Abstract
Two studies examined autonomic and cardiovascular functioning that may link school burnout to cardiovascular risk factors in young healthy adult females. Study 1 (N = 136) investigated whether school burnout was related to resting values of blood pressure (BP) and blood pressure variability (BPV) through laboratory beat-to-beat BP assessment. Study 2 (N = 94) examined the link between school burnout and diurnal BPV through ambulatory BP monitoring. Controlling for anxiety and depressive symptomatology, school burnout demonstrated strong positive relationships with indices of cardiac sympathovagal tone, sympathetic vasomotor tone, inefficient myocardial oxygen consumption, increased 24-h ambulatory heart rate and BP, blunted BP diurnal variability, and increased arterial stiffness. These studies establish cardiovascular biomarkers of school burnout and suggest that even in a seemingly healthy sample school burnout may predispose females to increased cardiovascular risk. Several future lines of research are outlined.
Introduction
Burnout, a construct developed within occupational research, has been recently extended to the school context (Parker & Salmela-Aro, Citation2011; Salmela-Aro et al., Citation2008, Citation2009), specifically to adolescents in high school. However, as important developmental processes continue in emerging adulthood (18–25 years, see Arnett, Citation2006) examining school burnout within collegiate populations merits consideration. Applied to academic populations, school burnout is conceptualized as a three-dimensional affective response to school-related stress characterized by chronic exhaustion from school-related work, cynicism toward the meaning of school and a belief of inadequacy in school-related accomplishment (Salmela-Aro et al., Citation2009). Although school burnout has been linked to such psychological and behavioral problems as depression, absenteeism, school dropout and academic underperformance (Fimian & Cross, Citation1986; Frydenberg & Lewis, Citation2004; Salmela-Aro et al., Citation2009; Yang, Citation2004), research examining the physiological underpinnings of school burnout is greatly limited (May et al., Citation2014). Therefore, two studies were conducted (assessing laboratory and ambulatory hemodynamics) to provide further insight into the relationship between school burnout and autonomic and cardiovascular precursors to deteriorated physiological health.
Study 1
Although the relationship between work burnout and cardiovascular disease (CVD) is suggested to be mediated through two physiological stress systems – the sympatheticadrenergic-medullary axis (SAM) and the hypothalamicpituitary-adrenal axis (HPA) – the specific cardiovascular and autonomic mechanisms contributing to this association have been contested (Danhof-Pont et al., Citation2011; De Vente et al., Citation2003; van Doornen et al., Citation2009). May et al. (Citation2014) provide the only research linking school burnout to physiological functioning demonstrating that males with increased school burnout display increased cardiac reactivity and impaired cardiac recovery in response to sympathetic stimulation. Furthermore, vagal rebound, defined as a marked increase in parasympathetic activity above resting levels following an acute stressor (Arai et al., Citation1989) and a condition suggestive of cardioprotective properties (Mezzacappa et al., Citation2001), was elicited in participants with lower school burnout scores but was absent in those with high burnout scores. These findings suggest that burnout may be predictive of increased risk of future CVD as elevated hemodynamic and sympathetic nervous system (SNS) activity has been shown to be indicative of early manifestations of CVD (Goldstein, Citation1983).
Although informative, the findings in May et al. (Citation2014) are limited to males, leaving the relationship between school burnout and female physiology unexplored; a limitation addressed in Study 1. Additionally, moving beyond the hemodynamics reported in May et al. (Citation2014), Study 1 incorporates autonomic nervous system markers via heart rate variability and blood pressure variability: the low frequency component of the heart rate variability (LF) and the low frequency component of the systolic blood pressure variability (LFSBP). LF indexes cardiac sympathovagal tone (i.e. the contribution the sympathetic influence on the balance of the autonomic state resulting from sympathetic and parasympathetic influences) and elevated LF has been identified as a precursor to deteriorated cardiovascular health (Goldberger, Citation1999; Goldstein, Citation1983). LFSBP reflects sympathetic vasomotor tone and links the vasculature with the autonomic nervous system (Malliani et al., Citation1991). Elevated LFSBP has been associated with a variety of negative wellness indicators (e.g. affective disorders, hypertension, autonomic nervous system disorders, Izdebska et al., Citation2004; Okamoto et al., Citation2012).
We proposed that if school burnout is associated with suboptimal physiology via elevated levels of resting hemodynamic and SNS activity, then it is reasonable to consider school burnout to be a potential risk factor for future CVD development. Therefore Study 1 evaluated the relationship between school burnout and hemodynamic and autonomic nervous system markers in a normotensive, female population via laboratory beat-to-beat BP assessment.
