Abstract
Polycystic ovary syndrome (PCOS) is a common endocrine disorder with a significant psychological burden throughout the life course of affected women. Thus, use of mindful awareness may be beneficial as an adjunct to conventional medical management of women with PCOS. A randomized, controlled trial was conducted at the Evgenideion Hospital of the Athens University Medical School to explore the impact of an 8-week mindfulness stress management program on measures of depression, anxiety and stress as well as on the quality of life in reproductive age women with PCOS. The study was approved by the Research Ethics Committee. Twenty-three and 15 women with PCOS were randomly allocated to the intervention or control group, respectively. All participants were administered DASS21, PSS-14, PCOSQ, Daily Life and General Life Satisfaction Questionnaires and provided three-timed daily samples of salivary cortisol, before and after the intervention. Intervention group participants were provided with the Credibility/Expectancy Questionnaire at the day of enrolment, to check for possible placebo effect on the outcome. Post-intervention, between-group results revealed statistically significant reductions in stress, depressive and anxiety symptoms, as well as in salivary cortisol concentrations, along with an increase in Life Satisfaction and Quality of Life scores in the intervention group only. There was no significant “placebo” effect on the outcome measures. Mindfulness techniques seem promising in ameliorating stress, anxiety, depression and the quality of life in women with PCOS and could be used as an adjunct method to the conventional management of these women.
Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders in reproductive age Greek women, with a prevalence of 6.7% (Diamanti-Kandarakis et al., Citation1999). It is a life-long condition of unclear etiology. Recent evidence suggests that PCOS may be associated with an imbalance of the brain stress system, i.e. enhanced reactivity of the sympathetic nervous system (Lansdown & Rees, Citation2012), the hypothalamic–pituitary–adrenal axis (Benson et al., Citation2009) and/or up-regulated expression of glucocorticoid receptors and glucocorticoid hypersensitivity (Milutinovic et al., Citation2011).
The syndrome is associated with long-term physical and mental health risks (Krępula et al., Citation2012), such as infertility (Costello et al., Citation2012), hirsutism (Roth et al., Citation2012), impaired sexual health (Mansson et al., Citation2011) and quality of life, mood disorders (Dokras, Citation2012), anxiety, depression and other stress-related symptomatology (Benson et al., Citation2009). Current treatments are only moderately effective; psychological comorbidity may interfere with patients’ compliance to proper uptake of medications or lifestyle modifications (Sundbom & Bingefors, Citation2013), thus further hindering successful response to treatment.
Recent studies suggest that complementary and alternative medicine treatments could be beneficial as an adjunct to conventional medical management of women with PCOS. Mindfulness has not been investigated in patients with PCOS, but it has been shown to reduce psychological distress and exert positive effects in non-PCOS patients (Raja-Khan et al., 2011). Mindfulness has emerged as a promising therapy for reducing stress and anxiety that accompanies daily life and chronic disease, with no negative side effects (Praissman, Citation2008). Mindfulness techniques are a clinical application of principles involving the key element of non-judgmental acceptance of psychological distress, thereby reducing the tendency to ruminate over these experiences. Several studies have shown that brain concentration to “moment-to-moment” awareness of one’s present thoughts, emotions and body sensations in a non-judgmental manner, in combination with brain plasticity, promote stress alleviation due to an enhanced relaxation response. This effect appears to be mediated by changes in brain activity and structure; in the autonomic nervous system (Kubota et al., Citation2001) and the hypothalamic–pituitary–adrenal (HPA) axis, i.e. serum cortisol reduction (Turakitwanakan et al., Citation2013); amelioration of poor sleep quality (Brand et al. Citation2012); brain temporal transcriptome changes (Bhasin et al., Citation2013); regulation of emotion (Robins et al., Citation2012) and default mode network connectivity (Brewer et al., Citation2011); increases in regional grey matter (Holzel et al., Citation2011); and enhanced focusing, sensory processing and reflective sensory experience awareness (Kilpatrick et al., Citation2011). Mindfulness has also been associated with improved glycemic control and decrease in depression, anxiety and general psychological distress in patients with type 2 diabetes mellitus (Rosenzweig et al., Citation2007). The above-mentioned facts suggest that the application of mindfulness techniques may have beneficial psychological effects on patients with PCOS.
Therefore, the aim of this study was to assess the impact of an 8-week mindfulness stress management program, accompanied by a weekly session with the principal investigator, on the depression, anxiety and stress levels, as well as on the quality of life in reproductive age women with PCOS.
