In this issue of Leukemia and Lymphoma, Mussetti and colleagues report on a single patient with well-documented myelomatous meningitis that responded to pomalidomide, having failed transplant and multiple novel agents [Citation1]. Myelomatous involvement of the central nervous system can occur in two forms. The first is an intracerebral plasmacytoma. Most frequently, these result from osseous lesions in the cranial vault, such as the base of the skull, sphenoid wing, nose or paranasal sinuses. These solitary plasmacytomas of bone with extension into the brain are treatable with external beam radiation therapy, do not necessarily represent progression in a sanctuary site, and do not carry the poor prognosis of myelomatous meningitis [Citation2].
Myelomatous meningitis is diagnosed by detecting plasma cells in the spinal fluid associated with elevation in cerebrospinal fluid protein, and reduction in sugar. Myeloma meningitis is recognized in 1% of patients with multiple myeloma. Most reports are single patients with a few patient series. One can expect patterns of myeloma relapse to change as patients live longer. With the introduction of novel drugs, the frequency of extramedullary myeloma is increasing. The longer survival allows for an increased frequency of mutations in genomic DNA with increased activation of oncogenes, deletion of tumor suppressor genes and changes in adhesion receptors. One might anticipate an increase in the frequency of central nervous system (CNS) myeloma as effective therapies continue to be developed.
The blood–brain barrier creates a sanctuary site in multiple myeloma since the chemotherapy agents currently used will not cross it. The current standard of care is intrathecal chemotherapy, and combinations of methotrexate, cytarabine and intrathecal steroids have all been used, as has craniospinal radiation [Citation3]. A 6-month neural progression- free survival rate of 7% has been reported. Although the diagnosis is established histopathologically, magnetic resonance imaging can demonstrate meningeal enhancement consistent with leptomeningitis [Citation4]. Using involved field radiotherapy to the spine and intraspinal chemotherapy, the largest case series of 14 patients reported six partial responses and eight therapy failures. The median response duration was 2.5 months. The median overall survival was 4 months, and none of the patients survived beyond 8 months. Toxicity associated with spinal radiotherapy and intrathecal therapy includes arachnoiditis in 50% and fatigue [Citation5]. Myelomatous meningitis has occurred in the face of allogeneic transplant, reflecting the central nervous system's ability to create a sanctuary from alloreactive T-cells that could recognize the malignant clone as non-self [Citation6].
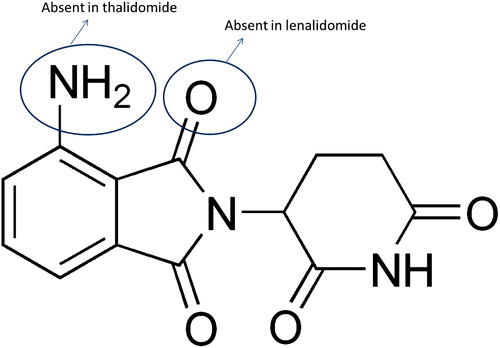
New strategies to manage CNS myeloma are warranted. Pomalidomide is a third-generation immunomodulatory agent that is anti-angiogenic, has a molecular weight of 273, and is water soluble (). The immunomodulatory effect is due to inhibition of tumor necrosis factor-α (TNF-α). Pomalidomide enhances antibody-dependent cellular cytotoxicity. Mole for mole, pomalidomide is 100 times more potent than thalidomide and 10 times more potent than lenalidomide. Pomalidomide plus low-dose dexamethasone has been used for relapsed multiple myeloma at a dose of 2 mg daily days 1 through 28 with weekly dexamethasone, 40 mg. Thirty-eight of 60 patients (63%) achieved a confirmed response, which was complete in 5%, a very good partial response (VGPR) in 28%, and partial response (PR) in 30%. Responses were seen in 40% of lenalidomide refractory patients, 37% of thalidomide refractory patients and 60% of bortezomib refractory patients. There was one thromboembolic event and a progression-free survival of 11.6 months [Citation7]. In a trial enrolling only lenalidomide refractory patients, pomalidomide at 2 mg daily with weekly dexamethasone was given to 34 patients with an overall response rate of 47% (three VGPR, eight PR and five minor response [MR]). In patients classified as having high-risk disease, the response rate was 57% (eight of 14). The median response duration was 9.1 months. Toxicity was primarily hematologic [Citation8].
