Robert K. Heaton1, Lucette A. Cysique1, Hua Jin1,2, Chuan Shi3, Xin Yu3, Scott Letendre1, Donald R. Franklin Jr 1, Christopher Ake1, Ofilio Vigil1, J. Hampton Atkinson1, Thomas D. Marcotte1, Igor Grant1, Zunyou Wu4, and the HNRC group.
1HIV Neurobehavioral Research Center (HNRC), Department of Psychiatry, University of California at San Diego, San Diego, California; 2VA San Diego Health Care System, San Diego, California; 3Institute of Mental Health, Peking University, Beijing, China; and 4National Center for AIDS/STD Control & Prevention (NCAIDS), China
This corrigendum concerns the following article published in the Journal of Neurovirology: Heaton RK, Cysique LA, Jin H, et al: Neurobehavioral effects of human immunodeficiency virus infection among former plasma donors in rural China. Journal of Neurovirology, 7:1-14, 2008. In this article we reported that 26% of the HIV uninfected (HIV-) sample and 46% of the HIV infected (HIV+) sample were also infected with the Hepatitis C virus (HCV).
Recently we discovered that there was a change in the laboratory personnel at the China CDC during the first year of data collection. The new person made a systematic transcription error when processing the hepatitis and liver panel data. This error resulted in an underestimation of HCV prevalence in our samples. The new (corrected) rates of HCV infection are as follows: 62.5% of the HIV- sample and 93% of the HIV+ sample were infected with HCV (p = .001).
The revised provides extended demographic information about the four reconstituted groups. There was a trend for a greater proportion of males in the uninfected control group, and the HIV/HCV coinfected group had many more prior plasma donations (and associated increased infection risk) than all other groups. Otherwise, the four groups were comparable with respect to age, ethnicity, and educational, family, linguistic, employment and rural living backgrounds.
Table 1 Extended demographic characteristics of Controls, HCV monoinfected HIV monoinfected and co-infected- groups
compares the HIV disease history and treatment characteristics of our two HIV infected groups. These groups were quite comparable in terms of distribution of CDC stages, as well as current and nadir CD4 cell counts and percent receiving ARV treatment. However, participants in the correctly constituted HIV monoinfected group had a longer duration of HIV infection, and those who were receiving ART were less likely to be on HAART regimens and had regimens with lower CNS Penetration Effectiveness (CPE) ranks. These differences were not seen in the original HIV infected groups that were classified on the basis of incorrect HCV information, and potentially could place the HIV monoinfected group at greater risk for CNS injury than their coinfected counterparts (Cysique et al, Citation2009; Tozzi et al, Citation2009; Letendre et al, Citation2008).
Table 2 Clinical and laboratory characteristics in the HIV monoinfected and coinfected groups
A central issue was whether the previously reported HIV effect on neurocognitive functioning was changed by the revised HCV prevalence rates. We found that it was not: the results concerning the effects of HIV infection on neuropsychological (NP) functioning remain highly significant. Although we were not able to detect an HCV effect in our HIV+ sample (37% impairment in the coinfected group vs. 36% impairment in the HIV monoinfected group; p = .92), a modest effect of HCV on NP functioning was evident in the HIV- control sample: Using the Global NP summary score, as described in our report, NP impairment was found in 23.3% of the HCV monoinfected group, vs. only 12.5% of controls uninfected with either virus (p = .06).
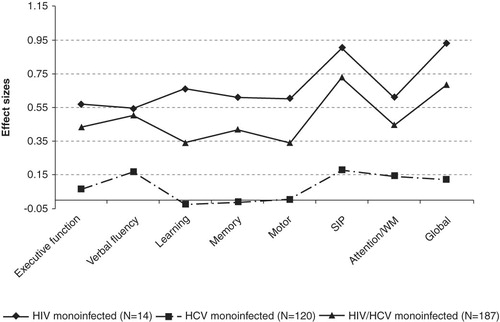
The new and provide details of the NP comparisons of the three infected groups with the uninfected controls. As reported in the original publication, both HIV infected groups evidenced substantial impairment across all ability domains. The somewhat larger effect for the HIV monoinfected than the coinfected group was not anticipated, but could relate to the above mentioned differences in ARV regimens for these two groups. Although the HCV monoinfected group evidenced some increased impairment versus controls on the NP summary score (23.3% vs. 12.5%), this rather subtle difference was not as apparent on the individual NP tests and ability domains ( and ). As reported in the original article, HIV+ former plasma donors with more advanced HIV disease (AIDS, n = 114) evidenced a significantly higher rate of NP impairment than those with less advanced disease (non-AIDS; n = 89) (43% vs. 29.2%; p < .05).
Table 3 Raw scores and effect sizes on individual NP test measures
Figure 1 Effect sizes on ability domains (Mean domain T-scores) and the total test battery (Global Mean T-scores) for infected groups as compared to 72 controls
shows that, after the groups were reconstituted with the correct HCV status, only the HIV monoinfected and coinfected groups reported increased unemployment. Also the coinfected group reported increased cognitive difficulties in everyday functioning, and a trend towards decreased independence in instrumental activities of daily living (IADLs). As stated in the original article, in the three infected groups combined, NP impairment was significantly associated with cognitive complaints and reduced independence in IADLs.
Table 4 Cognitive complaints, IADL dependence and employment in controls, HCV monoinfected, HIV monoinfected, and coinfected groups
References
- Cysique LA, Vaida F, Letendre S, Gibson S, Cherner M, Woods SP, McCutchan JA, Heaton RK, Ellis RJ (2009). Dynamics of cognitive change in impaired HIV+ individuals initiating antiretroviral therapy. Neurology 73:342–348
- Letendre S, Marquie-Beck J, Capparelli E, Best B, Clifford D, Collier AC, Gelman BB, McArthur JC, McCutchan JA, Morgello S, Simpson D, Grant I, Ellis RJ; and the CHARTER Group (2008). Validation of the CNS Penetration-Effectiveness rank for quantifying antiretroviral penetration into the central nervous system. Arch Neurol. 65:65–70.
- Tozzi V, Balestra P, Salvatori MF, Vlassi C, Liuzzi G, Giancola ML, Giulianelli M, Narciso P, Antinori AJ (2009). Changes in cognition during antiretroviral therapy: comparison of 2 different ranking systems to measure antiretroviral drug efficacy on HIV-associated neurocognitive disorders. Acquir Immune Defic Syndr. 52:56–63. Erratum in: J Acquir Immune Defic Syndr. 52: 529.
