Abstract
Purpose: To describe the effects of a rehabilitation program in a neurological inpatient unit in terms of independence for activities of daily living and return to work. Method: Retrospective study with 148 adults with stroke, traumatic brain injury (TBI), spinal cord injury, and Guillain–Barré syndrome admitted as rehabilitation inpatients within a 1-year period for hospitalization at the Instituto de Reabilitação Lucy Montoro, Brazil. According to their diagnostic groups, subjects undergone semi-standardized models of intensive multidisciplinary rehabilitation for 4–6 weeks. Primary outcome measures: Functional Independence Measure (FIM™), Modified Rankin scale (Rankin), and Glasgow Outcome Scale (GOS Subjects were evaluated at admission, discharge, and 6 months after discharge. Results: Improvement in motor FIM™, Rankin and GOS was observed in all groups. Cognitive FIM™ increase was less evident in TBI patients. After 6 months, 37.6% of patients were unemployed, 34% underwent outpatient rehabilitation, and 65.2% maintained gains. Conclusions: This is the first report on the effects from an inpatients rehabilitation model in Brazil. After a short intensive rehabilitation, there were motor and cognitive gains in all groups. Heterogeneity in functional gains suggests more individualized programs may be indicated. Controlled studies are required with larger samples to compare inpatient and outpatient programs.
The proposed brief model of rehabilitation for stroke, traumatic brain injury, spinal cord injury, and Guillain–Barre syndrome inpatients shows promising results in terms of functional improvement.
Apparent improvements in cognitive and motor levels can be observed after 30 d of the intensive hospital-based program five times a week focusing on caregiver and patients training.
After 6 months of discharge, more than one third of patients remained out of work, but appeared to have kept the benefits attained during hospitalization, and performed physical activities in the community as outpatients.
Implications for Rehabilitation
Introduction
Sub-acute rehabilitation interventions contribute to functional gain and quality of life under neurological conditions [Citation1]. Although the isolated decrease of impairment level partly explains the reduction of disability, therapies are additional factors in functional gain [Citation2], because they stimulate reorganization of motor engrams and enhance neuroplasticity, thus minimizing the impact of a subjacent condition [Citation3]. Although there has been a growing interest in new technologies, pharmaceutical and electrophysiological research, stem cells, tissue engineering, and brain–computer interface, traditional multidisciplinary programs are the most extensively provided rehabilitation care and is available in most environments. In Brazil, outpatient neuro-rehabilitation models are preferred as the mainstay strategy for most patients with multiple needs because patients can immediately apply what is learned at the Rehabilitation Center in their daily routine. Patients are usually admitted during the sub-acute phase and undergo treatment three times a week for at least 6 months, usually until there is a plateau of functional acquisitions. Conversely, hospitals dedicated to inpatient rehabilitation have recently been introduced in our country as a new rehabilitation model.
Efficacy of inpatient rehabilitation has been studied worldwide for the main disabling conditions, using outcome measures such as functioning, mortality, return to work, quality of life, and symptomatic improvement. Besides, cost-effectiveness and long-term effects are not well established. For neurological diseases, interdisciplinary inpatient rehabilitation [Citation4–6] is related to more functionally independent patients, and the functional gain after their rehabilitation does not seem to be related to age bracket [Citation7,Citation8]. However, practical care parameters in neurological rehabilitation have not yet been defined in Brazil and there is no evidence on the efficacy of this new model of rehabilitation care with a pre-defined length of stay. Also, the socio-demographic profile of the disabled patients referred to our service remains unclear in spite of evidence of the low functioning level among the population of patients with comorbidities, which indicates an unsatisfied demand for rehabilitation [Citation9].
This retrospective study aimed to describe new models of inpatient rehabilitation for some neurological conditions and report their effects on the performance of activities of daily living and participation at the moment of discharge and after a 6-month follow up.
