Abstract
Objective: This study assessed the efficacy and safety of testosterone replacement therapy (TRT) in aging Japanese men with late-onset hypogonadism (LOH).
Methods: This study included 50 (median age: 57.7 years) Japanese men with LOH, who were consecutively enrolled and treated with TRT for at least six months at our institution. We evaluated the following measurements before and after six months of treatment with TRT as follows: blood tests, prostate volume, residual urine volume, self-ratings for International Index of Erectile Function 5 (IIEF-5), International Prostate Symptom Score (IPSS), Self-Rating Depression Scale (SDS), Aging Male Symptom (AMS) and the Medical Outcomes Study 8-item Short-Form health survey (SF-8).
Results: Following six months of TRT, the levels of testosterone, red blood cells, hemoglobin and hematocrit were significantly increased from baseline, while total cholesterol level was significantly decreased from baseline. Furthermore, TRT led to a significant increase in IIEF-5 score and a significant decrease in IPSS score. Of 30 men who were diagnosed with depression at baseline, only 11 men (36.7%) were still suffering from depression after TRT, and SDS scores were significantly decreased from baseline at month six. Treatment with TRT led to a significant decrease in all scores of the AMS scale as well as a significant improvement in all scores of the SF-8 survey, with the exception of the bodily pain score.
Conclusion: These findings suggest that TRT is an effective and safe treatment for aging Japanese men with LOH. TRT improved depressive symptoms as well as health-related quality of life.
Introduction
The population is aging worldwide, which is leading to an increase in the incidences of many age-related healthcare problems. While female menopause is well studied, androgen deficiency of the aging male remains poorly understood [Citation1]. Serum total testosterone and free testosterone levels decline with age in males by 0.8% and about 2% per year, respectively [Citation2]. Low testosterone has been shown to be a predictor of mortality in aging men [Citation3,Citation4]. Low testosterone levels appear to be associated with common diseases, such as hypertension, hypercholesterolemia, type 2 diabetes mellitus, ischemic heart disease and osteoporosis [Citation5].
Based on the recommendations by Lunenfeld et al., late-onset hypogonadism (LOH) is defined as a clinical and biochemical syndrome that is associated with advancing age and is characterized by hypogonadal symptoms and a deficiency in serum testosterone levels [Citation6]. LOH-related hypogonadal symptoms include decreased muscle mass and strength, decreased bone mass and osteoporosis, increased central body fat, decreased libido and sexual desire, forgetfulness, loss of memory, difficulty in concentration, insomnia and a decreased sense of well-being [Citation7]. LOH may be associated with a significant deterioration in health-related quality of life (HRQOL) and many adversely affect the function of multiple organ systems.
Although all modern guidelines assess testosterone replacement therapy (TRT) as safe if recommendations are followed properly, there may not be yet conclusive evidence as to the safety of TRT [Citation1]. In this study, we investigated the efficacy and safety of TRT given for at least six months in 50 consecutively enrolled Japanese men with LOH.
Methods
This study included a total of 50 consecutively enrolled male Japanese men (median age: 57.7 years) who were diagnosed with LOH and subsequently received TRT for at least six months at our institution between January 2009 and December 2012. Informed consent was obtained from all men prior to their participation in this study. Diagnosis of LOH was based on medical history, medications and physical findings collected from each patient, and the indication for TRT was determined according to the Clinical Practice Manual for Late-onset Hypogonadism Syndrome in Japan [Citation8]. Exclusion criteria included prostate cancer, elevation of serum prostate-specific antigen (PSA; ≥4 ng/ml), severe liver dysfunction, polycythemia and/or a history of treatment for LOH. After diagnosis with LOH, testosterone enanthate (250 mg every four weeks) was administered by intramuscular injection in all men.
Blood tests were performed to measure the following parameters at baseline and after six months of the treatment with TRT: the level of testosterone, free testosterone, total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein cholesterol, aspartate aminotransferase, alanine aminotransferase, gamma-glutamyl transpeptidase, glucose, hemoglobin A1c, red blood cell (RBC) count, hemoglobin (Hb), hematocrit (Ht) and PSA. Prostate volume and residual urine volume were also measured by ultrasound sonography. Body mass index (BMI) was also recorded. Erectile function and urinary symptoms status were analyzed using International Index of Erectile Function 5 (IIEF-5) [Citation9] and International Prostate Symptom Score (IPSS) [Citation10], respectively.
