Abstract
Context: Rosemary essential oil has been used topically for several purposes (analgesic, anti acne, and anti-inflammatory) in Iranian traditional medicine.
Objectives: This investigation aimed to study the effect of essential oil of Rosmarinus officinalis L. (Lamiaceae) on the transdermal absorption of Na diclofenac from topical gel.
Material and methods: Diclofenac sodium topical gel was prepared with HPMC K4M and Carbopol 934P as a gelling agent, and several vehicles. The most stable gel was chosen and enhancing effects of the essential oil with different concentrations (0.1, 0.5, and 1.0% w/w) on the permeation of diclofenac were evaluated. The anti-nociceptive effect of preparations was evaluated based on the formalin and tail flick tests in mice.
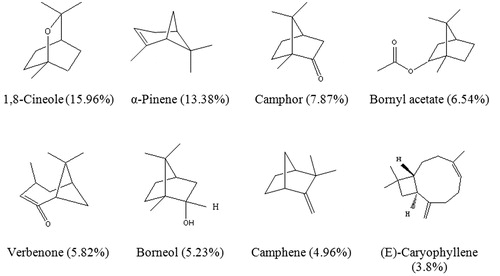
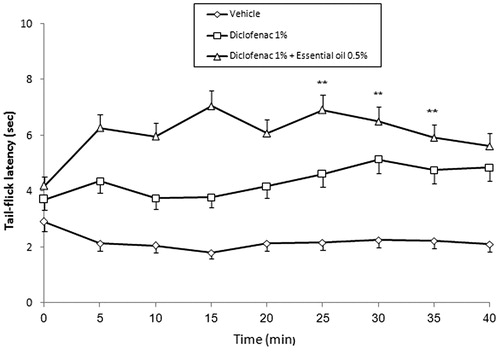
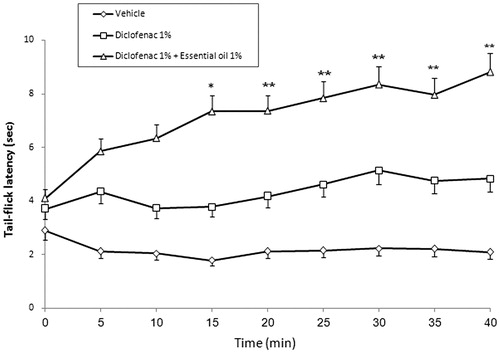
Results: The major constituents of the essential oil were 1,8-cineol (15.96%), α-pinene (13.38%), camphor (7.87%), bornyl acetate (6.54%), verbenone (5.82%), borneol (5.23%), camphene (4.96%), and (E)-caryophyllene (3.8%). Topical diclofenac containing 0.5% essential oil showed more analgesic effect after 25, 30, and 35 min (p < 0.001) than the reference drug in the tail flick test. The analgesic effect of preparation containing 1% essential oil was more than reference gel after 15 min (p < 0.05). This difference was observed after 20, 25, 30, 35, and 40 min (p < 0.001) too. Rosemary essential oil 1% promoted analgesic effect of drug in comparison with diclofenac gel in the formalin early phase (p < 0.05). The enhancing effect of rosemary was observed in 0.5 and 1% concentration (p < 0.05 and p < 0.001, respectively) in the late phase.
Conclusion: This study proved the enhancing effect of 0.5 and 1% of rosemary essential oil on diclofenac percutaneous absorption.
Introduction
Diclofenac is one of the routinely prescribed anti-inflammatory agents available for the management of pain and inflammation (Boinpally et al., Citation2003). Topical non-steroidal anti-inflammatory drugs (NSAIDs) present a safer potential alternative to oral therapy, with decreased systemic exposure to the active NSAID molecule (Simon et al., Citation2009). Therefore, an improved diclofenac formulation with a high degree of skin permeation could be useful in the treatment of not only locally inflamed skin tissues but also inflammatory and painful states of supporting structures of the body-bones, ligaments, joints, tendons, and muscles (Komatsu & Sakurada, Citation2012). For the last two decades, the skin has become important for drug delivery for topical, regional, or systemic effects. Nevertheless, human skin is a remarkably efficient barrier, thus causing difficulties for transdermal delivery of therapeutic agents since few drugs have the characteristics required to permeate sufficiently across the stratum corneum to reach therapeutic blood concentration. In order to enhance drug transdermal absorption, different methodologies have been investigated and developed, including the use of drug derivatives, drug-saturated systems, and physical and chemical enhancers that facilitate the diffusion of drugs through the stratum corneum (Femenía-Font, Citation2005).