Methods
Participants
One-hundred and thirty-six undergraduate female students qualified for study inclusion. In an attempt to avoid potential cardiovascular functioning confounds, participants were excluded from study participation through an online health screening assessment if they smoked, exercised regularly defined as >120 min per week in the previous 6 months (as previously specified in May et al., Citation2014), were hypertensive (BP ≥ 140/90 mmHg), had chronic diseases, or were taking beta blockers, antidepressants, or stimulants. We excluded participants who engaged in physical activity that would affect generalizability to “typical/normal physiology” for a few reasons. First an individual who exercises often may have an exceptionally low resting heart rate while still maintaining a normal blood pressure range (Pokan et al., Citation1994; Sacknoff et al., Citation1994). For example, the average resting heart rate is around 70 beats per minute (bpm), but the exceptionally fit may have a resting heart rate in the 50 bpm or even the 40 bpm range. Second, without a hard measure of fitness (e.g. oxygen consumption, metabolic rate, etc.) it would be insufficient to simply statistically adjust for weekly exercise time as participants with higher fitness levels physiologically function differently than those that do not exercise (Buchheit & Gindre, Citation2006). Participants were asked to abstain from caffeine, alcohol and strenuous physical activity for at least 24 h prior to testing and were asked not to eat any food 4 h prior to testing. Participants were tested in the early follicular phase of the menstrual cycle to avoid potential variations in pressure wave morphology and cardiac reactivity. The sample was 74% Caucasian, 10% African American, 9% Asian and 7% endorsed either biracial or non-disclosed ethnicity. Participants were recruited from undergraduate classrooms as an option for voluntary class credit and all data was collected in the middle (weeks 3–9) of the fall semester. All participants gave their written consent prior to study participation as approved by The Florida State University Institutional Review Board.
Instruments and measures
Anthropometrics
Height was measured using a stadiometer and body weight was measured using a Seca scale (Sunbeam Products Inc., Boca Raton, FL). Body mass index (BMI) was calculated as kg/m2.
Blood pressure
Hemodynamic indices include heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and rate pressure product (RPP) which is a marker of myocardial oxygen consumption and efficiency (Gobel, Citation1978). Beat-to-beat HR, SBP and DBP was recorded via finger plethysmography (NIBP-100 Biopac Inc., Goleta, CA). This method has been shown to provide accurate measurement of BP changes when compared with intra-arterial BP (Imholz et al., Citation1991). RPP is computed as SBP × HR. Increases in RPP indicates increases in myocardial oxygen consumption and inefficiency (Gobel, Citation1978).
Heart rate variability
The BP peaks were used to calculate the time duration of intervals between heartbeats (RRI) and were automatically detected using commercially available software (WinCPRS, Turku, Finland). The RRIs were inspected for artifacts, premature beats and ectopic episodes in order to calculate HRV parameters. The main spectral components of the HRV that we calculated, by means of Fast Fourier transformation, were the low frequency (LF; 0.04–0.15 Hz) and the high frequency (HF; 0.15–0.4 Hz). The use of absolute units (ms2) for HF and LF may be obtained in proportion to the total power (TP) which is expressed in normalized units (nu). Normalization is used to exclude the influence of other fractal components (Anonymous, Citation1996). Since there is structural algebraic redundancy inherent in the normalized spectral HRV measures with respect to each other (nLF=1-nHF), and also with respect to the LF/HF ratio, here we report LFnu to denote cardiac sympathovagal tone (Anonymous, Citation1996; Burr, Citation2007).
Blood pressure variability
To assess BPV, the SBP time series was resampled at 5 Hz and the continuous data stream passed through a low pass impulse response filter with a cutoff frequency of 0.5 Hz. The data were then subjected to Fast Fourier transform algorithms using a Hanning spectral window and subsequently smoothed using a triangular averaging function to produce a spectrum. The power was calculated by measuring the area under the peak of the power spectra density curve. Power spectra within the 0.04–0.15 Hz range were defined as LFSBP and taken as an estimate of sympathetic vasomotor modulation (Malliani et al., Citation1991).
School burnout
School burnout was measured using the School Burnout Inventory (SBI: Salmela-Aro et al., Citation2009). The SBI consists of 9 items measuring three first-order factors of school burnout: (a) exhaustion at school (four items), (b) cynicism toward the meaning of school (three items), and (c) sense of inadequacy at school (two items). Summed scores from the first-order factors comprise a second-order overall school burnout score. All the items are rated on a 6-point Likert-type scale ranging from 1 (completely disagree) to 6 (strongly agree). Higher composite scores indicate higher burnout. Reliability for the present sample was α = 0.90.