Methods
Trial design
This was a parallel, two-armed, randomized controlled trial (RCT), with a 1:1 allocation ratio of participants to intervention and control groups. The study was conducted in the PCOS Clinic of the Division of Endocrinology, Metabolism and Diabetes at the Evgenideion Hospital of the Athens University Medical School, in Greece. The study was in agreement with the Helsinki Declaration. Ethical approval was obtained from the Research Ethics Committee of the Evgenideion Hospital. This trial was registered at Australian New Zealand Clinical Trials Registry (ANZCTR; Registration number: ACTRN12613000623796) and the protocol is available at: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12613000623796.
Study participants
Patients were recruited from November 2012 to May 2013. Pre-menopausal women aged 15–40 years were eligible for participation if they were diagnosed with PCOS according to the Rotterdam definition [if they fulfilled at least two of the following three criteria (a) chronic anovulation, (b) clinical and/or biochemical hyperandrogenism and (c) polycystic ovaries on ultrasound, after exclusion of related disorders]. For adolescents, at least 2 years should have elapsed from menarche to participate in the study. Exclusion criteria included pregnancy, another genetic or endocrine disorder, neuropsychiatric disorders requiring psychotropic medications (e.g. antipsychotics, antidepressants or anticonvulsants) and practice of stress management techniques within 2 months from enrolment, simultaneous participation in other trials and inability to read or write in Greek. Patients who deemed eligible and were willing to participate provided written, informed consent prior to study entry.
Participants were assessed for their social and educational status and pattern of menstruation. Each patient underwent measurement of weight, height and clinical evaluation of body hair/hirsutism with the use of Ferriman–Gallwey (FG) score. Early morning blood samples, after an overnight fasting, were obtained for determination of luteinizing hormone (LH), follicle stimulating hormone (FSH), prolactin and testosterone concentrations. The diagnosis of PCOS was set by a designated endocrinologist who examined the patients and reviewed the results. Patients who at first gave consent but then refused to undergo thorough assessment were considered as drop-outs.
Randomization – blinding
An online randomization internet site (www.random.org) was used to assign the participants to intervention and control groups. Random allocation sequence was implemented by a designated clinical assistant who was not otherwise associated with the trial. The fellow researcher who administered the questionnaires and obtained the salivary cortisol devices at the end of the 8-week period was blinded (not aware of the assigned group of the patients). No concealment was used within the groups.
Study interventions
After random assignment, participants in the intervention group were trained in the mindfulness stress management technique and were administered questionnaires and salivary cortisol collection devices, at enrolment, by the principal investigator. The same procedure was applied to the control group, except for the mindfulness stress management technique.
Intervention consisted of an 8-week mindfulness stress management program, which included mindfulness breathing exercises and diaphragmatic breathing exercises. The mindfulness stress management program was administered in the form of an audio compact disc (CD), along with the necessary instructions by the principal investigator individually to each participant on the day of enrolment. The session lasted 30 min, during which the investigator provided advice for the implementation of the 30-min mindfulness stress management program in the daily routine once a day, usually before bedtime, for 8 weeks. Participants were monitored by the principal investigator on a weekly basis for any difficulties or concerns regarding the application of the mindfulness stress management technique.
For each study participant, a 30-min scheduled meeting or telephone call with the principal investigator was provided, depending on the availability or preference of the patients, at the end of each week, during which patients reported on their progress, the changes they had observed in the previous week and the frequency of their practice. Patients were also advised to get in touch with the investigator anytime they needed to report or discuss anything.
Objectives
The primary goal was to assess the efficacy of the mindfulness stress management program on the depression, anxiety, stress and health-related life quality levels. The secondary goal was to evaluate the impact of the placebo effect on the outcome measures.
Outcome measures
Primary outcome was the difference in depression, anxiety, stress and health-related life quality levels, before and after implementation of the mindfulness stress management program in the intervention and control groups. Secondary outcome was the impact of the placebo effect on the intervention group. Depression, anxiety, stress and health-related life quality levels were evaluated at baseline and post-intervention with the use of five questionnaires and the measurement of salivary cortisol concentrations.
The questionnaires used were the following.
1. DASS 21 (depression, anxiety, stress scales) questionnaire
The DASS 21 comprises of a set of three self-reported scales, designed to measure the perception/physical symptomatology of the negative emotional states of depression, anxiety and stress, during the past week. It includes 21 items, divided into subscales of seven items each with similar content; the depression subscale (items 3, 5, 10, 13, 16, 17 and 21), the anxiety subscale (items 2, 4, 7, 9, 15, 19 and 20) and the stress subscale (items 1, 6, 8, 11, 12, 14 and 18). It was administered in both groups. All questions are measured on a four-point Likert scale, ranging from 0 (“did not apply to me – NEVER”) to 3 (“applied to me very much, or most of the time – ALMOST ALWAYS”). It is validated in Greek language (Lyrakos et al., Citation2011).