Some researchers investigated the enhancing effects of the extracts, essential oils, or natural compounds (e.g., terpenes) on the in vitro percutaneous absorption of drugs (Abdullah et al., Citation1996; Das et al., Citation2006; Fang et al., Citation2004; Nokhodchi et al., Citation2007; Saeedi & Morteza-Semnani, Citation2008). Terpene is a constituent of an essential oil and consists of isoprene (C5H8) units. 1,8-Cineole has been used to promote the percutaneous of several lipophilic drugs through hairless mouse skin. Currently, natural products are receiving considerable interest in the pharmaceutical industry, and terpenes may provide a series of relatively safe, clinically acceptable accelerants for lipophilic and hydrophilic drugs (Gao & Singh, Citation1997). Niaouli oil 10% in propylene glycol (containing 1,8-cineole, α-pinene, and d-limonene as major constituents) showed enhancing effect on estradiol percutaneous absorption from hairless mouse skin (Monti et al., Citation2002).
Rosemary, Rosmarinus officinalis L. (Lamiaceae), is an evergreen plant typical of the Mediterranean region and many regions of Iran (Zargari, Citation1992). It has been used since ancient times for medicinal purposes and known for its antiseptic, antioxidant (Beretta et al., Citation2011; Morteza-Semnani et al., Citation2005; Zaouali et al., Citation2010), anti-rheumatic, antispasmodic (Zaouali et al., Citation2013), anti-inflammatory (Lee et al., Citation2008), and healing effects (Abu-Al-Basal, Citation2010). The objective of the present paper is to examine the influence of the rosemary essential oil on the percutaneous absorption and analgesic effect of diclofenac topical gel in mice through tail-flick and formalin tests.
Materials and methods
Materials
The following chemicals were used as received from the suppliers: methyl and propyl paraben, glycerin, ethanol, Tween 80, triethanolamine (Merck, Darmstadt, Germany), Carbopol 934P (BF Goodrich, Cleveland, OH), hydroxypropyl methylcellulose (HPMC, from Colorcon, Dartford, UK), and rosemary essential oil (Barij Essence, Tehran, Iran).
Gas chromatography–mass spectrometry (GC-MS) analysis
The essential oil was analyzed by GC and GC-MS analyses. Gas chromatographic analysis was carried out on a Perkin-Elmer 8500 gas chromatograph (PerkinElmer, Inc., San Jose, CA) with a FID detector and a DB-5 capillary column (30 m × 0.25 mm; film thickness 0.25 µm). The operating conditions were as follows: carrier gas helium with a flow rate of 2 mL/min, the split ratio was 1:30, the oven temperature was programmed 4 min. Isothermal at 60 °C and then 60–220 °C at 4 °C/min., injector and detector temperatures were set at 240 °C.
GC-MS was carried out on Hewlett Packard 6890 series (Hewlett-Packard Enterprise, Palo Alto, CA), using a DB-5 capillary column (30 m × 0.25 mm, film thickness 0.25 µm) which was programmed as follows: 60 °C for 5 min and then up to 220 °C at 4 °C/min. The carrier gas was helium at a flow rate of 2 mL/min. The carrier gas was helium at a flow rate of 2 mL/min; split ratio, 1:40; ionization energy, 70 eV; scan time, 1 s; acquisition mass range, m/z 40–400.
The components of the oil were identified by their retention time, retention indices relative to C9–C28 n-alkanes, computer matching with the WILEY275.L library as well as by comparison of their mass spectra with those of authentic samples or with data already available in the literature (Adams, Citation2007; Davies, Citation1990).
Preparation of Na diclofenac gels
The polymer (HPMC or carbopol) was dispersed in preserved vehicle (methyl paraben 0.18% and propyl paraben 0.02%), Tween 80 (0.2%), and glycerin for overnight (). The Na diclofenac (1%) was dissolved in vehicle before the addition of polymer. The enhancers (rosemary essential oil) in different concentrations (0.1, 0.5, and 1%) were added to the mixture before polymer suspending and stirred with a double-bladed mixer (Ika-werke, Staufen, Germany) 500 rpm for 30 min. The formulations containing carbopol as the gelling agent were neutralized by triethanolamine finally. The formulations were kept in 4, 25, and 40 °C for physical stability evaluation during 2 weeks and the best formulations based on consistency, homogeneity, syneresis, swelling, and clarity were selected for analgesic tests (Saeedi et al., Citation2007).
