Abstract
Purpose: This paper describes a continuum of customized exercise options for people with an existing and newly acquired disability or diagnosis referred to as the Transformative Exercise Framework. Background: The period directly after rehabilitation is a critical juncture where many individuals return to life with high rates of sedentary behavior. After rehabilitation discharge, people with newly acquired disability or diagnoses often never make the transition into usage of community-based exercise services that are tailored, safe and effective. Methods: Narrative review. Results: The Transformative Exercise Framework supports a patient-to-participant, rehab-to-wellness model that emphasizes a linkage between physical and occupational therapists and community-based exercise trainers. The four focus areas – Rehabilitation, Condition-specific Exercise, Fitness and Lifetime Physical Activity – emphasize a range of options for people with newly acquired disability and diagnoses, or for people with existing disability and/or chronic health conditions who have a new injury, secondary condition or are severely deconditioned. Conclusion: The concept of transformative exercise is to support people with disabilities and diagnoses with a seamless restore–improve–prevent continuum of programs and services. This continuum connects individuals to rehabilitation and exercise professionals in a dynamic framework, which maximizes the expertise of both sets of professionals and provides the most effective interventions to achieve the greatest gains in health and function and/or to avoid future health decline.
Patients discharged from rehabilitation should be transformed into participants in lifelong physical activity through a continuum of health services, which we refer to as Transformative Exercise.
Transformative exercise is a continuum of individually tailored exercise strategies/programs that aims to improve the function of underperforming systems, which inhibit community and/or lifelong physical activity participation.
The Transformative Exercise Framework can be used by a therapist or exercise trainer to design a program that maximizes performance and time and is based on a specific process for identifying short and long term goals.
Implications for Rehabilitation
Introduction
Health trajectories in the general population are typically impacted by lifestyle behaviors and genetics, yet there is a third, less understood, dimension in people with disabilities: the onset and course of secondary health conditions and their “weighted” or “additive” effect on changes in health and function [Citation1–3]. As illustrated in and [Citation4], some of the highest rates of physical secondary conditions () include pain, fatigue, deconditioning, and mobility limitations. High rates of psychosocial secondary conditions () include anxiety, isolation, problems sleeping and depression. On average, people with disabilities report 4–13 secondary conditions [Citation5–9]. These health conditions impose substantial limitations on various body structures and functions, negatively impacting rates of participation in general life activities including employment, social and community engagement and performing instrumental activities of daily living [Citation10–16].
Figure 1. Physical secondary conditions among an aggregate of studies in people with disabilities compared to a sample of the general adult population. A median percent sample of zero indicated that the condition was either not reported or measured in the sample. Modified with permission from Rimmer et al. [Citation4].
![Figure 1. Physical secondary conditions among an aggregate of studies in people with disabilities compared to a sample of the general adult population. A median percent sample of zero indicated that the condition was either not reported or measured in the sample. Modified with permission from Rimmer et al. [Citation4].](/cms/asset/8fee097d-6c3d-4baf-906b-c2a5241f6a66/idre_a_1047967_f0001_c.jpg)
Figure 2. Psychosocial secondary conditions among an aggregate of studies in people with disabilities compared to a sample of the general adult population. A median percent sample of zero indicated that the condition was either not reported or measured in the sample. Modified with permission from Rimmer et al. [Citation4].
![Figure 2. Psychosocial secondary conditions among an aggregate of studies in people with disabilities compared to a sample of the general adult population. A median percent sample of zero indicated that the condition was either not reported or measured in the sample. Modified with permission from Rimmer et al. [Citation4].](/cms/asset/47d28efb-833a-496a-9704-2a046189a6ec/idre_a_1047967_f0002_c.jpg)
While the benefits of physical activity on health are universal, physical activity and its subset, exercise, are an extremely important means for management and prevention of secondary conditions [Citation17–19]. Unfortunately, the most recent data from the US National Health Interview Survey (NHIS) reported that 47.1% of US adults with a disability, aged 18–64 years, are physically inactive (reporting no bouts of aerobic physical activity lasting 10 min or more per week) compared to only 26.1% of adults without disabilities [Citation20]. Inactive adults with a disability were 50% more likely to report one or more chronic diseases compared to those who were physically active.
The point of no return: post-rehabilitation health decline
Rehabilitation is the first step towards restoring the health and function of a patient who has just acquired a disability or has returned to a rehabilitation program as a result of an exacerbation of a pre-existing disability. From 1994 to 2001, the US healthcare system has reduced inpatient and outpatient rehabilitation from a median of 20 to 12 days [Citation21]. This trend continues today for several disability subgroups. For example, a recent cross-sectional analysis of 371 211 people with stroke in the US reported a mean decline in length of stay between 2002 and 2007 [Citation22]. This report, along with others [Citation23,Citation24], suggests that shortened length of stays may be associated with decreased functional gains achieved at rehabilitation discharge. As a result, many individuals post-rehabilitation may not achieve the functional gains that are necessary to reach a threshold for independent and productive living after discharge. This theoretical threshold represents a minimum level of function that is required for an individual to perform their activities of daily living and actively maintain or improve their current health status [Citation25]. Functional levels below this threshold may result in negative health trajectories, including the inability to stay active and reduce the risk of chronic health conditions that are associated with sedentary behavior (e.g. obesity, cardiometabolic disease).