2. PSS-14 (perceived stress scale) questionnaire
The PSS-14 includes 14 items, by which the patients can evaluate the degree of daily stress they have experienced during the past month. All questions (items) are measured on a five-point Likert scale, ranging from “never” (0) to “very often” (4). PSS-14 scores are obtained by reversing the scores on the seven positive items, e.g. 0 = 4, 1 = 3, 2 = 2, etc. and then summing across all 14 items. Items 4, 5, 6, 7, 9, 10 and 13 are the positively stated items. It was administered in both groups. It is validated in Greek language (Katsarou et al., Citation2012).
3. Routine-daily life questionnaire
The routine-daily life includes items about demographic characteristics such as age, educational level, marital status, height, weight and daily routine habits. It consists of many scales but only two were used, the “Daily Life Scale” and the “Life Satisfaction Scale”. Daily Life Scale includes 12 items about daily routine habits, which are measured on a four-point Likert scale from 1 (never) to 4 (always). Life Satisfaction Scale includes 18 items; 8 items for life satisfaction and general daily satisfaction, 5 items for relationship satisfaction and 5 items for job satisfaction. These items are also measured on a Likert scale from “extremely dissatisfied” (1) to “extremely satisfied” (5). The questionnaire was administered in both groups. It is developed in Greek language (Darviri et al., Citation2012).
4. PCOSQ (polycystic ovary syndrome health-related quality of life) questionnaire
The PCOSQ consists of 26 items, measuring five areas of health-related quality of life (HRQoL) and thus perception of difficulties concerning the experienced emotions (8 items), body hair (5 items), weight (5 items), infertility difficulties (4 items) and menstrual problems (4 items). Each item in the PCOSQ is graded with a seven-point scale ranging from 1 (maximum impairment of HRQoL) to 7 (no problems or difficulties) during the past two weeks (Jones et al., Citation2004). It was administered in both groups.
5. Credibility and expectancy questionnaire
The credibility and expectancy questionnaire is an easy-to-administer scale for assessing patient’s expectancy for treatment and rationale credibility. Credibility refers to how believable, convincing and logical the treatment is, whereas expectancy refers to improvements that patients believe that will be achieved. The aspects included in these two scales relate to (a) treatment rationale, (b) treatment satisfaction, (c) degree to which the patient would recommend the therapy to a friend with the same problem, (d) extent to which the intervention is considered to be useful in the same case and (e) extent to which the intervention would be considered aversive.
The credibility and expectancy questionnaire consists of 6 items, 4 on credibility and 2 on expectancy. Regarding the credibility questions, three are rated on a Likert-type scale from 1 to 10 and the fourth is rated from 0% to 100%. It was administered only in the intervention group and only at the time of enrolment, to check for possible placebo effect in the outcome measures (Devilly & Borkovec, Citation2000).
Salivary cortisol measurements
Diurnal saliva was collected with the use of Salivettes® (Sarstedt-Nuembrecht, Germany) three times a day for measurement of salivary cortisol concentrations; Cort1 – 8 a.m. (at rest – at awakening), Cort2 – 8.30 a.m. (30 min after waking up − at rest without employing any activity) and Cort3 – 8 p.m. (12 h post-awakening), on the day of enrolment and at the end of the 8-week period. Written and verbal instructions for use were given to patients prior to the procedure (Inder et al., Citation2012). Salivary cortisol concentrations were determined with the use of an automated electrochemiluminescence method on a COBAS e411 analyzer (Roche Diagnostics®). The area under the curve (AUC) for salivary cortisol concentrations was measured at awakening with respect to ground (AUCg) and with respect to increase (AUCi; Pruessner et al., Citation2003). Salivary cortisol AUCg is a biological indicator of negative affect and representative of the total hormonal output (Izawa et al., Citation2010) whereas AUCi is a biological indicator that provides information on the HPA axis reactivity (Fekedulegn et al., Citation2007).
Sample size
As this was a pilot study implementing a mindfulness stress management program in reproductive age women with PCOS in Greece, we aimed at a number of participants between 12 (Julious, Citation2005) and 25 (Sim & Lewis, Citation2012) per group.
