Abstract
Background. The omega-3 index (eicosapentaenoic acid + docosahexaenoic acid) content in red blood cell membranes has been suggested as a novel risk marker for cardiac death. Objective. To assess the ability of the omega-3 index to predict all-cause mortality, cardiac death and sudden cardiac death following hospitalization with an acute coronary syndrome (ACS), and to include arachidonic acid (AA) in risk assessment. Material and methods. The omega-3 index was measured in 572 consecutive patients (median 63 years and 59% males) admitted with chest pain and suspected ACS in an inland Northern Argentinean city with a dietary habit that was essentially based on red meat and a low intake of fish. Clinical endpoints were collected during a 5-year follow-up period, median 3.6 years, range 1 day to 5.5 years. Stepwise Cox regression analysis was employed to compare the rate of new events in the quartiles of the omega-3 index measured at inclusion. Multivariable analysis was performed. Results. No statistical significant differences in baseline characteristics were noted between quartiles of the omega-3 index. The median of the adjusted omega-3 index was 3.6%. During the follow-up period, 100 (17.5%) patients died. Event rates were similar in all quartiles of the omega-3 index, with no statistical significant differences. AA added no prognostic information. Conclusion. In a population with a low intake of fish and fish oils, the adjusted omega-3 index did not predict fatal events following hospitalization in patients with acute chest pain and suspected ACS.
Introduction
The omega-3 index is defined as the percentage in red blood cell (RBC) membranes of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Citation1), the two most important long chain omega-3 fatty acids (FA) derived from fish. The index is an independent measure of the amount of omega-3 FA available in the body. Although it correlates highly with measurements made in whole blood, plasma, and serum (Citation1), its half-life is 4–6 times longer, reflecting the average intake over several weeks (Citation2,Citation3,Citation4). It reflects the amount of EPA + DHA in the phospholipid compartment of cellular membranes and may be a useful surrogate measure of the beneficial effects of the omega-3 FA.
Epidemiological data suggest that omega-3 FA derived from fish can reduce the incidence of cardiovascular disease (CVD) (Citation5,Citation6,Citation7), mainly due to a reduction of fatal cardiac events. It has also been demonstrated that patients with a high tissue ratio of omega-3/omega-6 FA have a reduced risk of coronary artery events (Citation8). A meta-analysis of randomized trials involving patients with cardiac disease showed that supplementation with the marine omega-3 fatty acids EPA and DHA reduced the rate of death from coronary heart disease (CHD) by 20% (Citation9) and this was mainly based on the results of the open GISSI-Prevenzione trial (Citation10) and JELIS trial (Citation11). By excluding these two studies, Kwaak et al. (Citation12) found insufficient evidence of a secondary preventive effect of omega-3 FA supplements in 14 randomized, double-blind, placebo-controlled trials involving 20485 patients with a history of CVD. Similar results were obtained in the recently published ORIGIN study (Citation13).
Data from randomized and observational studies regarding the effect of the omega-3 FA on the rate of cardiovascular events in populations with a very low intake of fish are lacking.
Omega-3 FA displays several beneficial cardiovascular properties, such as anti-atherothrombogenic, antiarrhythmic, anti-inflammatory and antihypertensive effects, and they also lower the triglyceride levels and increase the HDL levels (Citation14,Citation15). The anti-lipidemic properties are present in populations with a naturally high dietary intake of marine omega-3 FA (Citation15), but clinical effects in these populations are modest (Citation11).
In the present prospective observational study, we selected a population with low consumption of fish and high consumption of meat. From a dietary perspective, we included arachidonic acid (AA) in addition to the omega-3 index in our analyses.
The aim of our study was to search for a threshold level of the omega-3 index in relation to mortality [total mortality, cardiac death, and sudden cardiac death (SCD)] and to evaluate its relation to AA in a cohort of chest pain patients with suspected acute coronary syndrome (ACS) and a low dietary intake of fish.