Table 1. The constituents of investigated formulations.
Animals
Male Swiss–Webster mice, weighing 25–30 g were used. The animals were housed nine per plastic cage in an animal room maintained at 21 ± 2 °C on a 12 h light/dark cycle (lights on 07:00–19:00 h). Food and water were available at all times except during the experiments. Each animal was used once only. This research approved by ethical committee of Mazandaran University of Medical Sciences (No. 90-62).
Tail flick test
The tail flick test was carried out in accordance to the method described elsewhere (Dewey, Citation1981), with minor modification. In brief, 0.5 g of diclofenac topical gel (1%) containing 0.1, 0.5, and 1.0% of rosemary essential oil was applied to the tail (n = 6) gently rubbing 50 times with the index finger. Mouse of the control groups received only the gel base. Na diclofenac topical gel (1%) applied in the same way was used as a reference. The tail of the mouse was placed on the photo element window of a Tail flick apparatus (Model DS20, Hugo Basile, Varese, Italy) and an infrared beam was focused on the tail area, 2 cm from its base. The latency time to respond to the pain stimuli was recorded. To avoid tissue damages, the maximal exposure to the pain stimuli was restricted to 10 s. The tail flick response was tested every 5 min till 40 min after topical administration at the preparations.
Formalin test
Diclofenac topical gel 1% (0.2 g) containing 0.1, 0.5, and 1.0% of rosemary essential oil was applied to the dorsal surface of the left hind paw (n = 6) by gently rubbing 50 times with the index finger. Mouse of the control groups received only the gel base. Na diclofenac topical gel (1%) applied in the same way was used as a reference. Fifteen minutes later, the anti-nociceptive activity was determined using the formalin test described by Dubuisson and Dennis (Citation1977). Formalin (2.5%, 50 μL) was injected to the dorsal surface of the left hind paw. The mice were observed for 60 min after the injection of formalin, and the amount of time spent licking the injected hind paw was recorded. The first 5 min post-formalin injection is known as the early phase and the period between 15 and 60 min as the late phase (Morteza-Semnani et al., Citation2004).
Statistical analysis
Repeat measurement ANOVA followed by the Newman–Keuls test was used to determine significant differences between groups, and p < 0.05 was considered significant.
Results
In this study, the GC-MS analysis showed that essential oil of R. officinalis was rich in monoterpenoids. The major constituents of the essential oil were 1,8-cineol (15.96%), α-pinene (13.38%), camphor (7.87%), bornyl acetate (6.54%), verbenone (5.82%), borneol (5.23%), camphene (4.96%), and (E)-caryophyllene (3.8%); these compounds were also identified in . Similar results were reported in previous researches; in one study, a total of 25 components accounting for 93.6–97.5% of essential oil were identified. 1,8-Cineol (40.0%), camphor (17.9%), α-pinene (10.3%), and camphene (6.3%) were the main constituents of essential oil of rosemary collected from Tunisia (Zaouali et al., Citation2010). Similar compounds were reported from Iran and China in other studies (Gachkar et al., Citation2007; Wang et al., Citation2008).
Figure 1. The major constituents of the essential oil of the aerial parts of Rosmarinus officinalis L.
Several formulations were prepared and the best formulation (F6) was chosen based on the physical stability as main Na diclofenac gel 1%. The formulation ingredients of selected topical gels for pharmacological evaluation are shown in .
The tail flick test was carried out every 5 min until 40 min after topical administration. All tested preparations possessed analgesic activity after 5 min following topical administration. The Na diclofenac 1% gel showed similar anti-nociceptive effect on preparation containing drug and rosemary essential oil 0.1% as an enhancer (). Topical Na diclofenac containing 0.5% essential oil as the enhancer showed more analgesic effect after 25, 30, and 35 min (p < 0.001) than the reference drug (diclofenac Na 1%). This difference was not significant in the 40th min ().
