Abstract
Objectives. A ruptured sinus of Valsalva aneurysm is a very rare cardiac anomaly. Successful repair of these aneurysms was first described in the late 1950s. Several approaches for repair, through the aortic root or the chamber into which the aneurysm ruptures or a combination of both, have been described. We present our experience with emergency surgical repair of ruptured sinus of Valsalva aneurysms and our current surgical policy. Design. A review of the St. Antonius Hospital database from January 1972 to December 2010 identified a total of 16 patients. A retrospective review of their medical records and telephonic follow-up was performed. Results. Fifteen patients (13 male, three female) aged 46 ± 13 years were operated. The ruptured aneurysm arose from the right coronary (63%) and non-coronary sinus (37%) and ruptured into the right ventricle (67%) and into right atrium (33%). Primary suture closure was done in six patients and patch closure was performed in the remaining 10 patients. No intra-operative death occurred. Long-term follow-up identified one recurrent fistula from right coronary sinus to right atrium 28 years after primary suture closure. Conclusions. We performed prompt surgical repair of the ruptured sinus of Valsalva aneurysm preferably with a patch.
Key words::
Aneurysms of the sinus of Valsalva are rare cardiac anomalies. They are thin-walled diverticular outpouchings, nearly always in the right coronary sinus or the adjacent half of the non-coronary sinus. They may be congenital, as result of absent muscular and elastic tissue in the aortic wall of the sinus of Valsalva or acquired, with aortic valve endocarditis being the most common cause (Citation1,Citation2). It is usually asymptomatic, but when rupture or a fistula develops, symptoms occur and the patient's condition deteriorates rapidly. A ruptured aneurysm of the sinus of Valsalva is very rare. Reported incidences are low, 0.14–0.96% of all cardiac operations requiring cardiopulmonary bypass. Incidence is higher in males and the Asian population (Citation3). The rupture results in a fistulous connection usually originating from the right coronary sinus to an adjacent structure, often the right atrium or ventricle. Association with other cardiac lesions such as ventricular septal defect (VSD) and aortic valve regurgitation are common. A ruptured aneurysm of the sinus of Valsalva produces symptoms in 80% of patients, although the severity is determined by the presence of a ventricular septum defect or aortic regurgitation. Successful repair of a ruptured aneurysm of the sinus of Valsalva was first described in the late 1950s (Citation4). Several approaches for repair, through the aortic root or the chamber into which the aneurysm ruptures or a combination of both, have been described. In this article we present our experience with emergency surgical repair of ruptured sinus of Valsalva aneurysms and our surgical policy.
Material and methods
Study population and data collection
A review of the St. Antonius Hospital database from January 1972 to December 2010 identified a total of 16 patients who underwent immediate emergency surgery for a ruptured sinus of Valsalva aneurysm. A retrospective review of their medical records was performed. Follow-up was performed by telephonic interview with patients and medical record review from the general practitioner.
Statistical analysis
Frequencies or percentages were used to describe categorical variables. Continuous variables were described as mean ± S.D. or median.
Results
Patient profile
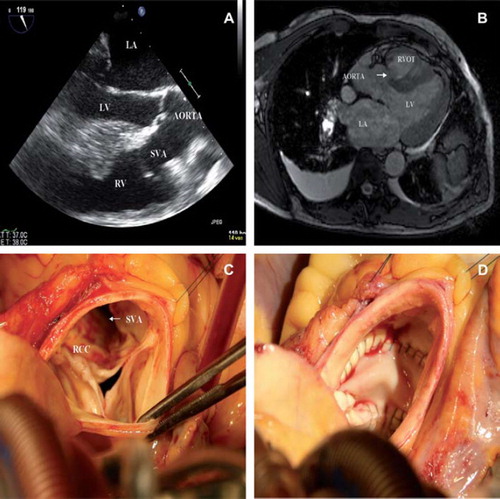
The mean age at operation was 46 ± 14 years (range 19 to 71 years). Eighty one percent (n = 13) of the patients were male. All patients were symptomatic at the time of admission and five (30%) were in New York Heart Association functional classes III and IV. Dyspnea (80%), palpitations (60%) and chest pain (40%) were the major symptoms with the common clinical finding of a continuous murmur at the left sternal border. Chest x-ray findings included an increased cardiothoracic ratio and congested lung fields. Electrocardiography showed normal sinus rhythm in all patients with left ventricular hypertrophy in five and a right bundle branch block in three patients. Diagnosis was established by transthoracic or transesophageal echocardiography (). Cardiac catheterization was carried out in four patients revealing one patient with a significant lesion in the left anterior descending artery (LAD), three patients underwent computed tomography (CT)-scanning or magnetic resonance imaging (MRI). The aneurysm arose from the right coronary sinus in 10 patients (63%) and from the non-coronary in six (37%). It ruptured into the right ventricle in 11 patients and into the right atrium in five. Only one of the patients had an associated VSD. Aortic regurgitation grade II-III / IV was present in six patients. One patient had an aortic valve stenosis as well as a pulmonary valve stenosis due to the presence of a subvalvular membrane. Tricuspid insufficiency requiring repair was present in one patient.