Statistical analyses
Statistical analyses were performed using the statistical software package IBM SPSS version 21.0 (IBM. Co., New York, NY) and StatSoft Statistica version 8. Baseline, descriptive characteristics are represented as mean values, standard deviation (SD), absolute (n) and proportional values (%). Statistical significance was set at p < 0.05. Cohen’s d effect sizes were also calculated to serve as a quantitative measure of the strength of our findings. The normality of data was assessed with the Shapiro–Wilk test and normal probability plots (Q–Q plots, P–P plots). Intention to treat analysis (Hollis & Campbell, Citation1999) was used, along with multiple imputations of the missing values. Statistical tests were performed between imputed and observed values to check for statistical differences (Sterne et al., 2009). Statistical analysis was performed using the Pearson χ2 for frequency group comparisons, the independent two-sample Student t-test for mean differences between the groups, the paired Student t-test for mean differences within the groups, the Pearson correlation coefficient (r) and repeated measures ANOVA followed by Bonferroni correction, to explore the impact of group assignment on the Life Satisfaction Scale scoring. The reliability of a scale can vary depending on the sample that it is used with. Therefore, we considered necessary to check that each scale used in this study was reliable within our sample. Consequently, we performed Cronbach alpha co-efficient analysis for every scale and subscale used, to assess internal consistency (Streiner & Norman, Citation1995). Multiple stepwise regression analysis was used to test if the baseline characteristics significantly predicted the outcome measures.
Results
Participant flow
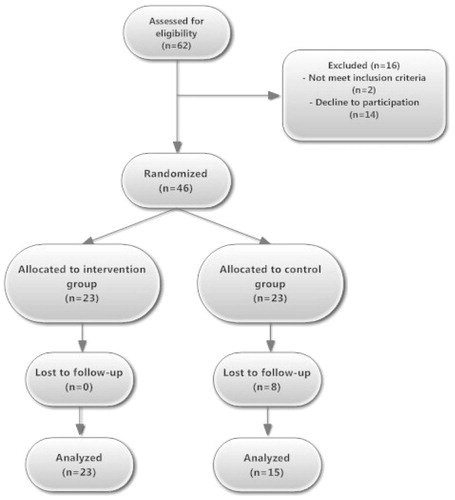
During a 7-month period, 69 women were screened for eligibility and 46 women who met the Rotterdam diagnostic criteria for PCOS were considered eligible. Of these, eight women were excluded after randomization, as they were considered as drop-outs. Consequently, a total of 23 PCOS patients were allocated to the intervention group and 15 to the control group (attrition rate 35% in the control group). The participants’ flow chart is shown in .
Baseline characteristics
Patient characteristics at enrolment are demonstrated in . There were no significant differences between the two groups for the majority of characteristics apart from total life satisfaction and its subscale, general satisfaction scores. Since the assumption of sphericity, normality and minimum sample requirement were satisfied, a linear, mixed between groups analysis of variance was conducted to explore the impact of the initial group assignment on general life satisfaction (p < 0.001) and total life satisfaction (p = 0.01) scores. There were statistically significant main effects for group assignment (Wilk’s Lambda = 0.89, F[1, 36] = 4.440, p = 0.021, partial η2 = 0.11) and the effect size was small. The main effect for group assignment (Wilk’s Lambda = 0.65, F [1, 36] = 5.83, p = 0.021) was also medium (partial η2 = 0.139). The main effects for time and group assignment also differed significantly (Wilk’s Lambda = 0.026, F [1, 36] = 11, p = 0.02, partial η2 = 0.235). These effect sizes might be attributed to the control group’s disappointment over group assignment. Other reasons might be cultural or even a result of different personality traits (Diener et al., 2012; Takeuchi et al., 2014).
Table 1. Baseline and post-intervention data (demographic and clinical characteristics, questionnaire scoring and salivary cortisol data) of study participants.
Outcomes
Results of study questionnaires’ internal consistency are demonstrated in . All the questionnaires and their subscales demonstrated satisfactory Cronbach alpha co-efficients, except for the emotions subscale of PCOSQ and the credibility and expectancy questionnaire. Cronbach alpha co-efficient is very sensitive to the number of items in the scale. Since the recommended range of these short scales’ items correlation co-efficient is between 0.2 and 0.4 (Briggs & Cheek, 1986), we considered this scale reliable for this study.
Table 2. Cronbach alpha coefficients for study questionnaires’ internal consistency.
Between-groups results post-intervention
Post-intervention results showed significant differences between the intervention and control groups in DASS21 depression [t(36) = −4.879, Cohen’s d = −1.72, p = 0.011] and stress subscales [t(36) = −5.540, Cohen’s d = −1.90, p = 0.025] and in Cort1 [t(36) = −2.702, Cohen’s d = −2.94, p = 0.001] and Cort2 [t(36) = −2.751, Cohen’s d = −2.65, p = 0.025] as shown in . No other statistically significant differences were observed between the two groups. Multiple stepwise regression analysis was used to test if the baseline characteristics (age, BMI, marital status, educational level, residence, hormonal profile, FG score and medication) significantly predicted participants' scores of DASS21 depression and stress subscales, Cort1 and Cort2 concentrations. No statistically significant predictors were found for DASS21 depression and stress subscales’ scores and for Cort1 concentrations. For the study participants who were on metformin, baseline BMI was the best predictor for Cort2, which explained 61.2% of the Cort2 variance [R2 = 0.58, F(1,17) = 26.8, SE = 1.12, p < 0.01]. In these patients, baseline BMI significantly predicted Cort2 concentrations [β = 0.38, SEβ = 0.07, t(17) = 5.181, p < 0.001]. For women who were not on medication, age was found to be the best predictor for Cort2, which explained 48.7% of the Cort2 variance [R2 = 43.6%, F(1,10) = 9.51, SE = 1.99, p = 0.01]. In these women, age significantly predicted Cort2 concentrations [β = 0.30, SEβ = 0.10, t(10) = 3.084, p < 0.011].