Figure 2. The effect of the presence of rosemary essential oil (0.1%) in Na Diclofenac (1%) topical preparation on tail-flick latency; values are mean ± SD (n = 6 animals per group).
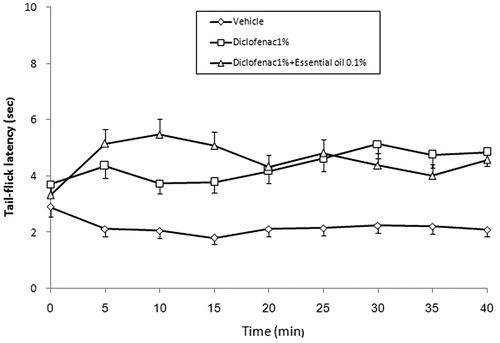
Figure 3. The effect of the presence of rosemary essential oil (0.5%) in Na Diclofenac (1%) topical preparation on tail-flick latency; values are mean ± SD (n = 6 animals per group). **p < 0.001 (Student–Newman–Keuls test).
The effect of rosemary essential oil on anti-nociceptive effect of Na diclofenac was observed in 1% concentration significantly. The analgesic effect of this preparation was more than the reference drug containing gel after 15 min (p < 0.05). This difference was also observed after 20, 25, 30, 35, and 40 min (p < 0.001) ().
Figure 4. The effect of the presence of rosemary essential oil (1%) in Na Diclofenac (1%) topical preparation on tail-flick latency; values are mean ± SD (n = 6 animals per group). *p < 0.05 and **p < 0.001 (Student–Newman–Keuls test).
The results of formalin test are shown in and . The analysis of data showed the analgesic effect of all investigated preparations in comparison with the vehicle in the early and late phases of the formalin test. The results () showed that addition of 0.1 and 0.5% of essential oil had no significant effect on the early phase anti-nociceptive effect of diclofenac. The more analgesic effect of diclofenac gel containing rosemary essential oil 1% was observed in comparison with diclofenac gel in the early phase (p < 0.05).
Figure 5. The effect of the presence of rosemary essential oil (0.1, 0.5, and 1%) in Na Diclofenac (1%) topical preparation on the first phase (0–5 min) anti-nociception in the formalin test; values are mean ± SD (n = 6 animals per group). *p < 0.05 (Student–Newman–Keuls test).
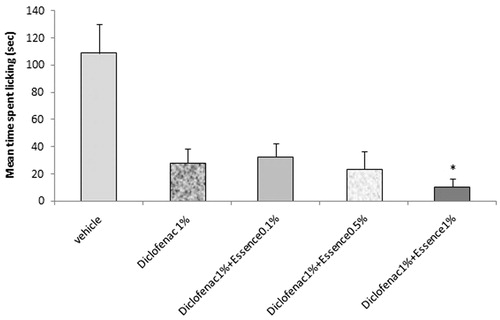
Figure 6. The effect of the presence of rosemary essential oil (0.1, 0.5, and 1%) presence in Na Diclofenac (1%) topical preparation on the late (15–50 min) phase anti-nociception in the formalin test; values are mean ± SD (n = 6 animals per group). *p < 0.05 and **p < 0.001 (Student–Newman–Keuls test).
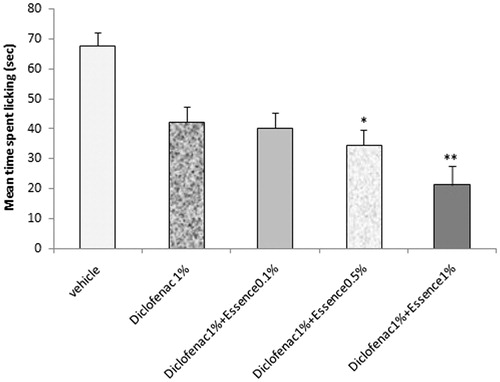
The results of the formalin test in the late phase showed that 0.1% rosemary essential oil had no significant effect on anti-nociceptive action of Na diclofenac. The enhancing effect of rosemary essential oil was observed in 0.5 and 1% concentration (p < 0.05 and p < 0.001, respectively) in the late phase of the formalin test ().