Depression
Depression was measured using the 10-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977; Santor & Coyne, 1997). The CES-D has been widely used as a measure of depressive symptoms in nonclinical samples. It asks participants to respond to a list of ways they may have felt or behaved during the previous week. Sample items include, “I was bothered by things that usually don't bother me”, and “I felt hopeful about the future”, (reverse coded). Responses ranged from 0 = Rarely or None of the time (Less than one day) to 3 = Most or all of the time (5–7 d). Responses were summed into one overall score, with a possible range of 0 to 30. Reliability for the sample was α = 0.73.
Anxiety
Anxiety was measured using the 20-item State-Trait Anxiety Inventory (STAI; Spielberger et al., 1970). Participants were asked to respond to anxiety items such as “upset”, “calm”, “secure”, “at ease”, and “nervous”. Responses were scored on a 4-point Likert scale (1 = Not at all to 4 = Very much so). Half of the items were reverse coded so that higher scores indicated greater anxiety. Items were then summed to create a composite anxiety score with a possible range of 20 to 80. Reliability for the sample was α = 0.92.
Procedure
Participants were first introduced to the laboratory setting and familiarized with the study procedures. Anthropometric measurements were then taken followed by the completion of a health questionnaire that included a health history form and a questionnaire containing the school burnout, depression and anxiety scales. Data collection was conducted in the morning after at least an 8-h postprandial period in a quiet, dimmed light, temperature-controlled room (23 ± 1 ºC), and at the same time of the day (± 2 h) in order to minimize potential diurnal variations in vascular reactivity. After a 10-min resting period in a seated position in which brachial BP was measured and used to calibrate beat-to-beat finger BP waveforms, beat-to-beat BP was recorded for 5 min.
Statistical analysis
Pearson correlations evaluated measurement scale and health demographic associations. Univariate analysis of variance (ANOVA) evaluated ethnicity and year in school associations with school burnout. As affective disorders may have overlapping symptomatology, investigators suggest the need to control for depressive and anxiety symptoms in designs focusing on burnout measurements (Melamed et al., Citation2006; Schaufeli & Buunk, Citation2003; Shirom, 2009). Therefore analyses were constructed to demonstrate the incremental contribution of school burnout above that of anxiety and depressive symptoms in accounting for variance in physiological markers. Hierarchical multiple regression (HMR) analyses were conducted to test the association between school burnout scores and cardiovascular parameters and to demonstrate any incremental contribution of school burnout scores above anxiety and depressive symptomatology in accounting of variance in physiological variables. Model 1 of the HMR contained the anxiety and depression predictors and Model 2 introduced school burnout as a predictor. All statistical analyses were performed using IBM SPSS version 20 (Chicago, IL).
Results and discussion
Correlations indicated no statistically significant associations between SBI scores and health demographic (). However, significant Pearson correlations between SBI, STAI, and CES-D scores support the need to statistically control for anxiety and depressive symptom influences while evaluating SBI relationships with physiological variables. ANOVA analyses indicated that SBI scores were not associated with either ethnicity F(4, 131) = 1.02, p = 0.399, or year in school, F(3, 132) = 1.31, p = 274. Model 2 of the hierarchical regression analyses showed that, after accounting for anxiety and depressive symptomatology, school burnout scores significantly (p < 0.05) accounted for an additional 6% of variance in HR values, 3% in RPP values, 3% in LFnu values, and 5% in LFSBP values (). School burnout scores did not significantly account for variance in SBP, DBP or MAP values after controlling for anxiety and depressive symptomatology. Therefore, these results indicate that during a laboratory beat-to-beat BP assessment and after controlling for anxiety and depressive symptomatology, school burnout was not associated with conventional BP indices (i.e. SBP, DBP and MAP) but was associated with increased autonomic sympathetic activity (HR and LFnu), myocardial oxygen consumption and inefficiency (RPP), and vascular sympathetic activity and vasomotor tone (LFSBP).
Table 1. Study 1 and study 2 correlation matrices of health demographics.
Table 2. Hierarchal linear regression of laboratory beat-to-beat hemodynamic indices.