Intervention group results
Statistically significant differences pre- and post-intervention were demonstrated for DASS 21 depression [t(22) = 3.557, 95% CI = 1.66, 6.33, Cohen’s d = 3.496, p = 0.002], anxiety [t(22) = 3.806, 95% CI = 1.74, 5.91, Cohen’s d = 1.462, p = 0.001] and stress [t(22) = 5.496, 95% CI = 4.38–9.7, Cohen’s d = 1.608, p < 0.001] subscales, along with the PCOSQ perception subscales [Emotions – t(21) = −3.211, 95% CI = −8.9, −1.9, Cohen’s d = −0.765, p = 0.004, body hair – t(21) = −3.687, 95% CI = −5.9, −1.6, Cohen’s d = −0.848, p = 0.001, weight – t(20) = −2.720, 95% CI = −6.05, −0.79, Cohen’s d = −0.670, p = 0.013, infertility – t(22) = −3.067, 95% CI = −5.02, −0.97, Cohen’s d = −0.693, p = 0.006, menstrual problems – t(22) = −3.180, 95% CI = −5.6, −1.17, Cohen’s d = −0.664, p = 0.004] and the general satisfaction subscale of daily routine questionnaire [t(22) = −3.557, 95% CI = −3.14, −0.77, Cohen’s d = −0.772, p = 0.002]. AUCg decreased significantly post-intervention [t(22) = 2.493, 95% CI = 1.64, 17.91, Cohen’s d = 3.834, p = 0.037]. Interestingly, no significant differences were observed in salivary cortisol levels, PSS-14 scores, daily routine questionnaire scores and job satisfaction or relationships satisfaction scores, before and after the intervention. Multiple stepwise regression analysis indicated no statistically significant predictors for the intervention group’s outcome measures.
The mean frequency of technique application was 35.86 (SD = 13.9, Min = 17, Max = 56). The 8-week period of the intervention sums up to 56 times, in total. There was statistically significant deviation from the expected frequency of technique application [t(21) = −6.79, 95% CI = −26.3, −13.96, p < 0.001]. However, the frequency of the technique application was not found to be significantly correlated with most of the results. The correlation and the regression co-efficients of the technique application frequency with the outcome measures are demonstrated in . Of all the questionnaires and subscales, only the body hair and the Weight perception subscale of the PCOSQ, the daily routine and the general satisfaction subscales of the routine-daily life questionnaire were significantly correlated with the frequency of technique application.
Table 3. Correlation and linear regression coefficients of the technique application frequency and the outcome measures in the Intervention Group.
Regarding the credibility and expectancy questions, the last question of the first section (confidence in recommending therapy to a friend) and the two items of the second section (success in reducing symptoms, expectancy scale) did not demonstrate correlation with any of the baseline characteristics or the outcome measures (before and after the intervention), suggesting that the placebo effect did not have any significant influence on the intervention group’s results.
Control group results
DASS 21 depression [t(14) = −2.371, 95% CI = −6.09, −0.305, 2.97, Cohen’s d = 0.166, p = 0.033] and anxiety [t(14) = −2.588, 95% CI = −5.60, −0.52, Cohen’s d = −0.739, p = 0.021] subscales along with PCOSQ emotions [t(14) = 4.257, 95% CI = 2.08, 6.31, Cohen’s d = 1.38, p = 0.001], body hair [t(14) = 2.595, 95% CI = 0.42, 4.5, Cohen’s d = 0.671, p = 0.021) and menstrual problems [t(13) = 2.459, 95% CI = 0.19, 3.08, Cohen’s d = 0.699, p = 0.029) perception subscales were the only outcome measures that significantly differed before and after the 8-week period of the trial. Multiple stepwise regression analysis indicated no statistically significant predictors for the control group’s outcome measures.
Adverse events
No adverse effects were noted in either group. Conversely, participants’ guardians or life partners commented on improvement of their demeanor and general behavior post-intervention.
Discussion
This study aimed to explore the impact of a mindfulness stress management intervention program on stress and other aspects of health-related quality of life in PCOS patients of reproductive age. Our findings confirmed that stress, anxiety and depression levels decreased and life quality improved with the intervention in these patients.