Discussion
The antimicrobial effect of rosemary essential oil was reported against Escherichia coli, Pseudomonas aeruginosa, Klebsiela pneumonia, Staphylococcus aureus, Bacillus subtilis, Staphylococcus epidermis, and Sterptococcus feacalis (Celiktas et al., Citation2007; Wang et al., Citation2008). Antioxidant activity of this essential oil was observed in this study also (Zaouali et al., Citation2010). The aerial part of this plant has a long tradition of use as antispasm in renal colic, antispasm, and analgesic in dysmenorrhea, anti-rheumatic, anti-aging, effective in respiratory disorders, lowering blood pressure, relieving kidney stones and digestive disease, and healing effect (Abu-Al-Basal, Citation2010).
One of the components of plants' essential oil is terpenes. Terpenes are promising, clinically acceptable enhancers because of their low systemic toxicity, high enhancement activity, and low cutaneous irritation at low concentration between 1 and 5% (Saeedi & Morteza-Semnani, Citation2008). These properties led us for using essential oil of R. officinalis as an enhancer in Na diclofenac gel. The results showed that the essential oil of rosmary was rich in monoterpenoids. These results were observed and reported in another researches previously (Gachkar et al., Citation2007; Wang et al., Citation2008; Zaouali et al., Citation2010).
Diclofenac sodium topical gel was prepared with HPMC K4M and Carbopol 934P as the gelling agent, and several vehicles. The formulations were examined for pH, spreadibility, consistency, homogeneity, and physical stability at three temperatures: 4, 25, and 40 °C for 3 months (data were not shown). The carbopol showed suitable effect as the gelling agent and formulations were designed as mentioned in . Carbopol 940 (0.75%) was used for the formulation of rosemary essential oil containing topical gel in one study. The results showed suitable stability in Carbopol 940 gel containing rosemary essential oil (Shukr & Metwally, Citation2013).
In the first phase of the formalin test, the significant analgesic activity of preparation was observed in diclofenac topical gel containing rosemary essential oil 1%. This anti-nociceptive effect was increased in preparations containing 0.5 and 1% of essential oil in the late phase of the formalin test. The tail flick test revealed these results too. The tail flick latency time increased in animals which received diclofenac topical preparations containing rosemary essential oil. This enhancing effect on analgesic property of topical preparation was significantly concentration dependent and was observed in topical gels containing 0.5 and 1% of rosemary essential oil.
Hydrophilic terpenes (alcohol, ketone, and oxide terpenes) are good candidates in enhancing the permeation of non-steroidal anti-inflammatory drugs. In some studies with indomethacin, as a lipophilic molecule, drug absorption was markedly enhanced by the addition of hydrophobic cyclic monoterpenes, while hydrophilic ones showed minor effects (Okabe et al., Citation1989). In contrast, a study performed under similar conditions, with diclofenac sodium as a hydrophilic penetrant, suggested an alcohol terpene (menthol) to be the most effective penetration enhancer (Williams & Barry, Citation1989). Also Arellano et al. (Citation1996) described the alcohol terpenes as the most effective accelerants for this NSAID followed by ketones and oxides.
Ghafourian et al. (Citation2004) investigated the structural requirements of some terpens as penetration enhancer using the quantitative structure–activity relationship (QSAR) technique. The results indicated that for diclofenac sodium, less hydrophobic enhancers were the most active.
1,8-Cineol, camphor, bornyl acetate, verbenone, and borneol as the main compounds of R. officinalis essential oil have a hydrophilic structure which accelerates transepidermal absorption of Na diclofenac. Camphor showed effective enhancement on percutaneous absorption of labetalol HCl (as a hydrophilic drug) across rat abdominal skin. This effect was more than basil oil, geraniol, thymol, and clove oil (Jain et al., Citation2008).
The enhancements could not be related to skin damage by the terpenes as they have been reported to be safe and non-toxic at high concentrations/or pure form. In experiments where skin was treated with pure terpene for 12 h prior to the permeation studies, Yamane et al. (Citation1995) showed that the effect of terpenes on skin is reversible using differential scanning calorimetery. Terpenes seem to increase skin permeability mainly through the enhancement of permeant diffusion. Jain et al. (Citation2002) reported that the contribution of partitioning in enhanced permeation of imipramine hydrochloride after terpene treatment at 5% (w/v) as negligible. Yamane et al. (Citation1995), however, reported some increase in partitioning of 5-fluorouracil after 6 or 12 h treatment with certain terpenes whereas d-limonene produced no positive effect on the drug partitioning.