A Mini-International Neuropsychiatric Interview (M.I.N.I.) [Citation11] was performed to determine depression status at baseline and month six. In addition, Self-Rating Depression Scale (SDS) scores were examined to evaluate the changes in the severity of depression at baseline and month six [Citation12]. Furthermore, Aging Male Symptom (AMS) scores and the Medical Outcomes Study 8-item Short-Form health survey (SF-8) were measured to analyze the changes in HRQOL status in these men. As previously reported, AMS scores consist a total scale and sub-scales (mental, physical and sexual scales) [Citation13], while the Japanese version of the SF-8 contains eight HRQOL domains, including physical function, role limitation due to physical problems, bodily pain (BP), general health, vitality, social function, role limitation due to emotional problems and mental health [Citation14,Citation15].
All statistical analyses were performed by Wilcoxon signed-rank test using Statview software version 5.0 (Abacus Concepts, Inc., Berkeley, CA). All data were expressed as mean ± standard deviation, and p < 0.05 was considered to be statistically significant.
Results
As shown in , six months of treatment with TRT led to a significant increase from baseline in serum testosterone and free testosterone levels and a significant decrease from baseline in total cholesterol and LDL cholesterol. In addition, there was a significant increase from baseline at month six in RBC, Hb and Ht levels. There were no significant changes from baseline at month six in the levels of glucose and liver enzymes. There were no significant changes from baseline at month six in prostate volume and residual urine volume. There was a slight but significant increase from baseline at month six in mean PSA level. There was also a significant improvement from baseline at month six in IIEF-5 and IPSS scores.
Table 1. Changes in various parameters after ART.
At baseline, 30 of the 50 men included in this study (60%) were diagnosed with depression by M.I.N.I., only 11 of the 30 men (36.7%) were still suffering from depression following TRT. Furthermore, as assessed by SDS, the severity of depression in 30 men was significantly improved from baseline at month six. There was no significant change in BMI.
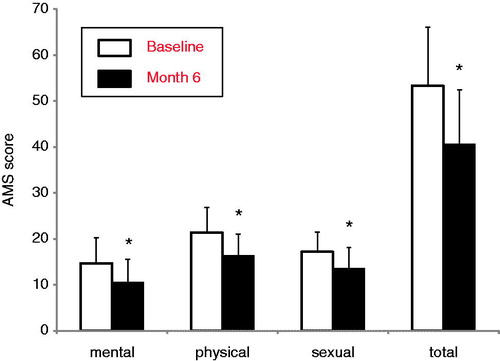
shows the changes in total scale and sub-scale AMS scores after six months of treatment with TRT. The total AMS score and all of the AMS sub-scales scores, including mental, physical and sexual scales decreased relative to baseline. However, the proportion of men showing a decrease from baseline in AMS scores did not significantly differ across subgroups categorized by the severity of this score at baseline (data not shown).
Figure 1. Comparison of total and sub-scales (mental, physical and sexual scales) of Aging Male Symptom (AMS) scores between Japanese men before and six months after testosterone replacement therapy (TRT) in late-onset hypogonadism (LOH) patients. *Significantly different from value before TRT (p < 0.001).
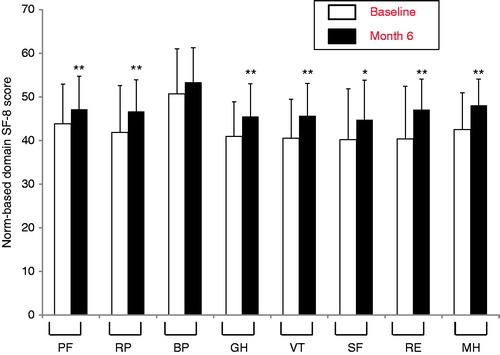
shows the changes in scale scores for the SF-8 survey. There was a significant increase from baseline at month six in all SF-8 scores, except for that of BP.
Figure 2. Comparison of scale scores on the Medical Outcomes Study 8-Item Short-Form Health Survey (SF-8) between Japanese men before and six months after the introduction of testosterone replacement therapy (TRT). PF, physical function; RP, role limitation due to physical problems; BP, bodily pain; GH, general health; VT, vitality; SF, social function; RE, role limitation due to emotional problems and MH, mental health. * and ** significantly different from the value before TRT (p < 0.01 and p < 0.005, respectively).