Methods
Subjects and program
Data were collected from all charts of adult patients consecutively admitted from October 2009 to October 2010 at the Instituto de Reabilitação Lucy Montoro (IRLM), which was, at that time, the only inpatient unit for rehabilitation of neurological conditions within the public healthcare system in the city of São Paulo.
For admission into this unit, there is an interdisciplinary screening procedure considering the following criteria: clinical stability and good control of comorbidities, family/caregiver support, neurological condition with less than 2 years since onset (acquired brain damage, spinal cord injury, and acute demyelinating polyradiculoneuritis), the existence of a disability that is disrupting to patient or caregiver, and the ability/willingness to participate in an intensive rehabilitation program [Citation10]. Each patient is admitted for one single hospitalization.
Services are provided by interdisciplinary teams led by physiatrists with the collaboration of professionals described in . During the hospitalization, the full-time presence of a caregiver, typically a family member, is required.
Table 1. Predefined number of weekly therapeutic sessions with each professional at the inpatient rehabilitation unit according to the diagnostic group.
Patients undergo an intensive interdisciplinary program of 4–6 weeks; therapies are offered 5 d a week. After defining short-term goals, the treatment is focused on performing activities independently, either by improving their physical or cognitive abilities, or by orienting their caregivers. Emphasis is given to training the caregiver as a therapeutic agent after hospitalization, keeping in mind that the continuation of the treatment in rehabilitation services is not guaranteed. During hospitalization, caregivers are subject to three institutional approaches: they receive personalized technical training for the care of the patient; attend to a 1-d collective course; watch a video focusing their own psychological, physical and cultural needs.
The program is set according to a weekly schedule of individual sessions described in in addition to the routine health care in the ward. The number of sessions varies, depending of the patient impairments observed at clinical evaluation, but the overall structure of the program is maintained in four predefined care models corresponding to four diagnostic groups: stroke (ST), traumatic brain injury (TBI), spinal cord injury (SCI), and Guillain–Barre syndrome (GB). Each of these four diagnostic groups is further divided according to the severity of functional impairments. Specific therapeutic objectives for each subgroup are:
Stroke [Citation11]:
Mild (Rankin 2): gait training, adaptation to orthoses and walking aids, fine use of upper limbs, safe swallowing, advanced speech skills, independence in activities of daily living.
Moderate (Rankin 3): balance training/standing, global strengthening, therapeutic gait, adaptation to orthoses and walking aids, spasticity control, functional speech/adaptation to alternative communication resources, improving swallowing skills, independence in activities of daily living, cognitive-behavioral interventions to shape more appropriate outcomes and post discharge plans.
Severe (Rankin 4–5): activity training with standing devices, global strengthening, positioning in bed/prevention of decubitus ulcers, orthoses for positioning and prevention of deformities, spasticity control, neuropsychological assessment, psychological support to patient and family, sphincter training, pain control.
Traumatic Brain Injury [Citation12]
Mild (GCS 13–15): gait and balance training, adaptation to orthoses and walking aids, fine use of upper limbs, safe swallowing, advanced speech skills, independence in activities of daily living, vocational counseling, orientation for social rights and post discharge plans.
Moderate (GCS 9–12): balance training/standing, global strengthening, therapeutic gait, adaptation to orthoses and walking aids, spasticity control, functional speech/adaptation to alternative communication resources, improving swallowing skills, independence in activities of daily living, cognitive-behavioral interventions to shape more appropriate outcomes and post discharge plans. Drugs to improve attention and behaviour may be tested.
Severe (GCS 3–8): activity training with standing devices, global strengthening, positioning in bed/prevention of decubitus ulcers, orthoses for positioning and prevention of deformities, spasticity control, neuropsychological assessment, psychological support to patient and family, sphincter training, pain control.
Spinal Cord Injury [Citation13]
Paraplegia: Bladder and bowel control, pain control, prevention of deformities and decubitus ulcers, adaptation to orthoses, transfers, standing, gait training, psychological support, vocational counseling, independence in activities of daily living, nutritional orientation.