The effect of rosemary essential oil on primary hypotension and its influence on both physical and psychological aspects responsible for quality of life of patients was evaluated. The results showed that rosemary essential oil to be safe. This essential oil showed significant lowering effect on systolic and diastolic blood pressures (Fernandez et al., Citation2014). It seems that rosemary essential oil can increase percutaneous absorption due to vasodilation effect.
Two other mechanisms of permeation enhancement are possible: increased lipid disruption in the stratum corneum by extract and essential oil constituents and the complex formation between the enhancer and the drug or structures from stratum corneum (Williams & Barry, Citation1989, Citation1991).
Conclusion
In conclusion, this study demonstrated that diclofenac sodium topical gel had significantly enhanced analgesic effect in combination with rosemary essential oil. This effect was concentration dependent and the most enhancing effect was observed in 1%. This essential oil was rich of monoterpenoids, especially 1,8-cineole which can promote skin absorption.
Declaration of interest
The authors report that there are no declaration of interest. This work was supported by a grant from the research council of the Mazandaran University of Medical Sciences.
References
- Abdullah D, Ping QN, Liu GJ. (1996). Enhancing effect of essential oils on the penetration of 5-fluorouracil through rat skin. Yao Hsueh Hsueh Pao (Acta Pharm Sin) 31:214–21
- Abu-Al-Basal MA. (2010). Healing potential of Rosmarinus officinalis L. on full-thickness excision cutaneous wounds in alloxan-induced-diabetic Balb/c mice. J Ethnopharmacol 131:443–50
- Adams RP. (2007). Identification of Essential Oil Components by Gas Chromatography/Mass Spectrometry, 4th Ed. Illinois: Allured Publishing Corp., 10–27
- Arellano A, Santoyo S, Martin C, Ygartua P. (1996). Enhancing effect of terpenes on the in vitro percutaneous absorption of diclofenac sodium. Int J Pharm 130:141–5
- Beretta G, Artali R, Maffei Facino R, Gelmini F. (2011). An analytical and theoretical approach for the profiling of the antioxidant activity of essential oils: The case of Rosmarinus officinalis L. J Pharm Biomed Anal 55:1255–64
- Boinpally RR, Zhou SL, Poondru S, et al. (2003). Lecithin vesicles for topical delivery of diclofenac. Eur J Pharm Biopharm 56:389–92
- Celiktas OY, Hames Kocabas EE, Bedir E, et al. (2007). Antimicrobial activities of methanol extracts and essential oils of Rosmarinus officinalis, depending on location and seasonal variations. Food Chem 100:553–9
- Das MK, Bhattacharya A, Ghosal SK. (2006). Effect of different terpene-containing essential oils on percutaneous absorption of trazodone hydrochloride through mouse epidermis. Drug Deliv 13:425–31
- Davies NW. (1990). Gas chromatographic retention indices of monoterpenes and sesquiterpenes on methyl silicone and carbowax 20M phases. J Chromatogr 503:1–24
- Dewey WL. (1981). Background on animal testing in the drug delivery systems program. NIDA Res Monogr 28:69–76
- Dubuisson D, Dennis SG. (1977). The formalin test: A quantitative study of the analgesic effect of morphine, meperidine and brain stem stimulation in rats and cats. J Pain 4:167–74
- Fang JY, Leu YL, Hwang TL, Cheng HC. (2004). Essential oils from sweet basil (Ocimum basilicum) as novel enhancers to accelerate transdermal drug delivery. Biol Pharm Bull 27:1819–25
- Femenía-Font A, Balaguer-Fernández C, Merino V, et al. (2005). Effect of chemical enhancers on the in vitro percutaneous absorption of sumatriptan succinate. Eur J Pharm Biopharm 61:50–5
- Fernandez LF, Palomino OM, Frutos G. (2014). Effectiveness of Rosmarinus officinalis essential oil as antihypotensive agent in primary hypotensive patients and its influence on health-related quality of life. J Ethnopharmacol 151:509–16