A prospective study of six rehabilitation centers across the US [Citation26] has confirmed some of this suspicion and reported that patients who received less physical therapy and had shorter stays during rehabilitation were more likely to be rehospitalized within a year after inpatient rehabilitation discharge. Out of 951 people with spinal cord injury, 36% were rehospitalized. Additionally, recent national data provided by the US Agency for Healthcare Research and Quality reported that out of 307 877 Medicare beneficiaries post-stroke, 44 379 patients were readmitted within a 30-day period, with 5322 of these cases (12%) suggested preventable through either improvements during hospitalization, discharge planning, follow-up care or better transitional partnerships between inpatient and outpatient teams [Citation27]. Taken together, evidence suggests that reduced length of stays may be linked to decreased functional status, ultimately increasing rates of rehospitalization and institutionalization. The immediate period after rehabilitation discharge is a critical window of opportunity for intervention.
Difficult Transition from patient to participant
To address the critical period post-rehabilitation, many therapists will recommend a home-based exercise program that the patient is expected to continue independently. However, poor adherence to such interventions after discharge from physical and occupational therapy is common [Citation28,Citation29]. Over time, this results in a loss of the recovered gains achieved from rehabilitation, and sedentary behavior worsens physical function. This may have some relationship to the aforementioned high rates of rehospitalization in some populations [Citation30,Citation31]. Additionally, as a person with a disability remains inactive, physical deconditioning occurs that worsens and increases the risk of secondary conditions. In turn, this leads to even greater levels of inactivity, which results in a constant cyclical pattern of physical deconditioning known as Disability Associated Low Energy Expenditure Deconditioning Syndrome (DALEEDS) [Citation32].
Today, many people who acquire a disability or are newly diagnosed (e.g. Parkinson's, multiple sclerosis) never make the transition from “rehabilitation patient” to “exercise participant” [Citation33]. After rehabilitation, recreation, leisure and fitness participation are often impeded by a community that is underprepared to support their health and wellness needs [Citation34,Citation35]. Several barriers to exercise have been identified, including inaccessible fitness and recreation centers, inexperienced staff, insufficient resources to pay for program and transportation costs, and lack of social support from friends or family [Citation36–41]. In addition to these external barriers, many people with newly acquired disability or a new diagnosis may perceive their condition as a limitation to improving their health. On the contrary, there is strong evidence that significant improvements in health can occur post-injury or post-diagnosis [Citation42]. Thus, a gap is created that makes it challenging for a patient to integrate or reintegrate into community exercise directly after rehabilitation.
Building the crossroad between rehabilitation and lifetime physical activity
The goal of transformative exercise is to assist individuals in moving along a continuum that transitions them from a patient in rehabilitation to a participant in lifelong physical activity. We define transformative exercise as a continuum of individually adapted exercise strategies/programs that aim to improve the function of underperforming systems (e.g. neuromotor, cardiorespiratory, musculoskeletal, mental, metabolic), which inhibit community and/or lifelong physical activity participation. In accordance with the mission statement provided by the National Institutes of Health (NIH) [Citation43], transformative exercise aims to prevent and protect people with disabilities from an onset or exacerbation of chronic and/or secondary health conditions that occurs with sedentary behavior, while also enhancing or improving health and function.
Promoting healthy lifestyles among people with a newly acquired disability (e.g. spinal cord injury, head injury, stroke, limb loss), diagnosis of a condition (e.g. multiple sclerosis, Parkinson's) or exacerbation of a secondary condition (e.g. joint pain, fatigue, edema, weight gain, reduced balance) requires a careful and thoughtful transition across a continuum of transformative exercise. For the gains achieved during rehabilitation to be maintained and improved upon, and for continued recovery post-disability, diagnosis or injury, the Transformative Exercise Framework must begin in the rehabilitation setting with early interaction between therapists and trainers [Citation25,Citation43,Citation44]. This will help to bridge the gap between the focus of therapist-assisted training in clinical settings to continued training by exercise professionals in community-based settings.
The primary advantage of the Transformative Exercise Framework is that it encompasses the combined expertise of both therapists and exercise trainers to maximize the health and function of people with disabilities and chronic health conditions. Adaptations under the guidance of qualified professionals should be made to the exercises, equipment and programs offered across the range of services to meet the specific goals/needs of the individual. Examples of such professionals may include physical or occupational therapists or specialty fitness trainers who are certified to work with individuals with disabilities. Ultimately, health services that are part of the Transformative Exercise Framework will maximize collaboration among qualified providers to ensure that the environment is safe, appropriate and comfortably-paced for the individual.