Tetraplegia: prevention of deformities and decubitus ulcers, adaptation to orthoses and wheelchair, prevention of reflex dysautonomy, global strengthening, breathing exercises, bladder and bowel control, pain control, psychological support.
Guillain–Barre
Mild/lower limb involvement: Bladder and bowel control, pain control, prevention of deformities and decubitus ulcers, adaptation to orthoses, transfers, standing, gait training, psychological support, vocational counseling, independence in activities of daily living, nutritional orientation.
Severe/four limb involvement: prevention of deformities and decubitus ulcers, adaptation to orthoses and wheelchair, global strengthening, breathing exercises, bladder and bowel control, pain control, assessment of swallowing, psychological support and vocational counseling.
Therefore, each of the four groups receives a set of predefined therapies with individual variations, according to the requirements observed after evaluation of each therapeutic modality at the beginning of hospitalization. Therapies are offered both in the ward and at the Rehabilitation center. After discharge, the patients are instructed to access rehabilitation units of low complexity for maintaining the functional status they have reached.
Design
We present a retrospective study with three assessments: day 1 of admission, day of discharge, both performed by the multidisciplinary team, and a structured follow-up telephone interview 6 months after discharge, completed by a social worker.
Data and outcome measurements
We used the Functional Independence Measures (FIM™) [Citation14–16], length of stay, Glasgow Outcome Scale (GOS) [Citation17,Citation18], and Rankin Scale [Citation11] as the primary outcome measures, which have been extensively studied regarding reliability and validity. The validated Brazilian version of FIM [Citation14–16] measures independence in 18 tasks, each one ranging in score from 1 to 7 and addressing motor activities, sphincter control, and cognitive skills. The score ranges from 18 to 126, and higher scores indicate higher independence. The Rankin scale is used for measuring the degree of disability in the daily activities among stroke survivors [Citation11]. It is the most widely used clinical outcome measure for cerebrovascular clinical trials and is composed of 6 levels, ranging from normal (0) to dead (6). The GOS is a brief descriptive outcome scale for brain injury. There are five levels, ranging from 1 (dead) to 5 (good recovery) [Citation17,Citation18]. Independent variables were age, gender, years in school, period from injury to admission for inpatient rehabilitation, and diagnosis.
Phone interview at 6-month follow-up checked for employment, rehabilitation adherence, social life, and functional status. GB and SCI patient answered the phone interview, whereas ST and TBI ones with cognitive of communication impairments would need the caregivers to answer the questions. Each feature was graded in 3 to 5 Likert options:
Employment: 1 – work leave or sick leave; 2 retired (disability retirement, retirement by age or length of service); 3 – fully returned to work or study; 4 – returned to adapted work or study; 5 – other (has never worked/studied/contributed to social security).
Rehabilitation adherence: 1 – performs therapies at home; 2 – performs therapies in community facilities; 3 – does not perform any; 4 – enrolled in an outpatient model at a rehabilitation center.
Social life: 1 – inactive; 2 – resumed some leisure activities; 3 – completely restored social and leisure activities.
Functional status: 1 – retains acquired improvements; 2 – decreased functional abilities; 3 – improved when compared to before hospitalization at IRLM.
Ethics and data analyses
The study was approved by the Internal Review Board of the Hospital das Clínicas at the University of São Paulo (approval number 0252/11), and the patients signed an informed consent term before inclusion in the study.
Data were analyzed by Excel 2003 for Windows, and SPSS 15.0 (SPSS Inc., Chicago, IL). Quantitative variables were summarized in means and standard deviation, while qualitative variables were presented as a proportion of each category. Normal distribution of FIM values was demonstrated, thus initial and final values were compared using the ANOVA (repeated measures, 2 factors) and Bonferroni corrections for multiple comparisons were performed when needed. Other results were analyzed as to their distribution, and their initial and final values were suitably compared by parametric or non-parametric tests (Wilcoxon test for paired samples and Kruskal–Wallis test). Association between the qualitative variables was made using the chi-square test. The level of significance was 5%.