Subjects and methods
Study subjects
This study was performed as a part of a major prospective, observational study termed “ARgentinean Risk Assessment Registry in ACS” (ARRA-RACS) (Ref. ClinicalTrial.gov identifier: NCT01377402), which was designed to identify early risk markers for all-cause mortality and cardiac death following hospitalization of patients with acute chest pain and suspected ACS. A total of 982 patients were recruited consecutively at nine centers in Salta, Argentina, from December 2005 until November 2009. To be considered eligible for the study, patients should be at least 18 years of age and should have provided a written informed consent. If the patient remained unconscious until death, consent was given by a close family member; the only exclusion criterion was previous inclusion in the same study cohort or participation in another clinical trial. The study was approved by the Ethics Committee appointed by the Board of Medical School of Salta and was conducted in accordance with the Helsinki Declaration of 1971, as revised in 1983. At two hospitals, the study was also required to be approved by a local ethics committee or institutional review board. The Norwegian biobank containing Argentinean blood samples was approved by the Regional Board of Research Ethics and the Norwegian health authorities.
Study design
At inclusion, we completed a case report form (CRF) including detailed clinical background information, use of medication, monthly intake of fish, fish oil supplementation and dietary intake, description of actual symptoms preceding the present hospitalization, and electrocardiographic findings at admission classified according to the presence of ST segment changes (Citation16). In the CRF, we also added relevant information obtained after hospitalization, such as coronary angiography, percutaneous coronary interventions (PCI), and coronary artery by-pass grafting (CABG).
During the follow-up period (median 3.6 years, range 1 day to 5.5 years), all-cause mortality, cardiac mortality, and SCD were recorded. Survivors were contacted by telephone to collect information with regard to new hospitalizations and vital status at 30 days, 6, 18, and 24 months, followed by annual interviews. A personal interview by a physician was performed one year from index admission. Moreover, the vital status of all the patients was monitored by means of a link to municipal and provincial registries. In the case of patients who died, the death certificate was obtained from the Civil Registry of the Province of Salta, and additional information on fatal events was obtained from hospitals and family members.
All-cause mortality was defined as the primary endpoint; cardiac- and sudden cardiac death as secondary endpoints. The definition of cardiac mortality included death preceded by a definitive myocardial infarction (MI) or chest pain lasting > 20 minutes without a given troponin T (TnT) (probable MI) or a history of ischemic heart disease and no other obvious cause of death. SCD was defined as unexpected death occurring in a short time period (generally within 1 hour of symptom onset), due to a cardiac cause in a person with known or unknown cardiac disease (Citation17).
Laboratory methods
Peripheral blood samples were drawn immediately following admission by direct venipuncture with a minimum of stasis of an antecubital vein. B-type natriuretic peptide (BNP) was analyzed in ethylene diamine tetraacetic acid (EDTA) plasma, whereas the analyses of TnT, creatinine, glucose, and lipids were performed in serum as part of the routine, with a repeated measurement of TnT approximately 6 hours after admission (Citation16). In case of increasing values, further TnT measurements were performed at less fixed intervals to confirm a typical diagnostic release pattern according to international guidelines (Citation18). Serum and EDTA plasma samples were prepared, stored, and shipped, as previously described (Citation16).
Preparation of RBC: After removing the plasma from EDTA blood following centrifugation, the RBC were washed once with 5 mL of 0.9% saline solution and then centrifuged at 1800 rpm for 8 min. The sediment containing RBC was stored in two tubes at ‐70°C after temporary storage at ‐20°C for 1 to 14 days. All RBC samples were transferred on dry ice in one shipment to VITAS laboratories, Oslo, Norway, for measurement of FAs.
Frozen RBC samples were thawed overnight in a refrigerator. Approximately 40 μL of wet red blood cells was transferred to a 1.8 mL GC vial using a pipette with wide opening. After a 3 second vortex mix, 900 μL methanolic HCL was added, followed by 3 second vortex mix and capping of the vial. Vials were then incubated at + 80°C with mixing at 1000 rpm for 2 hours. The vials were cooled and 500 μL hexane and 300 μL 3M KOH in water was gently added. After capping, shaking for 5 min and centrifugation for 5 min at 4000 rpm, 1 μL was injected by pulsed splitless injection on a GC-FID system (Agilent G7890A, Agilent Technologies, Waldbronn, Germany). Separation was performed on a SP-2380 (30 m × 0.25 mm i.d. × 0.25 μm film thickness) column from Supelco, USA. The following temperature program was used: initial temperature of 90°C held for 0.5 min, then increased by 50°C/min to 150°C, then increased by 10°C/min to 225°C, then increased by 120°C/min to 245°C and held for 3 min. The oven was cooled before the next injection. FAs were identified by comparison with known standards. An external standard containing known amounts of relevant FAMEs (fatty acid methyl esters) (Supelco 37 component FAME Mix, Supelco Bellafonte, USA) was included in each run to correct for differences in FA response factors. The individual FA was reported as weight percentage of total FAMEs and the omega-3 index given by the sum of EPA and DHA. The inter-assay coefficient of variation was <4%. To adjust to the analysis previously employed in a similar study performed in the southwestern coastal region of Norway (Citation19), C22:0, C24:0, C24:1, and unidentified peaks were removed from the denominator prior to the calculation of weight percentage. The AA/EPA + DHA ratio was based on the unadjusted values and introduced to reflect the balance between omega-6 and omega-3 in a nutritional perspective.