More specifically, DASS 21 anxiety, depression and stress subscales scores decreased significantly with mindfulness stress management. These results are similar to those of other studies, were statistically significant reductions in all three DASS 21 subscales were observed after implementation of mindfulness in different groups of patients (Gold et al., Citation2010). Regarding the PCOSQ questionnaire scores, the intervention group’s results also showed a significant improvement in almost all of its subscales, findings analogous to the results of other mindfulness stress management programs RCTs in breast cancer patients (Henderson et al., Citation2012; Hoffman et al., Citation2012).
We demonstrated that a statistically significant reduction in AUCg post-intervention which has been associated with a reduction of negative affect and, consequently, with decreases of stress perception (Piazza et al., Citation2013). The augmentation in the general satisfaction subscale score after intervention in our PCOS patients, confirmed the above associations.
The pathophysiology of cortisol signaling in women with PCOS is poorly understood (Milutinovic et al., Citation2011). Interestingly, we found that age was the best predictor for Cort2 only in patients who were not receiving medical treatment for their PCOS and probably represented the milder form of the syndrome. In normal women, cortisol levels may increase with age due to an increased activity of the HPA axis consistent with lifelong exposure to stress (Van Cauter et al., Citation1996). Baseline BMI was the best predictor for Cort2 only in those women who received metformin. These data probably support a role of increased HPA axis activity and elevated cortisol levels in the expression of worse metabolic PCOS phenotype in those women in need of metformin.
PSS-14 questionnaire scoring, which evaluates perceived stress levels, did not demonstrate statistically significant differences within or between groups post-intervention. However, according to the AUCg and the DASS 21 stress subscale scoring, it seems that in PCOS patients stress was indeed reduced. DASS21 stress subscale principally evaluates sympathetic nervous system symptomatology and not perceived stress, which patients experience subjectively. This finding is consistent with a recent study indicating that mindfulness techniques exert their beneficial effects primarily through direct remodeling of neural correlates, suggesting that the primary effect of mindfulness stress management may be mostly exerted in affect rather than in cognition (Kerr et al., Citation2013). Thus, it is possible that a longer duration of this particular intervention would help the patients to experience the benefits of this program more profoundly. Also, other experimental studies (Paredes et al., 1998) have shown that in PCOS patients, sympathetic nervous system tone is up-regulated, suggesting that the relaxation response cannot be easily achieved (de Sá et al., Citation2011; Yildirir et al., Citation2006).
We also attempted to evaluate the impact of the placebo effect, via the credibility and expectancy questionnaire. There is a methodological “battle” in the medical literature about how the placebo effect impacts on the results of RCTs. It seems that the “clinically important effects” are an integrating aspect of not only pharmacological RCTs (Kirsch, Citation2005), but also of complementary medicine RCTs, such as ours. It is, therefore, exceptionally difficult to interpret the results of a RCT, without evaluating the perceptions and notions of the participants and the expectancy and credibility of the intervention. According to our results, there was no impact of the credibility and/or expectancy notions, and hence, a placebo effect is unlikely.
Our study had some limitations. As it was not feasible to conduct a “placebo intervention”, the control group did not receive any program, and no concealment was used. Furthermore, with respect to intervention, we could not objectively validate the frequency of the technique application, since it was self-reported. We only assessed the effects of the mindfulness stress management program at the end of the 8-week period. Although the frequency of the technique application was of significance in other studies, this was not confirmed in this study, since it was not substantially correlated with the outcome. Maybe the duration of this particular technique application is of importance; it would be of interest to follow up these patients for longer periods and check for long-lasting effects of mindfulness stress management in their lives.
Our trial adds to the cumulative evidence, which supports the adaptation of mindfulness techniques for reduction of stress, anxiety and depression in several conditions (Klainin-Yobas et al., Citation2012). We conclude that mindfulness techniques are promising in reducing stress and ameliorating the quality of life in women with PCOS. Future studies in a larger number of patients and for a longer follow-up period are needed to allow definite conclusions.
Conclusions
We conducted a randomized controlled trial to evaluate the effect of a mindfulness stress management program on stress, anxiety and depression in women with PCOS. Mindfulness stress management techniques could be used as an adjunct method to conventional treatment for women with polycystic ovary syndrome.
Declaration of interest
The authors report no conflicts of interest. Salivary cortisol devices and measurements were funded by the Medical School and the First Department of Pediatrics of the National & Kapodistrian University of Athens in Greece.
Acknowledgements
The authors would like to thank the research fellow, Mr. Vasileios Pliatskas, for the masking procedure, Dr. Maria Drakopoulou for the measurements of cortisol concentrations and Professor Christina Darviri for giving permission to use the Routine-Daily Life questionnaire.