Study 2
As laboratory responses may not reflect real-life cardiovascular responses we next employed ambulatory blood pressure monitoring (ABPM) in the natural environment. The importance of doing so is emphasized by data suggesting that responses to stress in every-day life may be more important in understanding the development and progression of CVD than responses in the laboratory (Schwartz et al., Citation2003). Of particular importance is “non-dipping” or a pattern of blunted nocturnal BP decline that describes the inability of BP to decline throughout the nighttime hours. In comparing individuals characterized as normal nocturnal BP dippers (>10% fall in nighttime BP) with non-dippers (<10% fall in nighttime BP), non-dippers were at an increased risk of CVD with symptomatology ranging from the development of hypertension to cardiac death (Fagard et al., Citation2008; Viera et al., Citation2011).
Additionally, the ambulatory arterial stiffness index (AASI), which is calculated from ambulatory BP recordings, has been shown to be associated with the development of CVD; with increases in AASI resulting in increased cardiovascular morbidity and mortality (Adiyaman et al., Citation2008). AASI is an ideal supplement to conventional ambulatory hemodynamic indices (e.g. HR, SBP, DBP and MAP) and BP dipping values as research has shown AASI to be correlated with two gold standards of arterial stiffness: wave reflection (as measured by the augmentation index) and pulse wave velocity (Jerrard-Dunne et al., Citation2008). Importantly, measurement of arterial stiffness has been shown to be a predictor of CVD even in healthy young individuals (Berard et al., Citation2013).
Therefore, Study 2 examined the relationship between school burnout and diurnal BP variation in females through ambulatory BP monitoring. We hypothesized associations between elevated school burnout and increases in 24 h ambulatory hemodynamics, BP non-dipping and ambulatory arterial stiffness, while controlling for anxiety and depressive symptoms.
Methods
Participants
Ninety-four undergraduate female students (Mean age = 20.72 years, SD = 2.92) qualified for study inclusion. Participants were excluded from study participation through an online health screening assessment if they smoked, exercised regularly, defined as >120 min per week in the previous 6 months, were hypertensive (BP ≥ 140/90 mmHg), had chronic diseases, or were taking beta blockers, antidepressants or stimulants. Participants were asked to abstain from caffeine, alcohol and strenuous physical activity 24 h prior to the testing period and during the assessment period. Participants were tested in the early follicular phase of the menstrual cycle to avoid potential variations in pressure wave morphology and cardiac reactivity. The ethnic composition of the sample was 81% Caucasian, 9% African American, 4% Asian and 6% endorsed either biracial or non-disclosed ethnicity. Participants were recruited from undergraduate classrooms as an option for voluntary class credit and all data was collected in the middle (weeks 3–9) of the spring semester. All participants gave their written consent prior to study participation as approved by The Florida State University Institutional Review Board.
Instruments and measures
Ambulatory blood pressure monitoring
Ambulatory BP measurements were collected using validated oscillometric 90217A SpaceLabs (Spacelabs; Wokingham, Berkshire, UK) recorders and calibrated to take four measurements per hour for 24 h. Daytime and sleeping times were defined by self-reported waking and sleeping times. Dipping values were calculated (see Friedman & Logan Citation2009) as the degree of fall (%) in nocturnal MAP pressure relative to the diurnal MAP: 100 (1 – [nocturnal MAP daytime MAP]). To calculate the ambulatory arterial stiffness index (AASI), the regression slope of DBP on SBP was computed for each participant from the unedited 24 h measurements. AASI was defined as one minus the regression slope. The stiffer the arterial tree, the closer the regression slope and AASI are to zero and one, respectively (Adiyaman et al., Citation2008).
Measurement scales
As in Study 1, school burnout was measured using the SBI, depression the CES-D, and anxiety the STAI with sample α of 0.88, 0.75 and 0.88, respectively.
Procedure
After completing an online health history form, eligible participants were scheduled for a laboratory appointment to complete a 24 h ambulatory BP assessment. Upon arrival, participants completed a questionnaire containing the school burnout, depression, and anxiety scales. Anthropometrics were then measured and participants were fitted with an ambulatory BP monitoring device. Ambulatory BP setup and monitoring began between 0800 and 1100 h and concluded when the recorder was returned to the laboratory the following day.
Statistical analysis
As conducted in Study 1, Pearson correlations, multinomial logistic regressions, and hierarchical multiple regressions were utilized in Study 2.
