = 162).
shows that the highest level of professional training attained by the majority of health-employed personnel was a diploma in the chosen profession, e.g. Occupational Therapy or Physiotherapy. Whilst the majority of educational staff had diplomas in special education, there were a few with certificates (n = 3) and degrees (n = 5). The staff whose professional training was either non-existent (n = 3) or else limited to short course attendance (n = 3) were special education assistants. Similar data were not available from the Association for Physically Disabled in Kenya (APDK). The number of CPD events reported by health-based staff (n = 37) represented an approximate ratio of 4 courses per member of staff over a 10-year period. Examples of CPD were: skills-based courses such as counselling, tricycle design, cobbling and carpentry; knowledge-based events focusing on TB, HIV/Aids, malaria and leprosy. The majority of the courses appeared to be local, certificated events with the exception of 1 physiotherapist who had studied for a higher diploma in counselling. In the special education sector, 89 CPD courses were identified by the staff collectively, representing a ratio of two courses per member of staff over ten years. However, 11 of the 89 courses accounted for teachers currently studying for a degree. The remainder of courses (n = 78) included skills-based training in various assessment methods, hearing aid repair and maintenance, computer packages, Kenyan sign language, low vision training and Braille; and knowledge-based events focusing on HIV/Aids.
Table 2. Professional training and experience of staff.
Occupational therapy focused mainly on provision for the under-5-year-olds, with a small component of adult work. Service activity focused on physical dysfunction; splinting or corrective therapy for birth defects; counselling; and what was referred to as “speech therapy” in the absence of speech and language therapists. Physiotherapy had a greater emphasis on adult work with a small caseload of children with gait or mobility problems. Orthopaedic Technology provided corrective appliances for children and supportive appliances for adults.
The first special school (School A) catered for children with hearing impairment. In addition to usual curricular activities, such as literacy and numeracy, it also offered “speech rehabilitation, hearing aid maintenance and ear mould production”. The second school (B) provided for children with intellectual disability, with a focus on “daily living and vocational skills”. Two of the units served children with intellectual disability (Units A and D), with an emphasis on training students “to get along with their peers and other members of the society through social learning” and providing “a course of study with a suitable foundation”. The other units catered for children with cerebral palsy (Unit B), focusing on “daily living activities in order to depend on themselves in the future”; hearing impairment (Unit C), ensuring that “children within and around the centre gain access to the nearest service to their home”; and visual impairment (Unit E), which focused on “minimising the learning handicaps” and helping learners to be “self-independent”. There was also an Education Assessment Resource Centre (EARC) responsible for assessing children with special needs in the district, with a post-assessment focus on referral for “educational and medical intervention”.
In addition, there was one NGO: the Association for Physically Disabled Kenya (APDK), which worked closely with the Ministry for Health, but also had contact with special education [Citation8]. The work of the local branch was not confined to Kilifi District, but covered other areas in the Coast Province as far as Malindi, Taita Taveta, Kwale, Msambweni and Kinango. It focused mainly on assessment and onward referral, putting people with physical disabilities in touch with the most appropriate services and resources, e.g. orthopaedic surgery, assistive technology (callipers, wheelchairs) and the EARC for education. There were also 28 community-based organisations, with all but one focused on adults with disabilities. The one organisation making specific mention of children with disabilities was concerned with raising funds for the development of a special school. Information about the numbers of people helped and the type of assistance provided was not available.
Three major themes emerged from the key informant interviews. The first was service aims and objectives, which were a mixture of activities undertaken and service aspirations. The second was challenges to service provision, which acted as barriers to certain aspects of provision and included resource limitations, inadequate transport and opposing cultural beliefs. The third was sustainability of service, which was used frequently by the informants to refer to the financial support and money-raising initiatives on which the service was dependent. provide a summary of themes that emerged in relation to the topics framed in the interview. Service-based examples have been taken from the transcriptions and aligned to either the health or special education sector.
Table 3. Service aims and objectives.
Table 4. Challenges to service provision.
Table 5. Sustainability of service.