We analyzed 980 out of 982 RBC samples; one sample was missing and another was coagulated. Samples from 408 displayed signs of oxidation, leaving 572 patients available for the present evaluation. More precisely, the concentrations of the easily oxidizable polyunsaturated fatty acids (PUFAs) were not normally distributed as other FA, but showed a second distribution severely skewed to very low concentrations superimposed on the expected normal distribution for DPA (docosapentaenoic acid), strongly suggesting degradation with PUFA concentrations approaching zero in some samples.
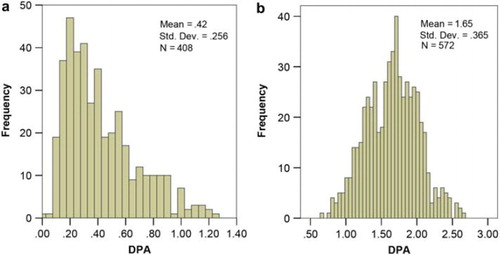
In order to discriminate between oxidized and non-oxidized samples we applied a k-means cluster analysis (SPSS 16.0, SPSS Inc. Chicago, IL, USA), by which we divided the material into 2 groups with respect to C22:6,n-3 (DHA), C22:5,n-3 (DPA), C20:5,n-3 (EPA), C22:4,n-6, C20:4,n-6 and C20:3,n-6. By taking all these FA into consideration in combination, the cluster analysis may be regarded as more objective and powerful as compared to the evaluation of only one of these fatty acids with respect to oxidation. The cluster analysis placed samples from 408 subjects in the oxidized group () and samples from 572 patients in the non-oxidized group with normal distribution of PUFAs ().
Statistical analyses
The patients were divided into quartiles according to their adjusted omega-3 index levels. Approximately, normally distributed variables were given as mean and standard deviation (SD) or as mean and 95% confidence interval (CI) of the mean, whereas variables with skewed distributions were given as median and quartiles. The Chi-square test for association was applied between omega-3 index quartiles and categorical variables at baseline. The one-way ANOVA test was used to test for equality of means of scale variables (e.g. age) amongst quartiles. Hazard ratios (HR) are presented with 95% CI. Stepwise Cox multivariable proportional hazards regression models with total death, cardiac and SCD death as the dependent variables and omega-3 index quartiles and other variables as potential independent predictors (listed below) were fitted. To examine the differences in prognosis between subjects in the upper versus the lowest quartile of the adjusted omega-3 index, we adjusted for age, sex, smoking, index diagnosis, diabetes mellitus, body mass index (kg/m2), congestive heart failure (CHF) (defined by Killip-Kimball class at admission, those patients in class 2 to 4 were classified as CHF patients and those in class 1 as non CHF), history of previous CHD (i.e. history of either angina pectoris, MI, CABG, or PCI), hypercholesterolemia/use of statins, baseline serum creatinine, BNP, and high sensitivity C-reactive protein (hsCRP) quartiles, triglycerides, HDL cholesterol, systolic and diastolic blood pressure, TnT > 0.01 ng/mL and beta-blockers prior to enrolment. The Kaplan-Meier product limits were used for plotting the times to event. The statistical analyses were performed using the statistical package SPSS version 19.0. All tests were two-sided with a significance level of 5%.
Results
Baseline characteristics
In our main analysis, we disregarded approximately 40% of the RBC samples due to the presence of oxidation, but patients from whom these samples were harvested, demonstrated baseline characteristics similar to those of the population under study (). An “intention-to-predict” analysis including all patients did not reveal any statistical differences in mortality between the quartiles of the omega-3 index.
Table I. Comparison of baseline characteristics in patients with and without oxidized samples.