The Transformative Exercise Framework
illustrates a framework that emphasizes the transformation of patients into participants. The distinction between the two is critical: care in a hospital setting is where patients begin their rehabilitation and need the full-time care from physical and occupational therapists. After they are discharged, however, it is important that they continue their recovery in the community and learn to self-manage their own health. Having therapists and exercise professionals work together early on in the process is rarely seen in health care [Citation45,Citation46], even though it can be one of the most important strategies for ensuring a successful patient-to-participant transformation.
Figure 3. The Transformative Exercise Framework supports a patient-to-participant, rehab-to-wellness model that emphasizes a linkage between physical medicine and rehabilitation, physical and occupational therapy and community-based exercise.

The three overarching goals of the Transformative Exercise Framework are Restore, Improve and Prevent. Subsumed under each goal are four overlapping focus areas: Rehabilitation, Condition-specific Exercise, Fitness and Physical Activity. Each focus area targets a set of health-related issues that are specific to the needs of the individual and are based on various baseline assessments. In order to better understand the individual's deficits and needs, the International Classification of Functioning, Disability and Health (ICF) [Citation47] provides a framework and language to describe the health and health-related states from two different perspectives: the perspective of the body (classification of body functions and body structures), and the perspective of the individual and society (classification of activities and participation). Body functions are the physiological functions of the body systems, which include both physical and psychological functions. Impairments are limitations in body function or structure that result in a significant deviation or loss of that organ or system.
The second component in the ICF model is Activities and Participation. Activities are defined as the execution of tasks or actions by an individual, and Activity Limitations are difficulties in executing certain types of activities. Participation is defined as involvement in a life situation, and Participation Restrictions are problems an individual experiences in a life situation. Activity limitations often lead to participation restrictions and both are associated with disability.
Focus Area 1: Rehabilitation. This first phase of treatment occurs during the acute or subacute stage in a hospital (inpatient) or clinical/home (outpatient) setting. This period usually lasts from a few days to a few weeks depending on the severity of the condition and what insurance companies or national health insurance programs are willing to pay. In accordance with the ICF model [Citation47], the focus of treatment is therapeutic in nature with a heavy emphasis on restoring “body functions and structures” and/or improving the impairments associated with them. The therapist diagnoses and manages the condition and a treatment plan is written for the patient based on physical and psychological needs. The primary goal is to restore physical function and prevent the onset and/or symptoms associated with a disability, diagnosis or injury [Citation48]. Mobility and self-care are critical target areas in the Recovery phase and certain strategies (i.e. techniques, adaptations, assistive technology) are used to recover function and independence in ADL/IADL and teaching patients how to use a new assistive device (e.g. wheelchair, walker, cane) to maintain ambulation.
Focus Area 2: Condition-specific Exercise. Focus Area 2 serves more in the capacity of being transformative in nature; that is, targeting improvements to specific systems that are associated with or causing one or more secondary conditions. Training should continue and build upon a pre-established recovery plan designed in Focus Area 1. In situations where an individual is not in rehabilitation but has an accident that doesn't require hospitalization (e.g. fall) or develops a new secondary health condition, a specific set of exercises is recommended. Common examples of condition-specific exercise training include those that focus on strength, balance, sitting and standing posture, mechanics (e.g. gait, wheelchair propulsion, walking-up stairs, etc.), locomotion and IADL improvements (e.g. carrying groceries, climbing stairs, performing transfers).
The number and type of secondary conditions that often accommodate disabilities requires a more streamlined process that focuses on the deficient system(s). In line with the ICF model, the primary domain that therapists and trainers are targeting falls under “activity limitations” [Citation47]. The individual is limited in performing certain activities (e.g. walking, doing household chores, exercising) because of the new injury or severity of the secondary condition. Two of the most common secondary conditions reported in people with physical disability are pain and fatigue [Citation49,Citation50]. Both secondary conditions can be mitigated with condition-specific exercise training that targets the system most responsible for the condition. In the case of pain and fatigue, several studies have reported success using warm-water exercises [Citation51–53] or body weight supported treadmill training [Citation54,Citation55] to improve these conditions.
Another unique feature of Focus Area 2 is that individuals are supported by an environment that allows them to comfortably perform a more concentrated dose of exercise, with the oversight and combined expertise of both therapists and specialty fitness trainers. For example, if an individual with multiple sclerosis has an exacerbation and is diagnosed with an increased risk of falls by the physical or occupational therapist, a specialty trainer may implement a comprehensive (high frequency/duration) balance training program to prevent or reduce the risk of falls. Likewise, if the rate limiting factor of community ambulation is lower extremity weakness, a high intensity progressive resistance training program may be prescribed to improve lower extremity strength and function [Citation56,Citation57]. These programs require a greater amount of supervised time. Unlike Focus Area 1, Focus Area 2 could range in duration from a couple of weeks to several months depending on the individual's needs and his/her level of progress. The decreased length of formal rehabilitation makes Focus Area 2 extremely important for ensuring that individuals make a smooth transition from rehabilitation to fitness and lifetime physical activity.