- Gachkar L, Yadegari D, Rezaei MB, et al. (2007). Chemical and biological characteristics of Cuminum cyminum and Rosmarinus officinalis essential oils. Food Chem 102:898–904
- Gao S, Singh J. (1997). Mechanism of transdermal transport of 5-fluorouracil by terpenes: Carvone, 1,8-cineole and thymol. Int J Pharm 154:67–77
- Ghafourian T, Zandasrar P, Hamishekar H, Nokhodchi A. (2004). The effect of penetration enhancers on drug delivery through skin: A QSAR study. J Control Release 99:113–25
- Jain AK, Thomas NS, Pachagnula R. (2002). Transdermal drug delivery of imipramine hydrochloride. J Control Release 79:93–101
- Jain R, Aqil M, Ahad A, et al. (2008). Basil oil is a promising skin penetration enhancer for transdermal delivery of labetalol hydrochloride. Drug Dev Ind Pharm 34:384–9
- Komatsu T, Sakurada T. (2012). Comparison of the efficacy and skin permeability of topical NSAID preparations used in Europe. Eur J Pharm Sci 47:890–5
- Lee J, Jung E, Koh J, et al. (2008). Effect of rosmarinic acid on atopic dermatitis. J Dermatol 35:768–71
- Monti D, Chetoni P, Burgalassi S, et al. (2002). Effect of different terpene-containing essential oil on permeation of estradiol through hairless mouse skin. Int J Pharm 237:209–14
- Morteza-Semnani K, Saeedi M, Hamidian M. (2004). Anti-inflammatory and analgesic activity of the topical preparation of Glaucium grandiflorum L. Fitoterapia 75:123–9
- Morteza-Semnani K, Saeedi M, Nozadi Z. (2005). Antioxidant activity of rosemary extract in 2% hydroquinone cream. Int J Biol Biotech 2:723–7
- Nokhodchi A, Sharabiani K, Rashidi MR, Ghafourian T. (2007). The effect of terpene concentrations on the skin penetration of diclofenac sodium. Int J Pharm 335:97–105
- Okabe H, Takayama K, Ogura A, Nagai T. (1989). Effect of limonene and related compounds on the percutaneous absorption of indomethacin. Drug Des Deliv 4:313–21
- Saeedi M, Kosaryan M, Fekri K, et al. (2007). A randomized double blind, controlled trial of testosterone gel treatment versus vehicle control on the facial hair of young men with beta-thalassemia major. J Dermatol Treat 18:271–4
- Saeedi M, Morteza-Semnani K. (2008). Effect of essential oil of Eryngium caeruleum on percutaneous absorption of piroxicam through rat skin. J Essent Oil Bear Plants 11:485–95
- Shukr MH, Metwally GF. (2013). Evaluation of topical gel bases formulated with various essential oils of antibacterial activity against methicillin-resistant Staphylococcus aureus. Trop J Pharm Res 12:877–84
- Simon LS, Grierson LM, Naseer Z, et al. (2009). Efficacy and safety of topical diclofenac containing dimethyl sulfoxide compared with those of topical placebo, DMSO vehicle and oral diclofenac for knee osteoarthritis. Pain 143:238–45
- Wang W, Wu N, Zu YG, Fu YJ. (2008). Antioxidative activity of Rosmarinus officinalis L. essential oil compared to its main components. Food Chem 108:1019–22
- Williams AC, Barry BW. (1989). Essential oils as novel human skin penetration enhancers. Int J Pharm 57:R7–9
- Williams AC, Barry BW. (1991). Terpenes and lipid protein partitioning theory of skin penetration enhancement. Pharm Res 8:17–24
- Yamane MA, Williams AC, Barry BW. (1995). Effects of terpenes and oleic acid as skin penetration enhancers towards 5-fluorouracil as assessed with time; permeation, partitioning and differential scanning calorimetery. Int J Pharm 116:237–51
- Zaouali Y, Chograni H, Rim T, Boussaid M. (2013). Changes in essential oil composition and phenolic fraction in Rosmarinus officinalis L. var. typicus Batt. organs during growth and incidence on the antioxidant activity. Ind Corps Prod 43:412–19
- Zaouali Y, Bouzaine T, Boussaid M. (2010). Essential oils composition in two Rosmarinus officinalis L. varieties and incidence for antimicrobial and antioxidant activities. Food Chem Toxicol 48:3144–52
- Zargari A. (1992). Medicinal Plants, vol. 4. Tehran, Iran: Tehran University Publications, pp. 71–5