Results
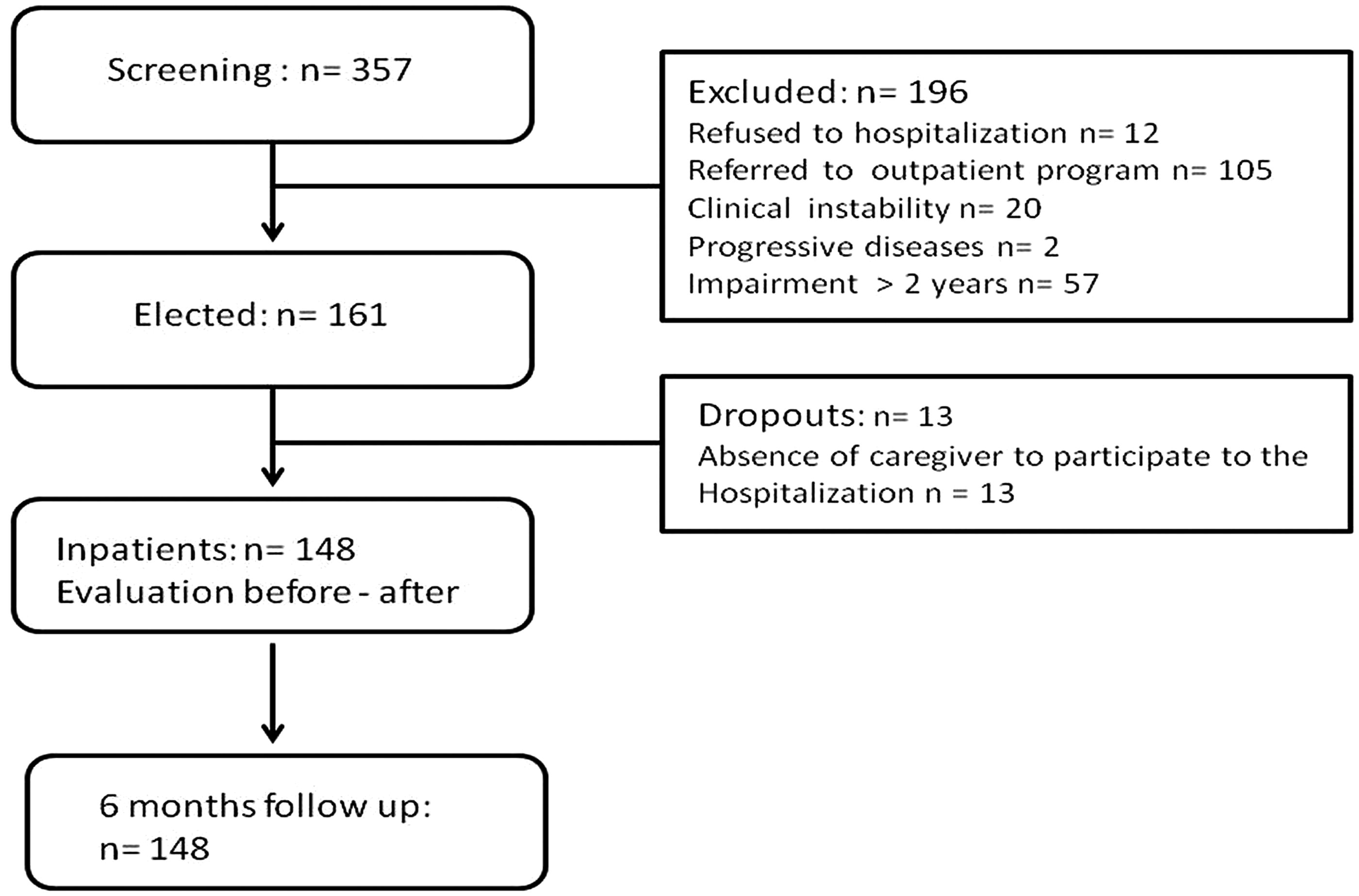
This study follows STROBE patterns (Strengthening the Reporting of Observational studies in Epidemiology), when applicable [Citation19]. Of the 357 screened patients, 209 did not fulfill the inclusion criteria: refused to be hospitalized, clinical instability, progressive illnesses (such as dementia), impaired for longer than 2 years, or could not be accompanied by a caregiver (). Therefore, the final sample had 148 subjects: stroke (28 subjects), traumatic brain injury (29 subjects), spinal cord injury (83 subjects), and Guillain–Barre syndrome (8 subjects).