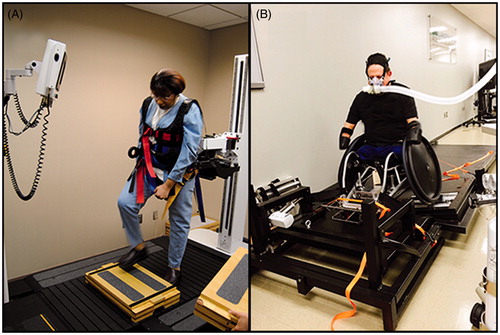
Condition-specific Exercise Training is ideally implemented in specialty fitness facilities where there is a range of exercise equipment that would support a comprehensive training program with oversight, when necessary, from a rehabilitation professional. This might include a body weight supported harness and low speed treadmill for neuromotor, balance, or cardiorespiratory training. Additional equipment may include biofeedback devices attached to fitness equipment that provide real-time performance feedback (e.g. step placement on a treadmill, visually observing slow, static training on a digital readout), functional electrical stimulation to improve muscle strength and bone mass, warm-water pools for pain relief, mat tables for easy transfer on and off the floor for performing flexibility exercises, and accessible modes of aerobic equipment for improving cardiovascular function, such as arm ergometers, wheelchair trainers/treadmills () and recumbent steppers.
Figure 4. (A) A fully interactive robotic body weight support system that provides a safe, yet challenging, method for mobility and balance training (KineAssist). (B) A roller dynamometer that provides a method of stationary wheelchair propulsion training and testing (WheelMill System).
Health professionals who implement condition-specific training should have an approved license (i.e. PT/OT) or certification related to working with people with disabilities or chronic health conditions. For fitness professionals, the American College of Sports Medicine (ACSM) has two certifications associated with this type of training: Certified Inclusive Fitness Trainer (CIFT) and Registered Clinical Exercise Physiologist (RCEP). Similarly, the National Strength and Conditioning Association (NSCA) offers exercise professionals the Certified Special Populations Specialist (CSPS).
Focus Area 3: Fitness. In Focus Area 3, the two primary target systems are the cardiorespiratory and musculoskeletal systems [Citation58]. Participants in this focus area do not require interventions that are condition-specific. Program components include a variety of activities that target aerobic capacity, muscular strength and endurance, power, balance, body composition and flexibility. Standard fitness equipment found in this setting includes exercise machines, free weights and small items such as balls, ropes and mats.
In Focus Area 3, participants independently manage their program with oversight/guidance from a fitness instructor and, when necessary, consultation from a therapist. The emphasis is on addressing mild-to-moderate “activity limitations” that are commonly found in inactive people to prevent DALEEDS [Citation32]. The exercise prescription follows the standard ACSM guidelines for intensity, frequency and duration [Citation59]. After a baseline assessment, the trainer uses various types of modalities to improve both the cardiorespiratory and musculoskeletal systems. For example, a circuit training program could be prescribed to simultaneously improve both cardiorespiratory and musculoskeletal health outcomes [Citation60].
Ideally, a fitness/conditioning program should include a range of exercise options targeting both systems (cardiorespiratory and musculoskeletal). This will help the individual to reduce the risk of chronic (e.g. hypertension, heart disease) and secondary (e.g. pain, weight gain, falls) health conditions [Citation32]. In some cases a personal trainer will be extremely helpful in prescribing appropriate exercise, offering a variety of activities to reduce boredom or burnout and serving as a motivator to keep the individual adherent to the exercise regimen.
Focus Area 4: Lifetime Physical Activity. A major emphasis in Focus Area 4 is on skill acquisition and lifetime physical activity. Once an individual achieves a targeted level of fitness and reaches a plateau, the emphasis in Focus Area 4 shifts from improvement to prevention and from intensity-driven exercise to sustainable lifetime physical activity. Preventive exercise protects such systems as the cardiac, circulatory, metabolic and mental systems [Citation61] by reducing the risk of obesity, hypertension [Citation62], hyperlipidemia, type 2 diabetes [Citation63,Citation64], falls [Citation65], poor sleep quality [Citation66], depression [Citation67] and many others. Settings for participating in lifetime physical activity are typically larger facilities that, in addition to a fitness area with strength and cardiorespiratory equipment, have an indoor walking track, swimming pool, courts for team sports (e.g. basketball, racquetball, etc.), and a multipurpose room for group exercise classes.
In accordance with the ICF model, the focus of this phase is to reduce the risk of “participation restrictions” by providing socially engaging, enjoyable forms of physical activity that can be maintained across the lifespan. Adherence to regular physical activity is a common problem in the general population but is often an even greater problem in people with disabilities and chronic conditions because of the larger number of secondary health conditions that make it difficult to exercise (e.g. pain, fatigue), or because there are more environmental barriers that must be overcome (e.g. cost of the program, limited transportation, accessible facility) [Citation41,Citation68].
Activities in Focus Area 4 should emphasize group dynamics and skill acquisition. Group dynamics involve a participant joining an exercise class that builds social cohesion with other members of the class and has consistently been shown to improve adherence [Citation69–71]. Other benefits of group exercise may include adopting positive exercise behaviors of the group [Citation72], and reduced stress [Citation73]. Sample recreational activities include tennis/wheelchair tennis, golf with or without an accessible golf cart, various forms of adapted dance, hiking, handcyling/cycling and warm-water aquatics classes, such as volleyball or tai chi. Several of these forms of exercise require skill acquisition in areas where learning and practice precede successful and efficient execution of the activity (e.g. a new dance routine, learning how to play wheelchair tennis, taking a martial arts class such as judo or karate).