References
- Benson S, Arck PC, Tan S, Hahn S, Mann K, Rifaie N, Janssen OE, et al. (2009). Disturbed stress responses in women with polycystic ovary syndrome. Psychoneuroendocrinology 34(5):727–35
- Bhasin MK DJ, Chang BH, Joseph MG, Denninger JW, Fricchione GL, Benson H, Libermann TA. (2013). Relaxation response induces temporal transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways. PLoS One 8:e62817
- Brand S, Holsboer-Trachsler E, Naranjo JR, Schmidt S. (2012). Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology 65(3):109–18
- Brewer JA WP, Gray JR, Tang YY, Weber J, Kober H. (2011). Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci USA 108(50):20254–9
- Briggs SR, Cheek JM. (1986). The role of factor analysis in the development and evaluation of personality scales. J Person 54(1):106–48
- Costello MF, Misso ML, Wong J, Hart R, Rombauts L, Melder A, Norman RJ, Teede HJ. (2012). The treatment of infertility in polycystic ovary syndrome: a brief update. Aust NZJ Obstet Gynaecol 52(4):400–3
- Darviri C, Fouka G, Gnardellis C, Artemiadis AK, Tigani X, Alexopoulos EC. (2012). Determinants of self-rated health in a representative sample of a rural population: a cross-sectional study in Greece. Int J Environ Res Public Health 9(3):943–54
- de Sa JC, Costa EC, da Silva E, Zuttin RS, da Silva EP, Lemos TM, De Azevedo GD. (2011). Analysis of heart rate variability in polycystic ovary syndrome. Gynecol Endocrinol 27(6):443–7
- Devilly GJ, Borkovec TD. (2000). Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 31(2):73–86
- Diamanti-Kandarakis E, Kouli CR, Bergiele AT, Filandra FA, Tsianateli TC, Spina GG, Zapanti ED, Bartzis MI. (1999). A survey of the polycystic ovary syndrome in the Greek island of Lesbos: hormonal and metabolic profile. J Clin Endocrinol Metab 84(11):4006–11
- Diener E, Inglehart R, Tay L. (2012). Theory and validity of life satisfaction scales. Soc Indic Res 112(3):497–527
- Dokras A. (2012). Mood and anxiety disorders in women with PCOS. Steroids 77(4):338–41
- Fekedulegn DB, Andrew ME, Burchfiel CM, Violanti JM, Hartley TA, Charles LE, Miller DB. (2007). Area under the curve and other summary indicators of repeated waking cortisol measurements. Psychosom Med 69(7):651–9
- Gold ESA, Hopper I, Herne D, Tansey G, Hulland C. (2010). Mindfulness-based stress reduction (MBSR) in primary school teachers. J Child Fam Stud 19:184–9
- Henderson VP, Clemow L, Massion AO, Hurley TG, Druker S, Hebert JR. (2012). The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Res Treat 131(1):99–109
- Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW. (2012). Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol 30(12):1335–42
- Hollis S, Campbell F. (1999). What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 319(7211):670–4
- Holzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T, Lazar SW. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res 191(1):36–43
- Inder WJ, Dimeski G, Russell A. (2012). Measurement of salivary cortisol in 2012 – laboratory techniques and clinical indications. Clin Endocrinol (Oxf) 77(5):645–51
- Izawa S, Sugaya N, Yamamoto R, Ogawa N, Nomura S. (2010). The cortisol awakening response and autonomic nervous system activity during nocturnal and early morning periods. Neuro Endocrinol Lett 31(5):685–9
- Jones GL, Benes K, Clark TL, Denham R, Holder MG, Haynes TJ, Mulgrew NC, et al. (2004). The Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ): a validation. Hum Reprod 19(2):371–7
- Julious SA. (2005). Sample size of 12 per group rule of thumb for a pilot study. Pharmaceut Stat 4:287–91
- Katsarou A, Panagiotakos D, Zafeiropoulou A, Vryonis M, Skoularigis I, Tryposkiadis F, Papageorgiou C. (2012). Validation of a Greek version of PSS-14; a global measure of perceived stress. Cent Eur J Public Health 20(2):104–9
- Kerr CE, Sacchet MD, Lazar SW, Moore CI, Jones SR. (2013). Mindfulness starts with the body: somatosensory attention and top-down modulation of cortical alpha rhythms in mindfulness meditation. Front Hum Neurosci 7:12
- Kilpatrick LA, Suyenobu BY, Smith SR, Bueller JA, Goodman T, Creswell JD, Tillisch K, Mayer EA, Naliboff BD. (2011). Impact of mindfulness-based stress reduction training on intrinsic brain connectivity. Neuroimage 56(1):290–8