Discussion
In recent years, ART has been widely administered to men with LOH. Despite the development of several LOH questionnaires, which are extremely useful as clinical tools, it remains difficult to evaluate objectively the efficacy and safety of TRT in order to consider TRT as a therapeutic choice for men with LOH. We performed comprehensive assessments of the efficacy and safety of TRT in 50 consecutive male Japanese men with LOH.
In this study, serum testosterone and free-testosterone levels were significantly increased with TRT, reaching levels within the normal range by month six.
Numerous previous studies have demonstrated that normalization of serum testosterone levels with TRT leads to significant improvement in a wide range of LOH symptoms in aging men [Citation16,Citation17].
Low testosterone levels appear to be associated with an increased mortality rate in aging men due to an increased risk of cardiovascular disease [Citation5]. In this study, treatment with TRT led to a significant decrease in total and LDL cholesterol, suggesting that TRT may have beneficial effects on cardiovascular disease risk.
A significant elevation in the values of RBC and Hb were detected following ART; however, these changes were not marked, and there was no patient with elevated levels of RBC and/or Hb who developed cardiovascular disease.
In this study, IIEF-5 scores were increased from baseline following TRT; however, it would be necessary to evaluate these scores with precision whether the increased IIEF-5 scores positively reflected a beneficial effect on the sexual symptoms in these men, considering the lower sexual activity of Japanese men than that of the Western population [Citation18]. One of the mechanisms of the improvement of IIEF-5 score by TRT is thought to be not only regulating NOS activity but also modulating phoshodiesterase-5 (PDE-5) activity [Citation19]. Another study revealed that TRT may have more significant effect on libido than erectile function [Citation20].
Previous studies have showed an adverse effect on lower urinary tract symptoms (LUTS) due to prostate enlargement induced by TRT [Citation21]. On the other hand, many recent study confirms that TRT is beneficial for LUTS [Citation22]. In a randomized controlled trial of 46 hypogonadal men, Shigehara et al. demonstrated that androgen improved LUTS in hypogonadal men with mild BPH [Citation23]. In our study, IPSS scores significantly decreased after TRT though prostate volume and residual urine volume had no significant change. A few studies have suggested that testosterone levels may have an effect on LUTS. The testosterone level may have some effects on the autonomic nervous system, activities of nitric oxide synthase, PDE-5 and Rho-kinase, through the androgen receptors localized on the lower urinary tract and may be related to urinary function [Citation24].
In this study, the severity of depression in 30 men was significantly improved from baseline at month six. Hypogonadal men exhibit a significantly higher prevalence of anxiety disorders and major depressive disorder [Citation25]. Some reports suggest that TRT in hypogonadal men greatly improves mood, alleviates anxiety and mitigates symptoms of depression [Citation26].
In recent years, a favorable HRQOL has been regarded as one of the most important concerns irrespective of different therapy modes, especially in men with benign diseases, such as LOH. Therefore, the main objective of medical intervention for such men is to relieve symptoms rather than to completely cure the disease.
In this study, the improvement of QOL by ART was clearly shown using two different QOL surveys, the AMS and the Japanese version of the SF-8. However, it remains unclear to analyze the symptomatic change contributing to the improved HRQOL after TRT, because favorable changes were detected in several symptoms, including erectile function, LUTS and depressive status.
Limitation of this study include its nature, relatively smaller sample size (n = 50). Second, this was a non-randomized, non-controlled, retrospective study. Third, this study included only aging male Japanese men with LOH, which may limit the ability to extrapolate these findings to the entire spectrum of men receiving TRT. Fourth, testosterone enanthate was used in four-weekly intervals in this study, which is underdosed compared with European or American guidelines; however, this dosage of testosterone enanthate may have sufficient effects on Japanese men. Finally, this study analyzed symptomatic changes after only 6 months of TRT; which again may limit the ability to draw conclusions about the long-term effects of TRT in men with LOH.