Service objectives included a range of activities, as shown in . Assessment was a recognised function of both health and special education services, although there was particular mention of early diagnosis by the occupational therapy service. Skills acquisition, self-help and independence were considered key outputs of the services. The provision of assistive technology was used to support motor development and functioning. The APDK appeared to have a particular remit for providing appliances such as reconditioned wheelchairs and crutches via their workshop at Bombolulu, Mombasa – 60 km from the area. Participation as a concept seemed to mean discharge from hospital services with school placement to follow, and attendance of mainstream classes in the educational sector. Psychological adaptation was a shared concern of both sectors. Counselling carers towards acceptance of the child’s disability was one aspect; informing and educating the community was another.
As shown in , the first areas of challenge related to staffing and resources, both of which were perceived to be inadequate. Low staffing levels were attributed with restricting outreach, community-based work by the occupational therapists. The volume of people accessing orthopaedic technology as a result of increased awareness, placed stress on already limited resources. Transport was seen as pivotal to service access and provision. An inadequate and expensive transport service restricted not only domiciliary practice, but also attendance of rehabilitation facilities by those in need of them. This was compounded by service user poverty. Personal finance was an identified factor in rehabilitation outcomes, because attendance of the hospital department could not be sustained. In the schools and units, the socio-economic vulnerability of families was recognised and placed extra responsibilities on the educational establishment to provide food and clothes, as well as learning materials. Community-held beliefs and the negative attitudes towards disability were seen as problematic by both sectors, which variously affected the services. For example, a school’s benefactor was cited as supporting boys in education, at the expense of girls. The move towards inclusive education was deemed to be thwarted by the negative, segregationist attitudes evinced by the community. Cultural superstitions were also identified as particular challenges to addressing the needs of children with disabilities.
As shown in , service sustainability relied on a combination of government funding, private donations and financial contributions from service users. Self-sufficiency projects were an additional source of income for the educational establishments, e.g. keeping domestic livestock and selling produce. The APDK worked with people with physical disabilities and supported the work of the EARC in assessing children, facilitating appropriate school placement, and providing financial support and reconditioned equipment.
Meeting the needs of children
This aspect of the survey focused on the formal aspects of the health and special education sectors. The total number of children (0–15 years) appearing on service registers was: 162 for the health sector; 276 for special education. As shown in , health-rehabilitation users were most frequently resident in the coastal divisions of Kikambala, representing around 40% of those individuals in current receipt of services, and secondly, Bahari (19%). The divisions of Ganze, Kaloleni, Chonyi and Vitengeni are inland areas, which accounted for 4–10% of registered service users, whilst the division of Bamba in the western part of Kilifi District and furthest away from the health rehabilitation base, was unrepresented. The small number of service users from Mombasa represented out of district contacts (4%). Similar information was not available from the special education facilities.
summarises the prevalence of daily living difficulties attributed to registered cases by the key informant for the service. No individual appeared on more than one service register. Mobility and self care problems appeared to be more prevalent in the health sector, e.g. sitting, walking, standing, dressing and washing, and functional limitations associated with language development were more commonly identified in special education, e.g. understanding, reading. Cases of sensory impairment were restricted to education. Difficulty with ‘speaking’ was identified minimally in special education and not at all in health.
Table 6. Number (%) of service users with difficulties in daily activities (Health: n = 162; Special education: n = 276).
summarises the intervention approaches assigned to cases on service registers by the key informant for each service. Fifty different labels for intervention approaches were generated initially, ranging from the general, e.g. home visit, rehabilitation exercise, equipment, to the specific, e.g. riding static bike, bilateral hip joint callipers, Braille. The items were sorted into seven categories (A–G) based on similarities in practice, as informed by service provider accounts and observational knowledge of the research team (). Only “rehabilitation exercise” under “Category C. Exercises” was mentioned by both sectors. The health sector listed therapy approaches with a physical orientation (Categories A, B and C). Special education focused on support for learning (Categories D, E and F). The final category – G. Social Support, comprised just one item: home visits, which was only referenced by the special education sector. Included in Category B. were “massage” and “sensory stimulation”, which were approaches used in Occupational Therapy to stimulate speech development, e.g. applying ice blocks to the oro-musculature. Approaches under F were specifically labelled as “speech work” or Kenyan Sign Language.
Table 7. Intervention approaches identified by service providers for children on caseload/school register.
Discussion
Paucity of documentation at case and service levels revealed the lack of technical capacity to record information, not only about the scale and activity of services but also the workforce delivering rehabilitation.