After individuals plateau in Focus Area 3 (Fitness), there is a risk that they may not recognize the importance of lifelong physical activity to protect themselves from various health risks. One method of addressing the lack of intercommunication between the participant and health professional, if the technology is available, would be an internet-based “booster” exercise class (through the computer or web-TV). This session could be offered to assist the person in gradually getting back into regular physical activity through mild exercises, such as breathing, relaxation techniques and stretching. Booster sessions have been shown to retain self-directed exercise participation after rehabilitation [Citation74]. More importantly, these booster sessions can reestablish a social connection between the trainer and participant. This interaction may also provide a critical window of opportunity for the implementation of behavioral change strategies, which are imperative to maintain adherence.
Behavior change strategies facilitate transformation
Long-term adherence (retention) is often measured as the pinnacle of success for interventions and is instrumental for transforming patients into participants along this Transformative Exercise Framework. Attitudinal and motivational elements are critical towards enhancing adherence. Interventions that contain only an exercise component are often not successful in retaining participation among people with disabilities [Citation75,Citation76]. One method of promoting retention is to incorporate behavior change strategies into an intervention, which have been found to strongly improve long-term exercise adherence in a variety of populations [Citation77–79].
Behavior modification strategies are based on well-grounded theories, such as Bandura's social cognitive theory [Citation80,Citation81], Transtheoretical model [Citation82] or the Physical Activity for People with a Disability (PAD) model [Citation18], all of which identify variables that are associated with a behavior, as well as the strategies and pathways that encourage behavior to change. Examples of these strategies include periodic counseling sessions focused on increasing motivation [Citation83,Citation84], self-management/empowerment programs combined with telephone support [Citation85], and tailored interventions provided in a community setting [Citation86].
Facilitating a patient's transformation to a participant in lifetime physical activity is not a rapid process, but requires an ongoing behavioral change in lifestyle. Programs that incorporate these tools must be carefully designed to achieve the desired effects and to extend across the lifespan, as different constructs or strategies have varying effects on participation and long-term adherence [Citation87]. For example, to be successful at maintaining adherence, some evidence suggests that interventions should be individually tailored [Citation75,Citation88], promote some form of social support (i.e. between the participant and a family member, between participants or between the participant and the therapist/trainer), help people to understand that engagement in physical activity can improve their health and fitness [Citation87], and/or focus on addressing environmental barriers that limit physical activity and enhance their self-esteem [Citation89]. Most importantly, interventions must reinforce the idea that the pathway to improved health through physical activity is a long process of behavior change that requires persistence to be successful, as continued use of these strategies has been identified as a predictor of long-term engagement [Citation90]. A seamless transition along the four focus areas of the Transformative Exercise Framework will require sustained adherence and should be viewed as a long-term process of behavior change.
Behavior change strategies will be different in each Focus Area of the framework, as they must be feasible for the individual as well as the health professional. For example, it may be optimal for therapists who have limited time with their patients in Focus Area 1 (Rehabilitation) to utilize behavioral strategies that are brief in nature. Such strategies include identifying participants' interests and goals related to physical activity during rehabilitation or referring them directly to specialty fitness trainers or programs upon discharge [Citation44]. Longitudinal behavioral strategies such as motivational interviewing or coaching may be best suited for health professionals in Focus Areas 2 and 3.
Placement on the Transformative Exercise Framework
While an ideal situation is for a person to continuously progress along the Transformative Exercise Framework (restore–improve–prevent), adverse health events or major functional losses can return an individual to a previous focus area. This could be caused by an accident, such as a fall, any serious medical event or even physical deconditioning (i.e. DALEEDS). For example, if a person post-stroke who has progressed from Rehabilitation (Focus Area 1) to engagement in A group physical activity program in the community (Focus Area 4) experiences a second stroke, he/she may again require a return to Rehabilitation followed by Condition-specific Exercise and Fitness before returning to the community program. Likewise, if an older adult who jogs recreationally (Focus Area 4) develops knee pain, he/she may require outpatient rehabilitation from a therapist followed by condition-specific training exercises to reduce the load on the knee and to improve jogging mechanics.
The Transformative Exercise Framework (restore–improve–prevent) is cyclical in nature, extending the significance of this framework not only to people who are discharged after rehabilitation, but also to those who may experience exacerbations or newly acquired conditions/disabilities throughout their lifespan.