In our main assessment of the 572 patients with non-oxidized samples, the mean(SD)% value of AA (C20:4,n-6) was 11.82(1.80)%, whereas the mean(SD)% of EPA, DHA, and DPA was 0.25(0.09)%, 2.57(0.74)%, and 1.65(0.37)%, respectively. The mean (SD)% of the omega-3 index was 2.81(0.79)%. After adjusting for C22:0, C24:0, C24:1, and unidentified peaks, the mean(SD)% of the omega-3 index increased to 3.58(0.99)%.
Baseline characteristics according to quartiles of the adjusted omega-3 index are given in . There was a predominance of men (59%), and the median age of the population was 63 years (ranging from 26 to 100 years). Except for smoking habits, there were statistically no significant differences in baseline characteristics between the adjusted omega-3 index quartiles.
Table II. Baseline characteristics for patient strata arranged according to quartiles of the adjusted omega-3 index (n = 572) at inclusion.
Follow-up
Patients were followed for a median period of 3.6 years, range 1 day to 5.5 years.
Dietary considerations
Sea fish intake of less than one meal per month or never was recorded in 51%, and a similar low intake of river fish was recorded in 50% of the population. As the proportion of omega-3 FA is very low in river fish, intake of sea fish and river fish were regarded separately (). Mortality related to diet is shown in .
Table III. Fish consumption in quartiles (Q) of the adjusted omega-3 index.
Table IV. Rate of total mortality, cardiac mortality, and sudden cardiac death (SCD) related to the frequency of meals with red meat, sea- and river fish, and chicken and eggs.
All-cause mortality
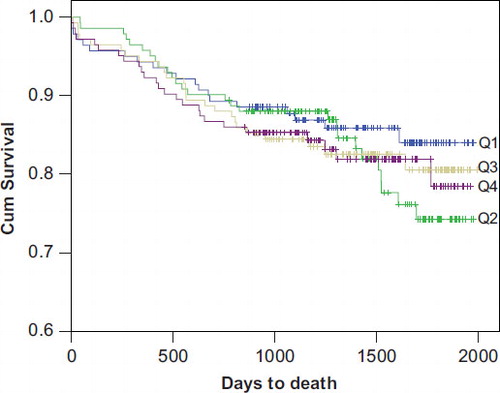
At final follow-up, 100 patients (17.5%) had died. The rate of death was found to be similar in all quartiles of the AA/EPA + DHA ratio (), and the prognostic utility was not improved by looking separately at the adjusted omega-3 index (). In the multivariable model for the five year follow-up data, HR (95% CI) for each of the three upper adjusted omega-3 index quartiles as compared to the lowest quartile (Q1) were non-significant; Q2: 0.89 (0.48–1.65), Q3: 0.80 (0.43–1.50), Q4: 0.73 (0.38–1.42), respectively. Only age, TnT > 0.01, level of creatinine, hsCRP quartiles, and systolic blood pressure at admission predicted total mortality. The Kaplan-Meier curves displayed a similar rate of all-cause mortality in all quartiles of the omega-3 index at final follow-up () with a non-significant log rank test (p = 0.789).
Table V. Events during 5 year follow-up, arranged according to the quartiles (Q) of the unadjusted AA/EPA + DHA ratio at inclusion.
Table VI. Events during 5-year follow-up, arranged according to the quartiles (Q) of the adjusted omega-3 index.
Cardiac death and SCD
At final follow-up, cardiac death occurred in 54 (9.4%) patients, of whom 35 (6.1%) were classified as SCD (). For the endpoints of cardiac death and SCD there were no significant reductions across quartiles. In the multivariate model for cardiac death, the HR (95% CI) in each of the three upper as compared to Q1 of the adjusted omega-3 index were Q2: 1.11 (0.47–2.63); Q3: 0.98 (0.40–2.36); Q4: 0.81 (0.32–2.06), respectively.
Omega-3 index in TnT positive patients
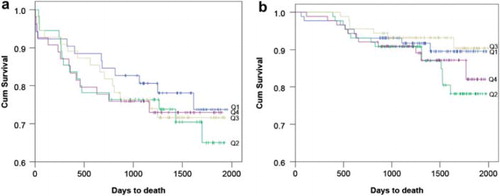
In the 218 patients admitted with TnT release, 59 (27.1%) patients had died during the 5-year follow-up period. In the multivariate analysis, we found no statistically significant difference when comparing each of the three upper quartiles to Q1 of the omega-3 index, and the HR (95% CI) for all-cause mortality were 0.48 (0.20–1.13) for Q2, 0.58 (0.25–1.35) for Q3, and 0.60 (0.25–1.45) for Q4, respectively ().