Groups were similar according to gender and geographic origin (50.67% lived in São Paulo city, 37.16% were from other cities from the state, and 12.3% from other states), but ST patients were older and better educated. For all groups, the mean period from impairment to admission for inpatient rehabilitation was longer than 1 year. Due to major confidence intervals and sample variability, there was no statistical significance among groups, in spite of the observed difference regarding diagnostic to hospitalization time (). According to the institutional standards, length of stay was about 1 month (), regardless of diagnosis, although individual demands could influence this period. Length of stay was similar among the diagnostic groups.
Table 2. Socio-demographic and clinical characteristics of the patients.
There was functional improvement specific to TBI and ST, measured by GOS and Rankin, respectively (, Wilcoxon test, paired samples). Motor and cognitive FIM improved in all groups, except by cognitive FIM for SCI.
Table 3. Description of Rankin, GOS, cognitive and motor FIM according to diagnosis.
Data from the 6-month follow-up phone interview for the four diagnostic groups showed that patients were not working either due to sick leave or retirement (59.6%), were socially inactive (37.6%), attended rehabilitation therapies in the community (34%) or at home (19.9%), and retained their acquired functioning levels (65.2%). Twenty-three patients did not participate in this interview: 18 (12.1%) had wrong phone numbers, 4 (2.8%) died and 1 (0.7%) refused to participate. Adherence to therapies after hospitalization was not associated to the city or region where the subject lived.
Discussion
The framework of the Brazilian public health system relies on a regionalized network SOUZACOSTA [Citation20] in which simpler interventions are organized by the cities and more complex strategies in State or Regional level. Only in 2001 this hierarchical network was described for rehabilitation interventions [Citation21]. The State of São Paulo was the first one to order different levels of complexity, ranging from local therapeutic services, usually with one or two professions, to complex multiprofessional inpatients setting as described here. This is the first description of interventions in these rehabilitation wards in the country. This may limit generalizability, but we believe this may represent a model to be followed by other states in Brazil and other countries without organized inpatient rehabilitation.
Early access to rehabilitation centers is associated with better functional outcomes, quality of life and general satisfaction [Citation5], although this was not observed in our data. The interval between diagnosis and the rehabilitation program startup was greater than the time frame recommended in previous studies [Citation22,Citation23]. This is due to the scarcity of rehabilitation centers throughout the country, lack of knowledge regarding the need for the rehabilitation process after clinical stabilization, and poor administrative integration between clinical services and rehabilitation centers. Therefore, late access of patients led to this inpatient rehabilitation program which mixes sub-acute interventions (strategies designed to enable recovery of impairments, compensation of disabilities and preventive techniques), and chronic demands (work focused on social re-entry, community and domestic functional independence, and the reduction of handicaps).