Figure 1. A. Transesophageal echocardiography showing a ruptured sinus of Valsalva (SVA) originating from the right-coronary cusp ending in the right ventricle (RV), left ventricle (LV), left atrium (LA). B. Pre-operative MRI, arrow indicating ruptured sinus of Valsalva aneurysm (SVA). C. Peri-operative picture looking inside the aortic root showing a windsock like aneurismal sac. Right coronary cusp (RCC). D. Peri-operative picture looking inside the aortic root the patch closed defect.
Operative techniques
Surgical repair was done using cardiopulmonary bypass (CPB) with moderate hypothermia (25°C to 34°C) via a median sternotomy in all patients. CPB was instituted using standard double venous cannulation and cannulation and clamping of the aorta. In the majority of cases (90%) a left ventricle vent was placed. Crystalloid cardioplegia, either selective coronary ostial or retrograde cardioplegia via coronary sinus infusion was used. In all cases an oblique or hockey stick aortotomy was performed. Repair was achieved through an additional incision in the chamber of termination in two cases. The defect in the sinus of Valsalva was closed after excising the aneurysm tissue. Primary suture closure of the ruptured sinus of Valsalva aneurysm was done in six patients (37%) and patch (autologous untreated pericard or Dacron) closure was performed in the remaining 10 patients (63%). Of the six patients with aortic regurgitation three received a Bentall procedure, one an aortic root homograft, one an aortic valve replacement (AVR) and one aortic valve could be spared by resuspension of the non-coronary cusp. In three patients the tricuspid valve was repaired. Modified supracoronary ascending aorta replacement with exclusion of the right coronary cusp and re-implantation of the right coronary artery was performed once. One patient received a venous graft on the LAD because of a significant stenosis, while another patient received a venous graft to the acute marginal branch after deliberate ligation of the right coronary artery. In the patient with the sub-valvular stenosis of the aortic and pulmonary valve the membranous tissue was excised. All patients could be weaned from CBP easily.
Outcome and follow-up
No intra-operative death was seen but one early death occurred. Surgical outcome in most patients was uneventful (93%). Early complications occurred in four patients. One patient required re- exploration due to excessive postoperative blood loss. A 55-year-old female showed severe neurological impairment after stopping all sedation. Repeated electroencephalogram (EEG) monitoring confirmed no cortical activity and further treatment was withheld. One patient was re-operated on the first postoperative day due to rhythm disturbances and signs of right ventricular failure, a venous bypass to the right coronary artery was performed, the patient recovered well afterwards. A fourth patient was re-operated for recurrent fistula and residual VSD seven days after primary surgery due to loosened pericardial patch and an iatrogenic induced peri-membranous lesion. Aortic root replacement using a homograft was performed and the VSD was closed with a pericardial patch. Long-term follow-up identified one recurrent fistula from right coronary sinus to right atrium 28 years after primary surgery. This defect was closed primarily through a trans-aortic approach, additionally the left internal mammary artery (LIMA) was grafted to the diagonal and LAD, and a venous jumpgraft was performed to the circumflex and postero-lateral branch of the right coronary artery due to significant lesions.
The remaining patients are well and symptom free. The average follow-up was 14.8 years (range 10 months to 40 years).
Discussion
The first description of aneurysmal enlargement of one of the sinuses of Valsalva is attributed to Hope in 1839. Thurnam described the clinical features of sinus of Valsalva aneurysms in a series of six cases (Citation5). Sinus of Valsalva aneurysms are rare with an incidence ranging from 0.1 to 3.5% of all congenital heart defects and account for only 0.14% of all open heart surgery (Citation2). Their exact prevalence is unknown, as the aneurysms are frequently clinically silent, however an autopsy study of 8138 individuals suggested a prevalence of 0.09% in the general population (Citation6). Sinus of Valsalva aneurysms have a marked male preponderance (4:1) and their incidence is higher in Asian populations (Citation7). The site of aneurysmal dilatation has been stated to be predominantly in the right coronary sinus (75–90%), followed by the non-coronary sinus (10–25%) with the reminder occurring in the left coronary sinus (Citation1).