Table VII. Events during 5-year follow-up in troponin-T positive and negative patients, arranged according to the quartiles (Q) of the adjusted omega-3 index.
Omega-3 index in TnT negative patients
During the total follow-up period, 41 (11.6%) of 353 patients with negative TnT results had died. As for the other patient groups, the omega-3 index added no prognostic information in the TnT negative patients ().
Kaplan-Meier plots for the cumulative risk in quartiles of the omega-3 index for total mortality in TnT positive and negative patients are presented in , respectively.
Threshold assessment
Of the 572 patients with non-oxidized samples, 165 subjects had an omega-3 index above 4%. In this group there were 30 deaths. No statistically significant differences in HR were noted when comparing total death, cardiac mortality. and sudden SCD in patients with an omega-3 index above 4% to those below 4%. In the univariate analysis, the HR (95% CI) for total death in patients with an omega-3 index above 4% was 1.12 (0.73–1.72) and in the multivariate analysis it was 0.92 (0.56–1.52).
Discussion
We have assessed the prognostic utility of the omega-3 index in patients admitted with acute chest pain and suspected ACS, grouping the patients according to quartiles of the omega-3 index. After adjustment for potential confounders, there were no significant differences in the risk of all-cause mortality, cardiac death, or SCD between quartiles of the omega-3 index. Although quartiles are often preferred for these calculations, our results were confirmed in a stepwise Cox proportional hazards model, replacing adjusted omega-3 value quartiles by the individual values and including the same confounding variables [HR 0.87 (95% CI 0.67–1.11), p = 0.26].
No additional prognostic information was obtained by introducing the ratio between AA and omega-3 index in our risk assessment.
Ideally, the method by which the omega-3 index is measured should mainly extract fatty acids from the glycerophospholipid fraction, which is the main source of the polyunsaturated FA (Citation20). However, there may also be a release of FA predominantly carried in the sphingolipids, such as C22:0, C24:0 and C24:1, and their release will reduce the weight percentage of the omega-3 index as compared to an assay with less release of these long-chain fatty acids. In a previous study of a coastal Norwegian chest-pain population (Citation19), we used an assay with a negligible release of long chain fatty acids (HS-Omega-3 Index). In order to compare the two studies, we adjusted our present index levels by excluding the above mentioned long chain FA as well as unidentified FA from the formula. The measured median omega-3 index was 20% lower than the adjusted index.
Von Schacky and Harris (Citation2) previously demonstrated that an omega-3 index > 8% is associated with 90% less risk for SCD, as compared to an omega-3 index of < 4%. A retrospective case-control study from the US in ACS patients supports this proposed cut-off point (Citation21).
However, in the present study an interquartile threshold related to mortality could not be found. These results are in accordance with the results obtained in our coastal Norwegian chest-pain population (Citation19).
Our study population was recruited consecutively at nine private and public centers serving an inland population in Northern Argentina, an area in which the diet essentially contains meat and only minor amounts of fish or products derived from fish, and this explains the low levels of the omega-3 index in our population.
An assumption of a possible threshold related to clinical benefits of omega-3 FA is mainly based on studies (Citation22) of populations characterized by a higher intake of omega-3 than in the present study. A high background ingestion of omega-3 exceeding an assumed threshold may explain the results from studies demonstrating lack (Citation15,Citation23) or less benefit than expected (Citation11) of omega-3 supplementation. Therefore, we designed the present study to search for a threshold related to mortality in a quartile analysis of the omega-3 index in a chest pain population with a low intake of omega-3 FA.
We found no evidence of a threshold related to a worse outcome within the range of the adjusted omega-3 index. The median adjusted omega-3 index in the lowest as compared to the highest quartile was 2.5% and 4.8%, respectively, and an index level above 4% offered no cardiovascular protection.