In opting for pre-defined therapeutic models lasting 4–6 weeks, there is better planning and management of requirements, both in terms of material and hiring of specialized professionals, thus optimizing costs and allowing the access of hospitalization for a broader portion of this disabled population. This short period of inpatient rehabilitation requires clear definition of short-term functional objectives for the patients as well as focus on training the caregivers to keep some interventions after discharge. Thus inpatient and outpatient rehabilitative care are complementary strategies, and functional outcomes should be sought beyond hospitalization [Citation24]. Average cost for the inpatient multiprofessional rehabilitation for 6 weeks at the IRLM is US$ 11 368.00, while the cost of outpatient standard program of 6 months is US$ 12 910.80 [Citation25]. However, it is still necessary to analyze cost-effectiveness comparing inpatient and outpatients rehabilitation models. Other public services also report hospitalization periods of 14–104 d [Citation26], or 11–48 d [Citation23], or even up to 44 d [Citation5,Citation22] reflecting the socio-demographic variability as well as technical resources and rehabilitation goals.
Short periods require intensive organization of therapies [Citation20,Citation24], up to 6 h a day, and the team must be alert to identify signs of exhaustion, which can be more common among recently impaired or unconditioned patients. As we have described, the number of weekly therapeutic interventions with each professional varied according to the diagnoses and severity of impairment (). This distribution was based on the local clinical expertise of the service with outpatients. This explains the absent predefinition of speech and language therapy for paraplegics. On the other hand, cognitive issues among TBI and ST patients require more cognitive assistance.
Besides describing these models, we intended to show their clinical results. Data from inpatients assisted during the first year of operation of the IRLM indicate that after an intensive hospital-based program 5 times a week, focusing on caregiver and patients training, there was an improvement of cognitive and motor levels, measured by FIM™, Rankin and GOS. Patients waited almost 2 years between diagnosis and service admission, so we can believe the improvement was not spontaneous, since the period of impairment restoration had long past. All diagnostic groups showed better motor and cognitive independence levels by discharge.
Independence gain is one of the main objectives of the rehabilitation programs. However, the measure of this construct depends on indirect observation, as the one performed in this study. Rankin and GOS showed low sensibility to clinical change, but were chosen because they are ubiquitous in other studies, and permit comparisons. FIM™ is sensitive to register functional gains during rehabilitation, and has high internal consistency [Citation27]. This work showed that the FIM™ was able to reveal motor and cognitive gains, noted in all diagnostic groups [Citation11,Citation12].
Motor FIM™ improvement suggests that length of stay is sufficient to allow functional gain, regardless of neural recovery. This finding is in line with expected and previous data from inpatient and outpatient neurorehabilitation programs [Citation28]. Conversely, although cognitive function also improved among groups, its evolution is uneven. There was improvement in ST and TBI, but not in GB and SCI – because these are basically motor conditions, and cognitive scores depart from a high value at the beginning of hospitalization. Cognitive deficits are relevant in acquired brain lesions (especially TBI), and represent one of the main rehabilitation goals of such patients. Regarding the four diagnoses of the sample, there are little data on the efficacy of different rehabilitation strategies, but one might suggest that methods incorporating compensation techniques and functional training with specific regimens of intensity, frequency, and specificity play a key role for the optimization of functional improvement for these patients [Citation4]. For TBI and GB, the rehabilitation efficacy is not yet clear [Citation22–24]. Functional improvement was observed in all groups of clinical conditions, and the gain was independent of gender or age – both young and elderly benefit from hospitalization for rehabilitation [Citation8].
After 6 months, 37.6% of patients remained out of work due to sick leave, but kept the benefits attained during hospitalization (65.2%), and performed physical activities in the community as outpatients (34%).
These numbers suggest that, although retained after discharge, the acquired functional gains were not enough to allow full return to work and social life. Another explanation may include physical and attitudinal barriers towards people with disability, as well as the limited public policies in Brazil, which do not provide worker assistance for adapted positions. The majority of this sample is composed by workers with poor formal education and with limited options for relocation for new adapted jobs. These factors stimulate the continuation of financial compensation for those still on sick leave or retirement. However, this discussion is beyond the scope of this study.