Results and discussion
Pearson correlations indicated no statistically significant relationships between SBI scores and health demographics (). ANOVA analyses indicated that SBI scores were not associated with either ethnicity F(4, 89) = 1.11, p = 0.357, or year in school, F(3, 90) = 1.22, p = 307. Model 2 of the hierarchical regression analyses showed that, after accounting for anxiety and depressive symptomatology, school burnout scores significantly (p < 0.05) accounted for additional variance in HR, (13%) SBP (4%), DBP (7%), MAP (12%), RPP (15%), SBP dipping (8%), DBP dipping (11%), MAP dipping (12%), and ASSI (5%) values (). Therefore, utilizing ambulatory assessments these findings demonstrate that school burnout was associated with elevated 24 h HR and BP, increased myocardial oxygen consumption and inefficiency, a blunting of normal diurnal variability (non-dipping) in BP, and increased arterial stiffness (AASI). In a graphical representation comparing study findings, contains scatterplots of raw scores displaying the regression of school burnout scores on heart rate and mean arterial pressure values from Study 1 and Study 2.
Figure 1. Regression of school burnout inventory (SBI) composite scores on heart rate (HR) and mean arterial pressure (MAP) values from Study 1 and Study 2.
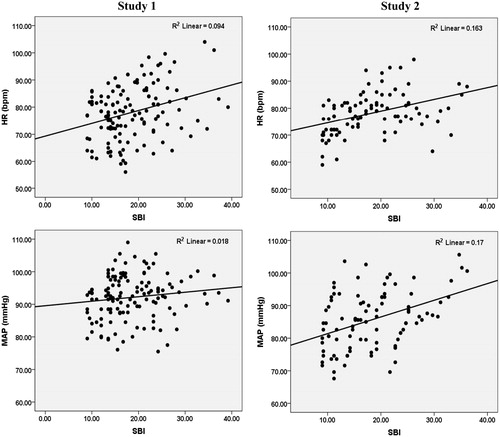
Table 3. Hierarchical linear regression analyses of ambulatory hemodynamic indices.
General discussion
Two studies were conducted assessing laboratory beat-to-beat blood pressure and then ambulatory blood pressure measurements in young females in an effort to evaluate potential cardiovascular biomarkers associated with school burnout symptomatology. These studies present the novel findings that increased school burnout was associated with (1) both cardiac sympathovagal tone (LF) and sympathetic vasomotor tone (LFSBP), (2) increased myocardial oxygen consumption and inefficiency, (3) increased 24-h ambulatory HR and BP, (4) blunted diurnal variability in SBP, DBP and MAP, and (5) increased arterial stiffness (AASI).
These findings suggest that even in a seemingly healthy sample, school burnout may predispose females to increased cardiovascular risk via elevated SNS activity, greater arterial tree stiffness and blunted diurnal variability in blood pressure. These findings are important as these indices have been shown to be early markers of impaired cardiovascular functioning.
Mechanistically, it appears that in those with greater school burnout the increase in SNS activity may potentially evoke vasoconstriction and arterial stiffness from the day into the night and subsequently it may impair the ability of BP to normally dip in the early morning hours. It is worth noting that even though laboratory assessments showed a link between markers of sympathetic activity (LFSBP, LFnu) and burnout scores, BP and RPP where not significantly correlated with SBI. However, the ambulatory assessments reveled that SBI was associated with poor blood pressure variability, increased arterial stiffness (AASI) and increased myocardial oxygen consumption (RPP). Furthermore, while Study 1 and 2 utilized differing assessment techniques and independent samples, previous research indicates ambulatory assessment, in particular, BP dipping and AASI, to be better predictors of cardiovascular outcomes when compared to laboratory or office measured BP (Adiyaman et al., Citation2008; Sega et al., Citation2005). Interestingly, BP indices displayed stronger relationships with school burnout during the ambulatory assessments than during the laboratory assessment. In addition, the AASI was significantly correlated with SBI, which may indicate that school burnout could evoke maladaptive alterations in the vasculature and baroreflex sensitivity (Stergiou et al., Citation2010; Wang et al., Citation2010). Therefore, the results of the present study suggest that prospective studies aimed at understanding the role of school burnout in the development of cardiovascular disease should pay special attention to ambulatory examinations of cardiovascular regulation.
The current research is consistent with May et al. (Citation2014) by similarly demonstrating school burnout to be related with cardiovascular functioning associated with increased cardiovascular risk. However, by examining female physiology, assessing heart rate variability and utilizing ambulatory assessments, the current research differs from May et al. (Citation2014). Furthermore, May et al. (Citation2014) demonstrated school burnout associations with hemodynamics under conditions of cardiac stress and recovery whereas the current research identified school burnout, hemodynamic and autonomic associations during resting and ambulatory conditions. Given the difference in gender and assessment methodologies between these studies, caution should be used regarding direct physiological parameter and /or gender comparisons.