Summary
The substantial gap between rehabilitation and lifetime physical activity can be closed with a framework that supports a patient-to-participant, therapist-to-trainer delivery model. The Transformative Exercise Framework can either start in Rehabilitation and progress through the three other focus areas ending with lifetime Physical Activity, or if an individual does not require hospitalization or outpatient rehabilitation, he/she can enter the framework in any one of the three focus areas depending on need (Condition-specific Exercise, Fitness, Physical Activity). The Transformative Exercise Framework has three primary goals: (1) prevent loss of continuity between rehabilitation and community exercise; (2) improve the quality of services through customization of exercise programs that target specific health and functional issues; and (3) reduce recidivism (dropout) rates by establishing closer connectivity between physicians, therapists, trainers and participants and promoting socially engaging physical activity through a combination of community-based activities and behavioral strategies, such as telecoaching, to improve motivation.
Declaration of interest
The contents of this publication were developed under a grant from the Department of Health and Human Services, Administration for Community Living, National Institute on Disability, Independent Living, and Rehabilitation Research, RecTech, HHS#90RE5009-01-00.
References
- White G, Gutierrez RT, Seekins T. Preventing and managing secondary conditions: a proposed role for independent living centers. J Rehab 1996;62:14–20
- Kinne S. Distribution of secondary medical problems, impairments, and participation limitations among adults with disabilities and their relationship to health and other outcomes. Disabil Health J 2008;1:42–50
- Rasch E, Magder L, Hochberg MC, et al. Health of community-dwelling adults with mobility limitations in the United States: incidence of secondary health conditions. Part II. Arch Phy Med Rehabil 2008;89:219–30
- Rimmer JH, Chen M-D, Hsieh K. A conceptual model for identifying, preventing and treating secondary conditions in people with disabilities. Phy Ther 2011;91:1728–38
- Campbell M, Sheets D, Strong PS. Secondary health conditions among middle-aged individuals with chronic physical disabilities: implications for unmet needs and services. Asst Tech 1999;11:105–22
- Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health 2004;94:443–5
- Wilber N, Mitra M, Walker D, et al. Disability as a public health issue: findings and reflections from the Massachusetts survey of secondary conditions. Milbank Q 2002;80:393–421
- Ravesloot C, Seekins T, Walsh J. A structural analysis of secondary conditions experienced by people with physical disabilities. Rehabil Psychol 1997;42:3–16
- Santiago M, Coyle C. Leisure-time physical activity and secondary conditions in women with physical disabilities. Disabil Rehabil 2004;26:485–94
- Lollar D, Crews, JE. Secondary conditions. In: Albrecht GA, ed. Encyclopedia of disability. Thousand Oaks: Sage; 2005:1288--93
- Ipsen C. Health, secondary conditions, and employment outcomes for adults with disabilities. J Disabil Policy Studies 2006;2:77–87
- Krause J. Secondary conditions and spinal cord injury: a model for prediction and prevention. Top Spinal Cord Inj Rehabil 1996;2:58–70
- Drum C, Krahn G, Culley C, et al. Recognizing and responding to the health disparities of people with disabilities. Californian J Health Promot 2005;3:29–42
- Krause J, Bell RB. Measuring quality of life and secondary conditions: experiences with spinal cord injury. In: Simeonsson R, McDevitt L, eds. Issues in disability and health: the role of secondary conditions and quality of life. Chapel Hill (NC): University of North Carolina Press; 1999:51--72
- Jensen MP, Chodroff MJ, Dworkin RH. The impact of neuropathic pain on health-related quality of life: review and implications. Neurology 2007;68:1178
- Charlifue S, Weitzenkamp DA, Whiteneck GG. Longitudinal outcomes in spinal cord injury: aging, secondary conditions, and well-being. Arch Phys Med Rehabil 1999;80:1429–34
- Durstine JL, Painter P, Franklin BA, et al. Physical activity for the chronically ill and disabled. Sports Med 2000;30:207–19
- van der Ploeg HP, van der Beek AJ, van der Woude LHV, et al. Physical activity for people with a disability: a conceptual model. Sports Med 2004;34:639–49
- Rimmer J, Shenoy, SS. Impact of exercise on targeted secondary conditions. In: Field MJ, Jette AM, Martin L, eds. Workshop on disability in America. Washington, DC: National Academies Press; 2006:205--21
- Carroll DD, Courtney-Long EA, Stevens AC, et al. Vital signs: disability and physical activity – United States, 2009–2012. MMWR Morb Mortal Wkly Rep 2014;63:407–13
- Ottenbacher K, Smith PM, Illig SB, et al. Trends in length of stay, living setting, functional outcome, and mortality following medical rehabilitation. JAMA 2004;292:1687–95
- O'Brien SR, Xue Y, Ingersoll G, Kelly A. Shorter length of stay is associated with worse functional outcomes for medicare beneficiaries with stroke. Phys Ther 2013;93:1592–602