These aneurysms may be acquired but are mostly congenital, due to incomplete fusion of the two halves of the distal bulbar septum. This is the structure that separates the aortic and pulmonary valves of the bulbar cordis, the primitive exit tube of the fetal heart (Citation8). Malfusion results in a weakness between the aortic annulus and aortic media. This predisposes to the formation of the aneurysmal sac. This sac appears as a windsock-like projection and is the result of continuous high aortic pressures on the weakened tissue (Citation9). Acquired sinus of Valsalva aneurysms are less commonly reported than congenital ones and are usually caused by conditions affecting the aortic wall, such as infection (syphilis, bacterial/fungal endocarditis or tuberculosis), degenerative disease (atherosclerosis, connective tissue disorders or cystic medial degeneration) or thoracic trauma (Citation10).
Sinus of Valsalva aneurysms may be clinical silent or cause symptomatic compression and distortion of the surrounding structures. It can become highly symptomatic due to intra-cardiac rupture resulting in life-threatening haemodynamic deterioration as a consequence of acute aortic regurgitation, coronary flow steal or massive left-to-right shunt. Less frequently it causes sudden death due to rupture into the pericardial, mediastinal or pleural cavities. Common symptoms include sudden onset of dyspnea, fatigue and paroxysmal nocturnal dyspnea or orthopnea due to abrupt volume overload caused by the left-to-right shunt. The symptoms are generally precipitated and aggravated by physical stress.
Ruptured sinus of Valsalva aneurysms are most common in men (two thirds of patients) and occur in the third or fourth decade of life (50–60% of patients). The right ventricle is the most common receiving chamber (80–90%), due to rupture of either right or non-coronary sinus of Valsalva aneurysms. Aortic valve abnormalities and aortic insufficiency occur in 25–45% of patients with ruptured aneurysms. VSD may coexist in these patients and is a predisposing factor for aortic insufficiency. Currently trans-thoracic colour Doppler echocardiography is the initial imaging technique of choice to delineate ruptured or unruptured sinus of Valsalva aneurysms.
Unruptured sinus of Valsalva aneurysms which produce hemodynamic derangements should be electively repaired. When a congenital sinus of Valsalva aneurysm has ruptured or is associated with a VSD prompt surgery is advisable since prognosis of patients without urgent repair is very poor. Successful repair of a ruptured aneurysm of the sinus of Valsalva was first described in the late 1950s. Recently percutaneous closure techniques have been used in selected cases. We believe that, although this approach may have several potential advantages mainly in high risk or unstable patients, surgery remains the treatment of choice since percutaneous closure may not halt progression of the aneurysm or revert the risk of further fistulae (Citation11). Surgical repair has an operative mortality rate of less than 2% and a good long-term outcome with 85% of the patients remaining in New York Heart Association Functional Class I or II (Citation12). Vural et al. proposed an algorithm-dependent classification for the timing of surgical repair (Citation13).
The surgical approach depends on various factors such as the site to which the aneurysm has ruptured, the need to repair or replace the aortic valve, the presence or absence of an orifice of the aneurysm and the presence of other cardiac abnormalities. In the case of ruptured sinus of Valsalva aneurysms the fistula tract should be exposed from the chamber of termination as well as through the aorta. Primary suture closure, patch closure or aortic root replacement have been used to repair the aneurysm. The recommended operative procedure is patch closure of the orifice of the aneurysm in most cases because it avoids deforming the aortic valve and reduces stress on the suture line, possibly improving long-term results relative to that of direct closure (Citation14). In support of this assertion, two reports have correlated primary closure with recurrent rupture (Citation12,Citation15). Other clinicians however maintain that direct closure is sufficient and easier for the repair of small aneurysms (Citation16,Citation17). We use primary closure for small aneurysms and Dacron or pericardial patches to repair larger lesions. Patch repair is especially useful in cases in which direct closure could deform the aortic valve.
Valve prolapse causing aortic regurgitation is reported in 30–50% of patients with sinus of Valsalva aneurysms. This prolapse can occur if the sinus of Valsalva aneurysm involves the aortic annulus, a concomitant VSD removes the support normally provided by the conus arteriosus or when a Venturi-effect on the involved leaflet pulls it into the sinus of Valsalva and causes it to prolapse into the left ventricular outflow tract. Successful aortic valve-sparing operations, such as remodelling or reimplantation procedures for multiple small sinus of Valsalva aneurysms have been reported but only when trivial to moderate aortic regurgitation was present and not in the presence of one large dilated sinus (Citation18,Citation19). In our series we had one patient who received a modified supracoronary ascending aorta replacement with exclusion of the right coronary cusp on re-implantation of the right coronary artery. In cases of moderate to severe aortic regurgitation, retracted, thickened or bicuspid aortic valve leaflets, AVR is usually required. There are also cases in which prosthetic replacement of the entire aortic root, reimplantation of the coronary arteries or both are required. In our series three patients received a Bentall procedure and one an aortic root homograft.