Service coverage
Service coverage demonstrates a considerable gap between those people in receipt of a service and the estimated number of people likely to require some form of rehabilitation. The KDHSS area has a reported population of 260 000 of which 160 335 are aged 15 years and below [Citation34]. Based on a 6.1% prevalence of moderate to severe disability amongst children [Citation38], it can be expected that 9620 children will live with a disability in the KDHSS area, and therefore require some form of rehabilitation service. However, the combined figure of children utilising health (n = 162) and special education facilities (n = 276) in the current survey is 438. This represents just 0.3% of the moderate to severe disabled children the KDHSS area. Thus, it can be seen that rehabilitation coverage falls way below the predicted level of need, i.e. 6.1%. It is possible that other rehabilitation facilities in neighbouring districts were accessed by residents living on the outskirts of Kilifi District, e.g. 52 km north-east of Kilifi is Malindi and 60 km south is Mombasa. Nevertheless, the gap between actual coverage and projected need would seem to be consistent with the findings from past research [Citation2–5].
Community access
The urban location of facilities in Kilifi echoes report from other low-economic countries [Citation5,Citation6]. In a rural community with a poor transport system where subsistence farming is the major source of income, it is expected that physical access to services may have been problematic for many, resonating findings from previous research [Citation33]. This may account for the fact that people residing in divisions closest to facilities made up the majority of caseload entries for hospital-based services. Referred to as distance decay, this suggests that distance from service centre is critical to accessing support.
In addition to distance from services and transport problems, social stigma and superstitious beliefs associated with disability may have further modulated the degree to which families displayed care-seeking behaviours. The role of information and education as a counterbalance to such negative responses cannot be ignored [Citation24]. The urban location of services could have restricted the spread of information [Citation12]. Outreach activities might have been one way of circumventing not only perceived lack of knowledge and understanding in the community, but also physical access problems experienced by the families. However, unsatisfactory staffing levels and inadequate resources on the supply side, and lack of funds for travel and educational/therapy fees on the user side, were recognised factors in the service situation. Delivery of service objectives was further constrained by poor quality materials and malfunctioning equipment in both sectors, which echoes reports from Ghana [Citation4]; Botswana [Citation21] and Uganda [Citation22]. Whilst self-sufficiency initiatives appeared to be essential to service sustainability, they represented another possible source of workload pressure on employed staff. The support offered by the one NGO – APDK, was recognised by the formal aspects of service provision for its work with physically disabled individuals; however, the limited financial and other resources confirms WHO’s report [Citation7]. Thus, the informant accounts of factors affecting the scale and nature of service activities are consistent with deficiencies reported for low-income countries [Citation7,Citation15,Citation16].
Meeting the needs of children
The extent to which caseload activity was determined by the professional background of practitioners rather than the presenting needs of children and their families is a matter for concern. The major focus on physical conditions in hospital-based services, with concurrent neglect of sensory and cognitive impairments, would indicate that sections of the disabled population of the district go unassisted. It may be that motor skills were viewed as a priority for early stage development in the younger caseload seen by occupational therapy, and cognition and communication seen as more relevant to the older, school-aged population. Nevertheless, the objective of “early intervention” identified by the occupational therapy service appears to be restricted to the physical domains of development. The limited opportunities for CPD may be another factor in caseload activity, which constrains the development of practice. However, the degree level studies of five staff suggest that professional growth is happening in the education sector.
It was observed that intervention approaches assigned to cases in each sector followed similar lines, with mainly physical approaches being adopted in the health sector, and approaches with a more cognitive orientation in the special education sector. Naturally, the professional background and related practitioner skills of personnel will influence the focus of practice. However, the extent to which continuity of care can be assured for the child with a developmental condition when intervention approaches appear to be divided according to professional background of staff employed in health or education is debatable. In high-income countries, speech and language therapy is acknowledged as the profession dealing with communication difficulties, the absence of which, in Kilifi, had led to the occupational therapists and teachers assuming responsibility for this aspect. Each profession appeared to deal with this area quite differently. The teachers identified “speech” work and “Kenyan Sign Language” amongst the interventions delivered to the children attending special school. However, the occupational therapists referred to “sensory stimulation” and “massage” as the techniques selected for their “speech therapy” work. Thus, the underlying pedagogy for each profession appears to be the driver behind approaches selected for speech work, with the occupational therapists focusing more on the oral musculature and the teachers more on the behavioural aspects of speech and language.