- Gillen R, Tennen H, McKee T. The impact of the inpatient rehabilitation facility prospective payment system on stroke program outcomes. Am J Phys Med Rehabil 2007;86:356–63
- Dobrez D, Heinemann AW, Deutsch A, et al. Impact of Medicare's prospective payment system for inpatient rehabilitation facilities on stroke patient outcomes. Am J Phys Med Rehabil 2010;89:198–204
- Rimmer JH. Getting beyond the plateau: bridging the gap between rehabilitation and community-based exercise. Phys Med Rehabil 2012;4:857–61
- DeJong G, Tian W, Hsieh CH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil 2013;94:S87–97
- Lichtman JH, Leifheit-Limson EC, Jones SB, et al. Preventable readmissions within 30 days of ischemic stroke among Medicare beneficiaries. Stroke 2013;44:3429–35
- Forkan R, Pumper B, Smyth N, et al. Exercise adherence following physical therapy intervention in older adults with impaired balance. Phys Ther 2006;86:401–10
- Carter S, Taylor D, Levenson R. A question of choice: compliance in medicine taking. London, United Kingdom: Medicines Partnership; 2003
- Nguyen HQ, Chu L, Amy Liu IL, et al. Associations between physical activity and 30-day readmission risk in chronic obstructive pulmonary disease. Ann Am Thorac Soc 2014;11:695–705
- Bohannon RW, Lee N. Association of physical functioning with same-hospital readmission after stroke. Am J Phys Med Rehabil 2004;83:434–8
- Rimmer JH, Schiller WJ, Chen M-D. Effects of disability-associated low energy expenditure deconditioning syndrome. Exer Sport Sci Rev 2012;40:22–9
- Forchheimer M, Tate DG. Enhancing community re-integration following spinal cord injury. NeuroRehabilitatin 2004;19:103–13
- Tate D, Forcheimer M. Enhancing community reintegration after inpatient rehabilitation for persons with spinal cord injury. Top Spinal Cord Inj Rehabil 1998;4:42–55
- Kirchner CE, Gerber EG, Smith BC. Designed to deter: community barriers to physical activity for people with visual or motor impairments. Am J Prev Med 2008;34:349–52
- Nary DE, Froehlich KA, White GW. Accessibility of fitness facilities for persons with physical disabilities using wheelchairs. Top Spinal Cord Inj Rehabil 2000;6:87–98
- Mulligan HF, Hale LA, Whitehead L, Baxter GD. Barriers to physical activity for people with long-term neurological conditions: a review study. Adapt Phy Act Q 2012;29:243
- Kehn M, Kroll T. Staying physically active after spinal cord injury: a qualitative exploration of barriers and facilitators to exercise participation. BMC Public Health 2009;9:168
- Arbour-Nicitopoulos K, Martin Ginis KA. Universal accessibility of “Accessible“ fitness and recreational facilities for persons with mobility disabilities. Adapt Phy Act Q 2011;28:1–15
- Rimmer JH, Riley B, Wang E, et al. Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med 2004;26:419–25
- Rimmer J, Chen M-D, McCubbin JA, et al. Exercise intervention research on persons with disabilities. What we know and where we need to go. Am J Phys Med Rehabil 2010;89:249–63
- National Institutes of Health (NIH). Mission. Available from: http://www.nih.gov/about/mission.htm [last accessed 23 Mar 2015]
- Beauchamp M, Francella S, Romano JM, et al. A novel approach to long-term respiratory care: results of a community-based postrehabilitation maintenance program in COPD. Resp Med 2013;107:1210–16
- Rimmer JH, Henley KY. Building the crossroad between inpatient/outpatient rehabilitation and lifelong community-based fitness for people with neurologic disability. J Neurol Phys Ther 2013;37:72–7
- Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Rev Peru Med Exp Salud Publica 2011;28:337–41
- Gilbert J, Yan J, Hoffman S. A WHO report: framework for action on interprofessional education and collaborative practice. J Allied Health 2010;39:196–7
- World Health Organization. International classification of functioning, disability and health (ICF). Geneva, Switzerland: World Health Organization; 2001
- American Physical Therapy Association. Guide to therapist practice. 2nd ed. American Physical Therapy Association; 2003:744
- Rimmer JH, Chen M-D, Hsieh K. A conceptual model for identifying, preventing and treating secondary conditions in people with disabilities. Phys Ther 2011;91:1728–38
- Ehde DM, Jensen MP, Engel JM, et al. Chronic pain secondary to disability: a review. Clin J Pain 2003;19:3–17
- Hinman RS, Heywood SE, Day AR. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther 2007;87:32–43
- Mannerkorpi K, Nordeman L, Ericsson A, et al. Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. J Rehabil Med 2009;41:751–60
- Jung T, Ozaki Y, Lai B, Vrongistinos K. Comparison of energy expenditure between aquatic and overground treadmill walking in people post-stroke. Physiother Res Int 2013;19:55--64
- Hunter D, Smith Cole E, Murray JM, Murray TD. Energy expenditure of below-knee amputees during harness-supported treadmill ambulation. J Orthop Sports Phys Ther 1995;21:268–76
- Martin Ginis KA, Latimer AE. The effects of single bouts of body-weight supported treadmill training on the feeling states of people with spinal cord injury. Spinal Cord 2007;45:112–15
- Ouellette MM, LeBrasseur NK, Bean JF, et al. High-intensity resistance training improves muscle strength, self-reported function, and disability in long-term stroke survivors. Stroke 2004;35:1404–9