Surgical repair has high success rates with low operative mortality (approximately 1%) however mortality rates are higher in patients with infected sinus of Valsalva aneurysms (3.9%). Peri-operative mortality was additionally associated with pre-existing sepsis and endocarditis. Peri-operative mortality in patients with non-infected aneurysms is largely attributable to low cardiac output postoperatively. Late complications are related to prosthetic valve malfunction, endocarditis, aneurysm recurrence and anticoagulation related bleeding. If there is insufficiency of the native aortic valve after the repair, it will often progress and may eventually require the patient to undergo aortic valve replacement later. The risk for recurrent fistula or VSD is considered minimal in the current surgical era. The life expectancy of patients who have successful repair of a ruptured aneurysm approximates that of the healthy population (10 year survival rates of 90–95%).
In conclusion, ruptured sinus of Valsalva aneurysms are rare cardiac anomalies in need of urgent surgical intervention. We prefer repair of ruptured sinus of Valsalva aneurysms with a patch, through an aortotomy with or without exploration via the receiving chamber. Prompt surgical repair can prevent life-threatening complications and long-term survival equals that of the healthy population.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Edwards JE, Burchell HB. The pathological anatomy of deficiencies between the aortic root and the heart, including aortic sinus aneurysms. Thorax. 1957;12:125–39.
- Takach TJ, Reul GJ, Duncan JM, Cooley DA, Livesay JJ, Ott DA, . Sinus of Valsalva aneurysm or fistula: Management and outcome. Ann Thorac Surg. 1999;68:1573–7.
- Lin CY, Hong GJ, Lee KC, Tsai YT, Tsai CS. Ruptured congenital sinus of Valsalva aneurysms. J Card Surg. 2004; 19:99–102.
- Lillehei CW, Stanley P, Varco RL. Surgical treatment of ruptured aneurysms of the sinus of Valsalva. Ann Surg. 1957;146:459–72.
- Thurnam J. On aneurysms, and especially spontaneous aneurysms of the ascending aorta, and sinus of Valsalva. Med Dhir Tr. 1840;23:323.
- Smith WA. Aneurysm of the sinus of Valsalva, with report of 2 cases. JAMA 1878;62:1914.
- Chu SH, Hung CR, How SS, Chang H, Wang SS, Tsai CH, . Ruptured aneurysms of the sinus of Valsalva in Oriental patients. J Thorac Cardiovasc Surg. 1990;99:288–98.
- Jones AM, Langley FA. Aortic sinus aneurysms. Br Heart J. 1949;11:325–41.
- Goldberg N, Krasnow N. Sinus of Valsalva aneurysms. Clin Cardiol. 1990;13:831–6.
- Sokol DM, Trachtenberg J, Goldman BS, Mustard WT. Surgical experience with ruptured aneurysms of the sinuses of Valsalva. Chest. 1973;64:615–8.
- Chang CW, Chiu SN, Wu ET, Tsai SK, Wu MH, Wang JK. Transcatheter closure of a ruptured sinus of Valsalva aneurysm. Circ J. 2006;70:1043–7.
- Barragry TP, Ring WS, Moller JH, Lillehei CW. 15- to 30-year follow-up of patients undergoing repair of ruptured congenital aneurysms of the sinus of Valsalva. Ann Thorac Surg. 1988;46:515–9.
- Vural KM, Sener E, Ta demir O, Bayazit K. Approach to sinus of Valsalva aneurysms: A review of 53 cases. Eur J Cardiothorac Surg. 2001;20:71–6.
- Wang ZJ, Zou CW, Li DC, Li HX, Wang AB, Yuan GD, . Surgical repair of sinus of Valsalva aneurysm in Asian patients. Ann Thorac Surg. 2007;84:156–60.
- Azakie A, David TE, Peniston CM, Rao V, Williams WG. Ruptured sinus of Valsalva aneurysm: Early recurrence and fate of the aortic valve. Ann Thorac Surg. 2000;70:1466–70.
- Au WK, Chiu SW, Mok CK, Lee WT, Cheung D, He GW. Repair of ruptured sinus of Valsalva aneurysm: Determinants of long-term survival. Ann Thorac Surg. 1998;66: 1604–10.
- Henze A, Huttunen H, Björk VO. Ruptured sinus of Valsalva aneurysms. Scand J Thorac Cardiovasc Surg. 1983;17: 249–53.
- Akashi H, Tayama E, Tayama K, Kosuga T, Takagi K, Aoyagi S. Remodeling operation for unruptured aneurysms of three sinuses of Valsalva. J Thorac Cardiovasc Surg. 2005;129: 951–2.
- Hughes GC, Swaminathan M, Wolfe WG. Reimplantation technique (David operation) for multiple sinus of Valsalva aneurysms. Ann Thorac Surg. 2006;82:14–6.