In comparing school burnout and work burnout differences appear regarding hemodynamic functioning. Researchers investigating work burnout have proposed a variety of potential mechanisms to mediate the link between burnout and hypertension (i.e. metabolic processes, SAM and HPA deregulation, autonomic nervous system activation, micro-inflammation, impaired immunity functions, blood coagulation, fibrinolysis, poor health, sleep behaviors), but imbalance in hemodynamic functioning has been underemphasized (Danhof-Pont et al., Citation2011; Melamed et al., Citation2006). One potential reason is that research fails to provide a clear picture of the relationship between work burnout and hemodynamics. For example, a meta-analysis examining the relationship between work burnout and hemodynamics indicated that in comparison with controls, patients with higher burnout had significantly lower systolic BP supporting the conclusion that work burnout is not associated with hypertension (Danhof-Pont et al., Citation2011). Conversely, other studies not included in the Danhof-Pont et al. (Citation2011) meta-analysis have documented associations between work burnout and hypertension suggesting that burnout may ultimately have a negative impact on physical health (Alves et al., Citation2009; Capizzi et al., Citation2010; Yu et al., Citation2009). We believe the current research helps support the conclusion that burnout is associated with altered hemodynamic functioning and serves to help clarify the burnout-hemodynamic association. Additionally, the present study utilized a more sensitive assessment of cardiovascular functioning than those utilized in prior burnout studies. Hence, the present findings suggest a potential link between school burnout and the development of hypertension, the most common form of CVD.
To help further investigate the relationship between physiology and school burnout a variety of potential improvements to prospective studies can be suggested. In addition to study replication it may also be beneficial, given the general normotensive nature of the individuals in school burnout samples used in this research, to implement more sensitive assessment protocols that are more conductive to identifying subtle physiological changes such as stress-induced manipulations (De Vente et al., Citation2003) or expanding the analysis of 24 ambulatory BP recording into multi-day diurnal variation (Fan et al., Citation2013; van Doornen et al., Citation2009). The current studies point to the need for continued research that investigates cardiovascular functioning and school burnout in both females and males, SBI subscale relationships with cardiovascular functioning, the establishment of clinical diagnostic cutoff points for SBI scores, as well as potential age-related effects. For example, given the age of the samples used in this research, prospective studies may benefit from sampling older, nontraditional students as there may potentially be an adverse synergistic effect of school burnout and aging on the cardiovascular system.
Whereas initial school burnout research focused on adolescents, we chose to investigate school burnout in a collegiate population where academic responsibilities are perceived to be as stressful as work-related activities (Hamaideh, Citation2011); thus future research may want to examine whether adverse school burnout-cardiovascular relationships can be identified in these younger populations. Additionally, in view of Parker & Salmela-Aro's (Citation2011) demonstration of the progression and consistency of school burnout over time and findings demonstrating consistent school burnout-suboptimal academic performance (decreased undergraduate grade point averages) associations for cross-sectional data collected over six academic semesters (Brown et al., Citation2013), the longitudinal effects of school burnout on cardiac functioning and physical health need to be investigated. Finally, it may be beneficial to implement more precise measures of SNS activity via HPA or SAM axis biomarkers such as cortiosteriods and/or catecholamines concentrations in studies investigating school burnout in regards to basal physiological values and physiological stress responses (De Vente et al., Citation2003) as well as more comprehensive heart rate variability and cardiac autonomic modulation measurements.
In conclusion, these studies established autonomic and cardiovascular biomarkers of school burnout. It appears that school burnout is associated with altered cardiovascular modulation via elevated levels of resting hemodynamic and SNS activity making it reasonable to consider school burnout to be a potential risk factor for future CVD development. Elevated SNS activity has been proposed to be an early manifestation of CVD (Goldstein, Citation1983). Consequently, early detection of cardiovascular anomalies is important as it may prevent the development of less treatable forms of CVD (Chobanian et al., Citation2003; Elliott & Black, Citation2007; Goldstein, Citation1983; Kearney et al., Citation2005; Minino et al., Citation2007). Therefore, these findings have important clinical implications for the evaluation of school burnout symptoms as they may be associated with the early manifestations of cardiovascular disease and negative health consequences, even in seemingly young healthy females.