- Macko RF, Ivey FM, Forrester LW, et al. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke. A randomized, controlled trial. Stroke 2005;26:2206–11
- Physical Activity Guidelines Advisory Committee. Physical activity guidelines advisory committee report, 2008. Washington, DC: US Department of Health and Human Services; 2008
- American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 8th ed. Baltimore: Lippincott Williams & Wilkins; 2010
- Jacobs PL, Nash MS, Rusinowski Jr JW. Circuit training provides cardiorespiratory and strength benefits in persons with paraplegia. Med Sci Sports Exerc 2001;33:711–17
- Gielen S, Laughlin MH, O'Conner C, Duncker DJ. Exercise training in patients with heart disease: review of beneficial effects and clinical recommendations. Prog Cardiovasc Dis 2015;57:347–55
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002;136:493–503
- Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement executive summary. Diabetes Care 2010;33:2692–6
- Braith RW, Stewart KJ. Resistance exercise training: its role in the prevention of cardiovascular disease. Circulation 2006;113:2642–50
- Sherrington C, Whitney JC, Lord SR, et al. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 2008;56:2234–43
- Reid KJ, Baron KG, Lu B, et al. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med 2010;11:934–940
- Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med 2000;62:633–8
- Rimmer JH, Wang E, Smith D. Barriers associated with exercise and community access for individuals with stroke. J Rehabil Res Dev 2008;45:315–22
- Fraser SN, Spink KS. Examining the role of social support and group cohesion in exercise compliance. J Behav Med 2002;25:233–49
- Carron A, Hausenblas H, Mack D. Social influence and exercise: a meta-analysis. J Sport Exerc Pscychol 1996;18:1--16
- Estabrooks PA, Carron AV. Group cohesion in older adult exercisers: prediction and intervention effects. J Behav Med 1999;22:575–88
- Plante T, Madden M, Mann S, et al. Effects of perceived fitness level of exercise partner on intensity of exertion. J Soc Sci 2010;6:50–4
- Plante T, Coscarelli L, Ford M. Does exercising with another enhance the stress-reducing benefits of exercise? Int J Stress Manage 2001;8:201–13
- Fleig L, Pomp S, Schwarzer R, Lippke S. Promoting exercise maintenance: how interventions with booster sessions improve long-term rehabilitation outcomes. Rehabil Psychol 2013;58:323–33
- Morris JH, Macgillivray S, McFarlane S. Interventions to promote long-term participation in physical activity after stroke: a systematic review of the literature. Arch Phys Med Rehabil 2014;95:956–67
- van der Ploeg H, Streppel KRM, van der Beek AJ, et al. Successfully improving physical activity behavior after rehabilitation. Am J Health Promot 2007;21:153–9
- Brekke HK, Bertz F, Rasmussen KM, et al. Diet and exercise interventions among overweight and obese lactating women: randomized trial of effects on cardiovascular risk factors. PLoS One 2014;9:e88250
- Pelletier CA, Latimer-Cheung AE, Warburton DE, Hicks AL. Direct referral and physical activity counselling upon discharge from spinal cord injury rehabilitation. Spinal Cord 2014;52:392–5
- Ellis T, Motl RW. Physical activity behavior change in persons with neurologic disorders: overview and examples from Parkinson disease and multiple sclerosis. J Neurol Phys Ther 2013;37:85–90
- Bandura A. Self efficacy: the exercise of control. New York, NY: Worth Publishers; 1997
- Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004;31:143–64
- Kosma M, Ellis R. Establishing construct validity of a stages-of-change algorithm for physical activity. Am J Health Promot 2010;25:e11–20
- Boysen G, Krarup LH, Zeng X, et al. ExStroke Pilot Trial of the effect of repeated instructions to improve physical activity after ischaemic stroke: a multinational randomised controlled clinical trial. BMJ 2009;339:b2810
- Alingh RA, Hoekstra F, van der Schans CP, et al. Protocol of a longitudinal cohort study on physical activity behaviour in physically disabled patients participating in a rehabilitation counselling programme: ReSpAct. BMJ Open 2015;5:e007591
- Huijbregts MP, Myers AM, Streiner D, Teasell R. Implementation, process, and preliminary outcome evaluation of two community programs for persons with stroke and their care partners. Top Stroke Rehabil 2008;15:503–20
- Dean CM, Rissel C, Sherrington C, et al. Exercise to enhance mobility and prevent falls after stroke: the community stroke club randomized trial. Neurorehabil Neural Repair 2012;26:1046–57
- Kosma M, Ellis R, Bauer JJ. Longitudinal changes in psychosocial constructs and physical activity among adults with physical disabilities. Disabil Health J 2012;5:1–8
- Bock B, Marcus B, Pinto B, et al. Maintenance of physical activity following an individualized motivationally tailored intervention. Ann Behav Med 2001;23:79–87
- van der Ploeg H, Streppel KRM, van der Beek AJ, et al. Underlying mechanisms of improving physical activity behavior after rehabilitation. Int J Behav Med 2008;15:101–8
- Bock BC, Albrecht AE, Traficante RM, et al. Predictors of exercise adherence following participation in a cardiac rehabilitation program. Int J Behav Med 1997;4:60–75