As demonstrated by a recent meta-analysis (Citation24) and in other reports, omega-3 FA reduce the risk of SCD as well as fatal and nonfatal MI (Citation6,Citation25,Citation26). However, the strongest evidence of a beneficial effect of omega-3 FA on survival is so far related to SCD (Citation2,Citation27). As we did not observe a decline in SCD within our omega-3 index quartiles, we presume that their anti-arrhythmic effect is not expressed in secondary prevention following ACS in a population with a very low intake of omega-3 FA.
According to Mozzafarian and Rimm (Citation22), no further reduction in anti-arrhythmic events can be expected in a population already consuming 250–500 mg/d of EPA + DHA. In the present population in which the low frequency of fish meals was unrelated to the omega-3 quartiles and risk of death, these polyunsaturated FA are probably essentially derived from other sources, and the most common pathway would be the increased conversion from alpha-linolenic acid to DHA and EPA (Citation28).
Thus, estimates of fish intake would not apply to risk stratification in these chest-pain patients. We have shown that the median of 4.8% in the upper quartile of the omega-3 index in this Argentinean population is comparable to the median of 4.7% in the lowest quartile of the previously reported chest pain population from coastal Norway (Citation19). Therefore, we had expected that the Argentineans would display omega-3 levels below the protective anti-arrhythmic threshold of the omega-3 fatty acids, but there was no gradient related to SCD risk through the quartiles of the omega-3 index, irrespective of TnT release during the index event, suggesting that levels higher than 4% of the omega-3 index are needed for anti-arrhythmic protection.
There may be other factors required for a beneficial effect of omega-3 FA. Thus, the two most important studies showing a positive effect have been performed under special conditions. One of them, the GISSI Prevenzione trial (Citation10) was done in Italy where they in their daily diet have an extremely high intake of very potent antioxidants, particularly antioxidants from olive oil that protects the omega-3 FA from being oxidized in their bodies. The other major study important for the positive outcome of the meta-analyses of randomized trials involving patients with cardiac disease was the JELIS trial (Citation11) performed in Japan. This was not a regular study on omega-3 fatty acids, as their intake was combined with the use of statins. Statins have, in addition to their LDL-cholesterol reducing effect, powerful anti-inflammatory effects that probably in combination with omega-3 FA have effects that are quite different from those of omega-3 FA.
Limitations
Due to the high oxidation potential of red blood cells and their vulnerability to temperature changes, a k-means cluster analysis was applied to divide the patients into groups with and without the presence of oxidation. Using this method we cannot preclude the possibility of some degree of oxidation in the lower range of the omega-3 concentrations. However, all subtypes of omega-3, including DPA, have been accounted for in our analysis, supporting the quality of our data.
We assume that oxidation may essentially have occurred in vitro. However, the oxidation potential in our patient population has not been studied, and these Argentinean subjects may be prone to develop this phenomenon.
As a further control, sampling was repeated during follow-up (median 32, range 22–40 months following inclusion) in 20 arbitrarily selected patients with non-oxdized inclusion samples, employing optimized conditions (no washing of blood cells, immediate freezing at ‐70°C, addition of antioxidant), demonstrating persisting low omega-3 index levels, approximately 20% higher than at inclusion (unpublished data). Change to a healthier lifestyle can be expected in a population with a recent cardiac event, although a tapering of compliance to dietary advice may occur over time (Citation29).
Although oxidation was found to be present in approximately 40% of the total population, the remaining 60% were regarded as reliable, with a level of DPA (not included in the omega-3 index) approaching that of a Norwegian population in which the HS-Omega-3 index was measured (Citation27). Furthermore, in our Argentinean population, the mean (and median) level of unadjusted AA was 12% of total FA, far higher than our patient groups in coastal Norway, reflecting a high intake of meat. AA is also highly oxidizable, and its relative percentage supports the quality of our measurements.
However, the loss of 40% of the total patient population might introduce a bias in the interpretation of our results, but, fortunately, the baseline characteristics of patients with and without the presence of oxidation were found to be similar, supporting our conclusions. As the total patient sample was reduced due to the oxidation phenomenon, 42.2% of total deaths was lost, which has influenced the statistical power of our study.
We need to emphasize that we have studied the utility of the omega-3 index as a biomarker for future all-cause and cardiac death, and our results should not be extrapolated to those of an interventional study. Having said that, the 100 events observed in the study would provide a power of 80% at the two-sided 5% significance level to detect HR of 1.76 in a traditional equal allocation, two-parallel armed clinical trial. If the 73 deaths of patients with oxidized samples were included, the HR would be 1.53. The 46 events in the upper and lower quartiles of patients with non-oxidized samples would be enough to detect a HR of 2.29 with 80% power and 5% significance, an unrealistic figure in this setting. Although this analysis has low power (partly due to the loss of the oxidized samples), it does provide some guidance on the duration of follow-up needed to provide sufficient power in future analyses.