- Kirsch I. (2005). Placebo psychotherapy: synonym or oxymoron? J Clin Psychol 61(7):791–803
- Klainin-Yobas P, Cho MA, Creedy D. (2012). Efficacy of mindfulness-based interventions on depressive symptoms among people with mental disorders: a meta-analysis. Int J Nurs Stud 49(1):109–21
- Krepula K, Bidzinska-Speichert B, Lenarcik A, Tworowska-Bardzinska U. (2012). Psychiatric disorders related to polycystic ovary syndrome. Endokrynol Pol 63(6):488–91
- Kubota Y, Sato W, Toichi M, Murai T, Okada T, Hayashi A, Sengoku A. (2001). Frontal midline theta rhythm is correlated with cardiac autonomic activities during the performance of an attention demanding meditation procedure. Brain Res Cogn Brain Res 11(2):281–7
- Lansdown A, Rees DA. (2012). The sympathetic nervous system in polycystic ovary syndrome: a novel therapeutic target? Clin Endocrinol (Oxf) 77(6):791–801
- Lyrakos GN, Arvaniti C, Smyrnioti M, Kostopanagiotou G. (2011). Translation and validation study of the depression anxiety stress scale in the Greek general population and in a psychiatric patient's sample. Eur Psychiatry 26:1731
- Mansson M, Norstrom K, Holte J, Landin-Wilhelmsen K, Dahlgren E, Landen M. (2011). Sexuality and psychological wellbeing in women with polycystic ovary syndrome compared with healthy controls. Eur J Obstet Gynecol Reprod Biol 155(2):161–5
- Milutinovic DV, Macut D, Bozic I, Nestorov J, Damjanovic S, Matic G. (2011). Hypothalamic-pituitary-adrenocortical axis hypersensitivity and glucocorticoid receptor expression and function in women with polycystic ovary syndrome. Exp Clin Endocrinol Diabetes 119(10):636–43
- Paredes A, Gálvez A, Leyton V, Aravena G, Fiedler JL, Bustamante D, Lara HE. Stress promotes development of ovarian cysts in rats: the possible role of sympathetic nerve activation. Endocrine 1998;8:309–15
- Piazza JR, Charles ST, Stawski RS, Almeida DM. (2013). Age and the association between negative affective states and diurnal cortisol. Psychol Aging 28(1):47–56
- Praissman S. (2008). Mindfulness-based stress reduction: a literature review and clinician's guide. J Am Acad Nurse Pract 20(4):212–6
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology 28(7):916–31
- Raja-Khan N, Stener-Victorin E, Wu X, Legro RS. (2011). The physiological basis of complementary and alternative medicines for polycystic ovary syndrome. Am J Physiol Endocrinol Metab 301(1):E1–10
- Robins CJ, Keng SL, Ekblad AG, Brantley JG. (2012). Effects of mindfulness-based stress reduction on emotional experience and expression: a randomized controlled trial. J Clin Psychol 68(1):117–31
- Rosenzweig S RD, Greeson JM, Edman JS, Jasser SA, McMearty KD, Goldstein BJ. (2007). Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med 13:36–8
- Roth LW, Huang H, Legro RS, Diamond MP, Coutifaris C, Carson SA, Steinkampf MP, et al. (2012). Altering hirsutism through ovulation induction in women with polycystic ovary syndrome. Obstet Gynecol 119(6):1151–6
- Sim J, Lewis M. (2012). The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 65(3):301–8
- Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. (2009). Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338:b2393
- Streiner DL, Norman GR. (1995). Health measurement scales: a practical guide to their development and use. 2nd ed. Oxford: Oxford University Press
- Sundbom LT, Bingefors K. (2013). The influence of symptoms of anxiety and depression on medication nonadherence and its causes: a population based survey of prescription drug users in Sweden. Patient Prefer Adherence 7:805–11
- Takeuchi H, Taki Y, Nouchi R, Hashizume H, Sassa Y, Sekiguchi A, Kotozaki Y, et al. (2014). Anatomical correlates of quality of life: evidence from voxel-based morphometry. Hum Brain Mapp 35(5):1834–46
- Turakitwanakan W, Mekseepralard C, Busarakumtragul P. (2013). Effects of mindfulness meditation on serum cortisol of medical students. J Med Assoc Thai 96:S90–5
- Van Cauter E1, Leproult R, Kupfer DJ. (1996). Effects of gender and age on the levels and circadian rhythmicity of plasma cortisol. J Clin Endocrinol Metab 81(7):2468–73
- Yildirir A, Aybar F, Kabakci G, Yarali H, Oto A. (2006). Heart rate variability in young women with polycystic ovary syndrome. Ann Noninvasive Electrocardiol 11(4):306–12