The main strength of this study lies in the fact that it is an observational study without any artificial process of subject allocation or selection, it accurately reflects the clinical reality of an inpatient unit of rehabilitation. Due to the heterogeneous nature of the sample, FIM was chosen to enable comparison of the groups; it is widely used as a tool for the evaluation of rehabilitation services and the monitoring of functional gains. Although data are relatively limited, FIM scores have been used as functional outcome predictors in patients with neurological conditions submitted to rehabilitation [Citation29]. Because it is a new facility, IRLM is prone to change rehabilitation models and may test new solutions. Besides, due to the lack of national data on rehabilitation, the results of this study may be a reference in relation to future studies in the field. Although a qualitative interview was used and not a validated questionnaire, the phone call accessed the subjective opinion of the patients themselves, and also information regarding their social status 6 months after hospitalization, with no data loss. The follow-up made it possible to gather functional data beyond the immediate moment after discharge.
However, the study has limitations. First, although it covers all patients hospitalized over a 1-year period, the sample is small. Second, a non-controlled study cannot derive any causal link between functional achievements and the rehabilitation strategies. However, data may suggest functional improvement. Comparison to one untreated group or sham would be ethically questionable [Citation30]. Third, the functional evaluation was based on FIM™ (a sensitive, non-specific instrument), associated with two non-sensitive specific tools (Rankin for ST and GOS for TBI). Other scales could have been chosen, such as the FAM™ (Functional Assessment Measure) [Citation31], for providing more robust functional data and exploring the cognitive aspects of abilities. FIM™ could be used as a measure of change at follow-up as well [Citation32]. Fourth, because one of the main goals of the interdisciplinary inpatient program is the caregiver training to enable him to reproduce the rehabilitation strategies in real environments, a specific evaluation of a caregiver’s learning and burden might be necessary.
In conclusion, we have described a new model of short multidisciplinary adult inpatients rehabilitation, provided in a public facility, which produced benefits in functioning in ST, SCI, TBI, and GB. By the end of 6 months of discharge, most patients retained those functional achievements, but social participation was still a problem. Further studies comparing inpatient and outpatient models, with more specific functional instruments and cost-effectiveness analysis, may guide the decision-making process toward rehabilitation strategies for neurologically impaired population.
Acknowledgements
The authors wish to thank Marta Imamura MD, PhD (Clinical Research Center of the Instituto de Reabilitação Lucy Montoro).
Declaration of interest
The authors report no conflict of interest.
References
- Prvu Bettger JA, Stineman MG. Effectiveness of multidisciplinary rehabilitation services in postacute care: state-of-the-science. A review. Arch Phys Med Rehabil 2007;88:1526–34
- Roth EJ, Heinemann AW, Lovell LL, et al. Impairment and disability: their relation during stroke rehabilitation. Arch Phys Med Rehabil 1998;79:329–35
- Dimyan MA, Cohen LG. Neuroplasticity in the context of motor rehabilitation after stroke. Nat Rev Neurol 2011;7:76–85
- Kollen B, Kwakkel G, Lindeman E. Functional recovery after stroke: a review of current developments in stroke rehabilitation research. Rev Recent Clin Trials 2006;1:75–80
- Wang H, Camicia M, Terdiman J, et al. Time to inpatient rehabilitation hospital admission and functional outcomes of stroke patients. PM R 2011;3:296–304
- Collaboration. SUT. Organised inpatient (stroke unit) care for stroke. Cochrane Database of Systematic Reviews 2007;CD000197. DOI: 10.1002/14651858.CD000197.pub2.(4)