Limitations
The variation and scarcity in caseload documentation, which ranged from sketchy notes on paper, to notebooks read out by the key informant, challenged the veracity of data collected. The list of variables employed to facilitate extraction of data from documentary sources had variable success, particularly on the service user side. For example, variables about the “primary & secondary condition”, “type of need assistance required”, “duration of difficulty” and “social inclusion” yielded inconsistent information. This meant a reliance on retrospective accounts of key informants, where information supplied could not be validated and essential detail was often missing.
In conclusion, rehabilitation provision for children 0–15 years and their families in Kilifi District is affected by poor staffing levels and inadequate resources. The urban location of services together with a poor transport system was a perceived barrier to uptake by children and their families. Rehabilitation activities appear to be informed by professional background of practitioners, which may be at the expense of meeting needs. If people with disabilities are to have access to rehabilitation services as recommended by the United Nations Convention on the Rights of People with Disabilities [Citation40], and if practice is to be relevant and effective, there needs to be greater investment in rehabilitation provision. This might include development of outreach practice and improving capacities to work with and contribute to the development of Community-Based Rehabilitation programmes so that better access to support for all is achieved. Finally, there needs to be better understanding of the importance of skills for monitoring and evaluating practice.
Declaration of interest
The study was funded by the CP Trust. The authors report no conflicts of interest. Charles Newton is supported by Wellcome Trust, UK [No. 083744].
Acknowledgements
We would like to thank the Director of Kenya Medical Research Institute for permission to publish the data. We are grateful to the CP Trust (UK) for funding the project and to KEMRI/Wellcome Trust research programme for their support. Thanks must also go to those people involved in rehabilitation in Kilifi District, whether as provider or user.
References
- World Health Organization, Disability & Rehabilitation Team. Disability and rehabilitation status: review of disability issues and rehabilitation services in 29 African countries. Geneva: World Health Organization; 2004
- Haig AJ, Im J, Adewole D, et al. The practice of physical and rehabilitation medicine in sub-Saharan Africa and Antarctica: a white paper of a black mark? J Rehabil Med 2009;41:401–5
- Hartley S, Finkenflugel H, Kuipers P, Thomas, M. Community-based rehabilitation: opportunity and challenge. Lancet 2009;374:1803–4
- Tinney MJ, Chiodo A, Haig A, Wiredu E. Medical rehabilitation in Ghana. Disabil Rehabil 2007;29:921–7
- Njelesani J, Couto S, Cameron D. Disability and rehabilitation in Tanzania: a review of the literature. Disabil Rehabil 2011;33: 2196–207
- Parnes P, Cameron D, Christie N, et al. Disability in low-income countries: issues and implications. Disabil Rehabil 2009;31:1170–80
- World Health Organization. Rehabilitation. In: World report on disability. Geneva: World Health Organization, The World Bank; 2011:93–134
- Association for Physically Disabled Kenya (APDK). Available from: http://www.kenyadisability.or.ke/index.php/resources/disabled-persons-organizations/57-association-for-the-physically-disabled-of-kenya [last accessed 15 Jan 2013]
- Brouillette R. The rehabilitation of hearing loss: challenges and opportunities in developing countries. In: McPherson B, Brouillette R, eds. Audiology in developing countries. Boston (MA): Nova Science Publishers; 2008:141–66
- Dal Poz MR, Gupta N, Quain E, Soucat ALB. Handbook on monitoring and evaluation of human resources for health – with special applications for low-and middle-income countries. Geneva: World Health Organization; 2009
- Bangirana P, Idro R, John CC, Bolvin MJ. Rehabilitation for cognitive impairments after cerebral malaria in African children: strategies and limitations. Trop Med Int Health 2006;11:1341–9
- Cameron DL, Nixon S, Parnes P, Pidsadny M. Children with disabilities in low-income countries. Paediatr Child Health 2005;10:269–72
- Mont D. Measuring disability prevalence. Disability & Development Team, Social Protection unit, The World Bank; 2007
- Olness K. Effects on brain development leading to cognitive impairment: a worldwide epidemic. J Dev Behav Pediatr 2003;24:120–30
- Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet 2007;370:878–89
- International World Federation of Occupational Therapy, Human Resources Project. Electronic citation. Available from: http://www.wfot.org/ResourceCentre.aspx/ [last accessed 15 Jan 2013].