References
- Adiyaman A, Dechering DG, Boggia J, Li Y, Hansen TW, Kikuya M. (2008). Determinants of the ambulatory arterial stiffness index in 7604 subjects from 6 populations. Hypertension 52(6):1038–44
- Alves MG, Chor D, Faerstein E, Werneck, GL, Lopes CS. (2009). Job strain and hypertension in women: Estudo Pro-Saude (Pro-Health Study). Rev Saude Publica 43(5):893–6
- Anonymous. (1996). Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task force of the European Society of Cardiology Pacing Clinical Electrophysiology. Circulation 93:1043–65
- Arai Y, Saul JP, Albrecht P, Hartley LH, Lilly LS, Cohen RJ, Colucci WS. (1989). Modulation of cardiac autonomic activity during and immediately after exercise. Am J Physiol 256(1Pt2): H132–41
- Arnett JJ. (2006). Emerging adulthood: understanding the new way of coming of age. In: Arnett JJ, Tanner JL, editors. Emerging adults in America: coming of age in the 21st century. Washington, DC: American Psychological Association. p 3–19
- Berard E, Bongard V, Ruidavets JB, Amar J, Ferrieres J. (2013). Pulse wave velocity, pulse pressure and number of carotid or femoral plaques improve prediction of cardiovascular death in a population at low risk. J Hum Hypertens 9:529–34
- Brown PC, May RW, Sanchez-Gonzalez MA, Koutnik AP, Fincham FD. (2013). The relationship of school burnout, anxiety, and depressive symptoms with academic performance. Poster session presented at the 25th Annual Convention of the Association for Psychological Science; 2013 May; Washington, DC
- Buchheit M, Gindre C. (2006). Cardiac parasympathetic regulation: respective associations with cardiorespiratory fitness and training load. Am J Physiol Heart Circ Physiol 291(1):H451–8
- Burr RL. (2007). Interpretation of normalized spectral heart rate variability indices in sleep research: a critical review. Sleep 30:913–19
- Capizzi JA, Allen GJ, Murphey D, Pescatello LS. (2010). The interactive effects of metabolic syndrome, blood pressure, and mental health in worksite employees. Physician Sportsmed 38:45–53
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr. (2003). Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42(6):1206–52
- Danhof-Pont MB, Van Veen T, Zitman FG. Biomarkers in burnout: a systematic review. J Psychosom Res 2011;70:505–24
- De Vente W, Olff M, Van Amsterdam JGC, Kamphuis JH, Emmelkamp PMG. (2003). Physiological differences between burnout patients and healthy controls: blood pressure, heart rate, and cortisol responses. J Occup Environ Med 60:54–61
- Elliott WJ, Black HR. (2007). Prehypertension. Nat Clin Pract Cardiovasc Med 4(10):538–48
- Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. (2008). Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 51(1):55–61
- Fan LB, Blumenthal JA, Hinderliter AL, Sherwood A. (2013). The effect of job strain on nighttime blood pressure dipping among men and women with high blood pressure. Scand J Work Environ Health 39(1):112–19
- Fimian M, Cross A. (1986). Stress and burnout among preadolescent and early adolescent gifted students: a preliminary investigation. J Early Adolesc 6:247–67
- Friedman O, Logan AG. (2009). Nocturnal blood pressure profiles among normotensive, controlled hypertensive and refractory hypertensive subjects. Can J Cardiol 25(9):312–16
- Frydenberg E, Lewis R. (2004). Adolescents least able to cope: how do they respond to their stresses? Br J Guid Counc 32:25–37
- Gobel FL, Norstrom LA, Nelson RR, Jorgensen CR, Wang Y. (1978). The rate-pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation 57(3):549–56
- Goldberger JJ. (1999). Sympathovagal balance: how should we measure it? Am J Physiol Heart Circ Physiol 276:H1273–80
- Goldstein DS. (1983). Plasma catecholamines and essential hypertension: an analytical review. Hypertension 5(1):86–99
- Hamaideh SH. (2011). Stressors and reactions to stressors among university students. Int J Soc Psychiatr 57(1):69–80
- Imholz BP, Wieling W, Langewouters GJ, van Montfrans GA. (1991). Continuous finger arterial pressure: utility in the cardiovascular laboratory. Clin Auton Res 1(1):43–53
- Izdebska E, Cybulska I, Izdebskir J, Makowiecka-Ciesla M, Trzebski A. (2004). Effects of moderate physical training on blood pressure variability and hemodynamic pattern in mildly hypertensive subjects. J Physiol Pharmacol 55(4):713–24