- Denti L, Agosti M, Franceschini M. Outcome predictors of rehabilitation for first stroke in the elderly. Eur J Phys Rehabil Med 2008;44:3–11
- Gosselin S, Desrosiers J, Corriveau H, et al. Outcomes during and after inpatient rehabilitation: comparison between adults and older adults. J Rehabil Med 2008;40:55–60
- Jorge LL, Sugawara AT, Carneiro MSO. The general hospital inpatient referred to Physical Medicine Department: functional level and epidemiological profile. Acta Fisiatr 2006;13:124–9
- Riberto M, Jucá SSH, Miyazaki MH, Battistella LR. The triage process in rehabilitation centers. Acta Fisiatr 2010;17:130–3
- Cincura C, Pontes-Neto OM, Neville IS, et al. Validation of the National Institutes of Health Stroke Scale, Modified Rankin Scale and Barthel Index in Brazil: the role of cultural adaptation and structured interviewing. Cerebrovasc Dis 2009;27:119–22
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974;2:81–4
- Marino RJ, Barros T, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003;26:S50–6
- Riberto M, Miyazaki MH, Jorge-Filho D. Reprodutibilidade da versão brasileira da Medida de Independência Funcional. Acta Fisiatr 2000;8:45–52
- Riberto M, Miyazaki MH, Jucá SSH, et al. Validation of the Brazilian version of Functional Independence Measure. Acta Fisiatr 2004;11:72–6
- Riberto M, Pinto PPN, Sakamoto H, Battistella LR. Functional Independence of spinal cord injured patients. Acta Fisiatr 2005;12:61–6
- Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet 1975;1:480–4
- Jennett B, Snoek J, Bond MR, Brooks N. Disability after severe head injury: observations on the use of the Glasgow Outcome Scale. J Neurol Neurosurg Psychiat 1981;44:285–93
- Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med 2007;147:W163–94
- Souza GCA, Costa ICC. Twenty years of SUS: reflections in a context of changes. Saude Soc 2010;19:509–17
- Ministério da Saúde – Portaria N° 793 de 24 de abril de 2012 [Internet]. Brasilia, Brazil. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/prt0793_24_04_2012.html [last accessed 4 Apr 2014]
- Lee HC, Chang KC, Huang YC, et al. Inpatient rehabilitation utilization for acute stroke under a universal health insurance system. Am J Manag Care 2010;16:e67–4
- Kuptiratsaikul V, Kovindha A, Massakulpan P, et al. Inpatient rehabilitation services for patients after stroke in Thailand: a multi-centre study. J Rehabil Med 2009;41:684–6
- Evans RL, Connis RT, Haselkorn JK. Hospital-based rehabilitative care versus outpatient services: effect on functioning and health status. Disabil Rehabil 1998;20:298–307
- IRLM Internal audit – Annual Report. Sao Paulo, SP, Brazil: Planisa Planejamento e Organização de Instituições de Saúde (in Portuguese); 2011
- Gagnon D, Nadeau S, Tam V. Clinical and administrative outcomes during publicly-funded inpatient unit rehabilitation based on a case-mix group classification. J Rehabil Med 2005;37:45–52
- Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil 1993;74:531–6
- Schönle PW. Outpatient and inpatient neurological rehabilitation – a follow-up comparison. Rehabilitation (Stuttg) 2002;41:183–8
- Chumney D, Nollinger K, Shesko K, et al. Ability of functional independence measure to accurately predict functional outcome of stroke-specific population: systematic review. J Rehabil Res Dev 2010;47:17–29
- Fregni F, Imamura M, Chien HF, et al. Challenges and recommendations for placebo controls in randomized trials in physical and rehabilitation medicine: a report of the international placebo symposium working group. Am J Phys Med Rehabil 2010;89:160–72
- Jorge LL, Marchi FH, Hara AC, Battistella LR. Brazilian version of the Functional Assessment Measure: cross-cultural adaptation and reliability evaluation. Int J Rehabil Res 2011;34:89–91
- Passalent LA, Tyas JE, Jaglal SB, Cott CA. The FIM™ as a measure of change in function after discharge from inpatient rehabilitation: a Canadian perspective. Disabil Rehabil 2011;33:579–88