- World Health Organization. International Society for Prosthetics and Orthotics Guidelines for training personnel in developing countries for prosthetics and orthotics services. Geneva: World Health Organization; 2005
- Frantz J. Challenges facing physiotherapy in Africa. Internet J Appl Health Sci Pract 2007;5:1--5
- Shakespeare T, Iezzoni LI, Groce NE. The art of medicine: disability and the training of health professionals. Lancet 2009;374:1815–16
- Willis-Shattuck M, Bidwel P, Thoma S, et al. Motivation and retention of health workers in developing countries: a systematic review. BMC, Health Services Res 2008;8:247
- Dart G. ‘My eyes went wide open’ – an evaluation of the special needs education awareness course at Molepolole College of Education, Botswana. Br J Spec Educ 2006;33:130–8
- Kristensen K, Omagor-Loican M, Onen N, Okot D. Opportunities for inclusion? The education of learners with special educational needs and disabilities in special schools in Uganda. Br J Spec Educ 2006;33:139–47
- Ackers J, Hardman F. Classroom interaction in Kenyan primary schools. Compare J Comparative Int Educ 2001;31:245–61
- Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Pol Plan 2004;19:69–79
- Makinen M, Waters H, Rauch M, et al. Inequalities in health care use and expenditures: empirical data from eight developing countries and countries in transition. Bull World Health Organ 2000;78:55–65
- Ambikile JS, Outwater A. Challenges of caring for children with mental disorders: experiences and views of caregivers attending the outpatient clinic at Muhimbili National Hospital, Dar es Salam, Tanzania. Child Adolesc Psychiatry Mental Health 2012;6:16
- Gona JK, Mung’ala-Odera V, Newton CR, Hartley S. Caring for Children with disabilities In Kilifi, Kenya: what is the carer’s experience? CHILD: Care Health Dev 2011;37:175–83
- Hamzat TK, Mordi EL. Impact of caring for children with cerebral palsy on the general health of their caregivers in the African community. Int J Rehabil Res 2007;30:191–4
- Raina P, O-Donnell M, Rosenbaum P, et al. The health and well-being of caregivers of children with cerebral palsy. Paediatr 2005;115:e626–36
- Raina P, O-Donnell M, Schwqellnus H, et al. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatr 2004;4:1–13
- Amooti-Kaguna B, Nuwaha F. Factors influencing choice of delivery sites in Rakai district of Uganda. Soc Sci Med 2000;50:203–13
- Mbuba CK, Ngugi AK, Fegan G, et al. Risk factors associated with the epilepsy treatment gap in Kilifi, Kenya: a cross-sectional study. Lancet Neurology 2012;11:688–96
- Moïsi JC, Nokes JD, Gatakaa H, et al. Sensitivity of hospital-based surveillance for severe disease: a geographic information system analysis of access to care in Kilifi district, Kenya. Bull World Health Organ 2011;89:102–11
- Kilifi Health Demographic and Surveillance System [KHDSS], 2012. Electronic citation. Available from: http://www.kemri-wellcome.org/khdss/ [last accessed 15 Jan 2013]
- Carter JA, Neville BG, White S, et al. Increased prevalence of epilepsy associated with severe falciparum malaria in children. Epilepsia 2004;45:978–81
- Carter JA, Lees JA, Gona JK, et al. Severe falciparum malaria and acquired childhood language disorder. Dev Med Child Neurology 2006;48:51–7
- Gona JK, Hartley S, Newton CRJ. Using participatory rural appraisal [PRA] in the identification of children with disabilities in rural Kilifi, Kenya. Rural Remote Health 2006;6:553
- Mung’ala-odera V, Meehan R, Njuguna P, et al. Validity and reliability of the ‘Ten Questions’ questionnaire for detecting moderate and severe impairments in children aged 6–9 years in rural Kenya. Neuroepidemiology 2004;23:67–72
- Taylor-Powell E, Renner M. Analysing qualitative data. Programme development and evaluation. Madison (WI): University of Wisconsin-Extension, Cooperative Extension; 2003
- United Nations. Convention on the rights of persons with disabilities; 13th December 2006 [cited 19 Jun 2012]. Available from: http://www.un.org/disabilities/default.asp?id=150 [last accessed 15 Jan 2013]