- Jerrard-Dunne P, Mahmud A, Feely J. (2008). Ambulatory arterial stiffness index, pulse wave velocity and augmentation index--interchangeable or mutually exclusive measures? J Hypertens 26(3):529–34
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. (2005). Global burden of hypertension: analysis of worldwide data. Lancet 365(9455):217–23
- Malliani A, Pagani M, Lombardi F, Cerutti S. (1991). Cardiovascular neural regulation explored in the frequency domain. Circulation 84(2):482–92
- May RW, Sanchez-Gonzalez MA, Brown PC, Koutnik AP, Fincham FD. (2014). School burnout and cardiovascular functioning in young adult males: a hemodynamic perspective. Stress 1:79–87
- Melamed S, Shirom A, Toker S, Berliner S, Shapira I. (2006). Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psycho Bull 132:327–53
- Mezzacappa ES, Kelsey RM, Katkin ES, Sloan RP. (2001). Vagal rebound and recovery from psychological stress. Psychosom Med 63(4):650–7
- Minino AM, Heron MP, Murphy SL, Kochanek KD. (2007). Deaths: final data for 2004. Natl Vital Stat Rep 55(19):1–119
- Okamoto LE, Raj SR, Peltier A, Gamboa A, Shibao C, Diedrich A. (2012). Neurohumoral and haemodynamic profile in postural tachycardia and chronic fatigue syndromes. Clin Sci (Lond) 122(4):183–92
- Parker PD, Salmela-Aro K. (2011). Developmental processes in school burnout: a comparison of major developmental models. Learn Individ Differ 21:244–8
- Pokan R, Huonker M, Schumacher M, Zweiker R, Eber B, Starz I, Klein W. (1994). ECG of the athlete's heart. Acta Med Austriaca 21(3):76–82
- Salmela-Aro K, Kiuru N, Pietikäinen M, Jokela J. (2008). Does school matter? The role of school context in adolescents' school-related burnout. Eur Psychol 13(1):12–23
- Radloff LS. (1977). The CES-D Scale. Appl Psychol Meas 1:385–401
- Salmela-Aro K, Kiuru N, Leskinen E, Nurmi JE. (2009). School burnout inventory (SBI): reliability and validity. Eur J Psychol Assess 25:48–57
- Sacknoff DM, Gleim GW, Stachenfeld N, Coplan NL. (1994). Effect of athletic training on heart rate variability. Am Heart J 127(5):1275–8
- Santor DA, Coyne JC. (1997). Shortening the CES -D to improve its ability to detect cases of depression. Psychol Assessment 9:233–43
- Schaufeli WB, Buunk BP. (2003). Burnout: an overview of 25 years of research and theorizing. In: Schabracq MJ, Winnubst JAM, Cooper CC, editors. The handbook of work and health psychology. 2nd ed. West Sussex, England: Wiley. p 383–429
- Schwartz AR, Gerin W, Davidson KW, Pickering TG, Brosscho JF, Thayer JE, Christenfeld N, et al. (2003). Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Pyschosom Med 65:22–35
- Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, Mancia G. (2005). Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the pressioni arteriose monitorate e loro associazioni (PAMELA) study. Circulation 111(14):1777–83
- Shirom A. (2009). Epilogue: mapping future research on burnout and health. Stress Health 25:375–80
- Spielberger CD, Gorsuch RL, Lushene RE. (1970). Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press
- Stergiou GS, Kollias A, Rarra VC, Nasothimiou EG, Roussias LG. (2010). Arterial stiffness index based on home (HASI) vs. ambulatory (AASI) blood pressure measurements. Hyperten Res 33(7):731–6
- van Doornen LJP, Houtveen JH, Langelaan S, Bakker AB, van Rhenen W, Schaufeli WB. (2009). Burnout versus work engagement in their effects on 24-hour ambulatory monitored cardiac autonomic function. Stress Health 25(4):323–31
- Viera AJ, Zhu S, Hinderliter AL, Shimbo D, Person SD, Jacobs DR Jr. (2011). Diurnal blood pressure pattern and development of prehypertension or hypertension in young adults: the CARDIA study. J Am Soc Hypertens 5(1):48–55
- Yang H. (2004). Factors affecting student burnout and academic achievement in multiple enrollment programs in Taiwan's technical–vocational colleges. Int J Educ Dev 24:283–301
- Yu SF, Zhou WH, Gu GZ, Wu YY, Qiu Y, Wang S. (2009). Effect of occupational stress on hypertension. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 27(12):706–10
- Wang MY, Huang CJ, Wu YL, Liu JC, Tsai PS. (2010). The influence of baroreflex sensitivity on ambulatory arterial stiffness index in individuals with cardiovascular risk. Blood Press Monit 15(5):262–7