In conclusion, the findings of this small, non-randomized, retrospective study suggest that TRT is a safe and effective therapy in aging Japanese men with LOH.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Mäkinen JI, Huhtaniemi I. Androgen replacement therapy in late-onset hypogonadism: current concepts and controversies – a mini-review. Gerontology 2011;57:193–202
- Feldman HA, Longcope C, Derby CA, et al. Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the Massachusetts male aging study. J Clin Endocrinol Metab 2002;87:589–98
- Laughlin GA, Barrett-Connor E, Bergstrom J. Low serum testosterone and mortality in older men. J Clin Endocrinol Metab 2008;93:68–75
- Tivesten A, Vandenput L, Labrie F, et al. Low serum testosterone and estradiol predict mortality in elderly men. J Clin Endocrinol Metab 2009;94:2482–8
- Bassil N, Alkaade S, Morley JE. The benefits and risks of testosterone replacement therapy: a review. Ther Clin Risk Manag 2009;5:427–48
- Lunenfeld B, Saad F, Hoesl CE. ISA, ISSAM and EAU recommendation for investigation, treatment and monitoring of late-onset hypogonadism in males: scientific background and rationale. Aging Male 2005;8:59–74
- Liao CH, Wu YN, Lin FY, et al. Testosterone replacement therapy can increase circulating endothelial progenitor cell number in men with late onset hypogonadism. Andrology 2013;1:563–9
- Namiki M, Akaza H, Shimazui T, et al. Clinical practice manual for late-onset hypogonadism syndrome. Int J Urol 2008;15:377–88
- Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 1999;11:319–26
- Barry MJ, Fowler FJ Jr, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992;148:1549–57; discussion 1564
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22–33; quiz 34–57
- Tarolla E, Biondi M, Fabi E, et al. Measuring depression with questions about well-being: a study on psychiatric outmen. Riv Psichiatr 2012;47:304–8
- Heinemann LA, Zimmermann T, Vermeulen A, Thiel C. A New ‘Aging Male’s Symptoms’ (AMS) Rating scale. Aging Male 1999;2:105–14
- Fukuhara S, Bito S, Green J, et al. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol 1998;51:1037–44
- Fukuhara S, Suzukamo Y. Manual of the SF-8 Japanese version. Kyoto: Institute for Health Outcome and Process Evaluation Research; 2004
- Karazindiyanoğlu S, Cayan S. The effect of testosterone therapy on lower urinary tract symptoms/bladder and sexual functions in men with symptomatic late-onset hypogonadism. Aging male 2008;3:146–9
- Ho CK, Beckett GJ. Late-onset male hypogonadism: clinical and laboratory evaluation. J Clin Pathol 2011;6:459–65
- Kawa G, Taniguchi H, Kinoshita H, et al. Aging male symptoms and serum testosterone levels in healthy Japanese middle-aged men. Nihon Hinyokika Gakkai Zasshi 2008;99:645–51
- Traish AM, Goldstein I, Kim NN. Testosterone and erectile function: from basic research to a new clinical paradigm for managing men with androgen insufficiency and erectile dysfunction. Eur Urol 2007;1:54–70
- Shabsigh R. Hypogonadism and erectile dysfunction: the role for testosterone therapy. Int J Impot Res 2003;15(Suppl 4):S9–13
- Meikle AW, Arver S, Dobs AS, et al. Prostate size in hypogonadal men treated with a nonscrotal permeation-enhanced testosterone transdermal system. Urology 1997;49:191–6
- Pearl JA, Berhanu D, François N, et al. Testosterone supplementation does not worsen lower urinary tract symptoms. J Urol 2013;5:1828–33
- Shigehara K, Sugimoto K, Konaka H, et al. Androgen replacement therapy contributes to improving lower urinary tract symptoms in patients with hypogonadism and benign prostate hypertrophy: a randomised controlled study. Aging Male 2011;1:53–8
- Shigehara K, Namiki M. Late-onset hypogonadism syndrome and lower urinary tract symptoms. Korean J Urol 2011;10:657–63
- Zarrouf FA, Artz S, Griffith J, et al. Testosterone and depression: systematic review and meta-analysis. J Psychiatr Pract 2009;15:289–305
- Kanayama G, Amiaz R, Seidman S, Pope HG Jr. Testosterone supplementation for depressed men: current research and suggested treatment guidelines. Exp Clin Psychopharmacol 2007;15:529–38