Pomalidomide has been used in the presence of extramedullary disease. In a trial including 13 patients with extramedullary disease, there were two complete and two partial responses (31%). Survival was shorter for patients with treatment-emergent extramedullary disease, median 16 months. This encouraging activity of pomalidomide in extramedullary disease would make its use in myelomatous meningitis logical [Citation9]. Pomalidomide in patients who were refractory to both bortezomib and lenalidomide enrolled 35 patients, each in cohorts receiving 2 and 4 mg daily. The overall response rate was 49% (14% VGPR, 11% PR and 23% MR) at 2 mg. In the 4 mg cohort, the overall response rate was 43%. Overall survival at 6 months was 78 and 67%, respectively, in the 2 and 4 mg cohorts. Myelosuppression was the most common toxicity [Citation10].
New drug development in multiple myeloma is proceeding at a rapid rate and offers hope for our patients. In addition to pomalidomide, carfilzomib, a tetrapeptide epoxyketone proteasome inhibitor, was approved by the United States Food and Drug Administration (FDA) on 1 August for patients with myeloma who had received at least two prior therapies, including both bortezomib and thalidomide or lenalidomide. The anti-CS1 antibody elotuzumab shows no single agent activity, but appears to be active when combined with bortezomib or lenalidomide. Oral proteasome inhibitors are enrolling patients with myeloma. Bendamustine is an agent being studied in myeloma, currently approved for the treatment of chronic lymphocytic leukemia and indolent B-cell non-Hodgkin lymphoma that has progressed within 6 months of treatment with rituximab or a rituximab-containing regimen. Histone deacetylase (HDAC) inhibitors, when combined with a proteasome inhibitor, can result in the excessive buildup of misfolded proteins leading to apoptosis. Both vorinostat and panobinostat have been studied for their activity with bortezomib in multiple myeloma. Currently, median survivals in patients with myeloma are approaching 7–8 years. We can anticipate breaking the 10-year barrier shortly.
Supplementary Material
Download Zip (424.2 KB)Potential conflict of interest:
A disclosure form provided by the author is available with the full text of this article at www.informahealthcare.com/lal.
References
- Mussetti A, Dalto S, Montefusco V. Effective treatment of pomalidomide in central nervous system myelomatosis. Leuk Lymphoma 2013;54;864–866.
- Cerase A, Tarantino A, Gozzetti A, . Intracranial involvement in plasmacytomas and multiple myeloma: a pictorial essay. Neuroradiology 2008;50:665–674.
- Lopes da Silva R, Costa I, Prata M, . Plasma cell meningitis: a rare neurological complication of multiple myeloma requiring a high index of suspicion. Acta Neurol Taiwan 2011;20:209–212.
- Licci S, Narciso P. Myelomatous meningitis. Eur J Haematol 2008;81:328.
- Chamberlain MC, Glantz M. Myelomatous meningitis. Cancer 2008;112:1562–1567.
- Savage DG, Mears JG, Balmaceda C, . Leptomeningeal relapse of multiple myeloma following allogeneic stem cell transplantation. Leuk Res 2002;26:689–692.
- Lacy MQ, Hayman SR, Gertz MA, . Pomalidomide (CC4047) plus low-dose dexamethasone as therapy for relapsed multiple myeloma. J Clin Oncol 2009;27:5008–5014.
- Lacy MQ, Hayman SR, Gertz MA, . Pomalidomide (CC4047) plus low dose dexamethasone (pom/dex) is active and well tolerated in lenalidomide refractory multiple myeloma (MM). Leukemia 2010; 24:1934–1939.
- Short KD, Rajkumar SV, Larson D, . Incidence of extramedullary disease in patients with multiple myeloma in the era of novel therapy, and the activity of pomalidomide on extramedullary myeloma. Leukemia 2011;25:906–908.
- Lacy MQ, Allred JB, Gertz MA, . Pomalidomide plus low-dose dexamethasone in myeloma refractory to both bortezomib and lenalidomide: comparison of 2 dosing strategies in dual-refractory disease. Blood 2011;118:2970–2975.