The prospective design, the absence of loss to follow-up, and the use of diagnostic biomarkers precludes other major sources of bias. Also, blood samples were collected immediately after admission and should therefore reflect the actual content of FA prior to hospitalization and the consequences of interventions and the disease in itself.
In conclusion, in a population with a very low intake of fish and fish oils, the omega-3 index did not predict future fatal events in patients with acute chest pain and suspected ACS.
Acknowledgments
We gratefully acknowledge the contribution by the participating medical doctors: Alejandro Farah (Hospital San Bernardo), Sebastian Saravia Toledo (CENESA), Sebastian Araujo (Hospital Privado Santa Clara de Asis), Pedro Kairuz (Hospital Militar), Fernando Marconetto (Sanatorio San Roque), Cesar Laspiur (Clinica San Rafael), Patricio Gallo (Sanatorio El Carmen), Fernando Rassi (Sanatorio Parque), Florencia Wayar (Clinica Guemes) and the service rendered by our devoted biochemical engineers Silvia Dib Ashur, Carolina Moreno Ten, Natalia Ruiz and Mariela Ponce. Furthermore, we appreciate the support of Professor Augusto Torino at the Favaloro Institute. Also, we wish to extend our gratitude to Ernesto Lovaglio MD, Maria José Aleman, and Valeria Choque for their coordinating service. We are also grateful for the facilities we used at the Catholic University of Salta.
In the non-Argentinean part of the study, we greatly value the contribution by our statistician Harry Staines PhD and by Heidi Grundt MD PhD who coordinated the database. Also, we highly appreciate the analytical work on the fatty acid analyses provided by Tore Bolstad.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Harris WS, von Schacky C. The omega-3 index: a new risk factor for death from coronary heart disease? Prev Med. 2004;39:212–20.
- Von Schacky C, Harris WS. Cardiovascular benefits of omega-3 fatty acids. Cardiovasc Res. 2007;73:310–5.
- Cao J, Schwichtenberg KA, Hanson NQ, Tsai MY. Incorporation and clearance of omega-3 fatty acids in erythrocyte membranes and plasma phospholipids. Clin Chem. 2006; 52:2265–72.
- Metcalf RG, James MJ, Gibson RA, Edwards JR, Stubberfield J, Stuklis R, et al. Effects of fish-oil supplementation on myocardial fatty acids in humans. Am J Clin Nutr. 2007;85:1222–8.
- Kromhout D, Bosschieter EB, de Lezenne Coulander C. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N Engl J Med. 1985;312:1205–9.
- Daviglus ML, Stamler J, Orencia AJ, Dyer AR, Liu K, Greenland P, et al. Fish consumption and the 30-year risk of fatal myocardial infarction. N Engl J Med. 1997;336:1046–53.
- Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetham PM, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989;2:757–61.
- Harris WS, Poston WC, Haddock CK. Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis. 2007;193:1–10.
- León H, Shibata MC, Sivakumaran S, Dorgan M, Chatterley T, Tsuyuki RT. Effect of fish oil on arrhythmias and mortality: systematic review. BMJ. 2008;337:a2931. doi: 10.1136/bmj.a2931.
- Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction; results of GISSI-Prevenzione trial. Lancet. 999;354:447–55.
- Yokohama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Japan EPA lipid intervention study (JELIS) investigators. Lancet. 2007; 369: 1090–8. Erratum in Lancet 2007;370:220.
- Kwaak SM, Myung SK, Lee YJ, Seo HG. Korean Meta-analysis Study Group. Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta-analysis of randomized, double-blind, placebo-controlled trials. Arch Intern Med. 2012;172:686–94.
- ,The ORIGIN trial investigatorsBosch J, Gerstein HC, Dagenais GR, Díaz R, Dyal L, Jung H,et al. N-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med. 2012;367:309–18.
- Grundt H, Nilsen DW. N-3 fatty acids and cardiovascular disease. Haematologica. 2008;93:807–12.
- Nilsen DWT, Albrektsen G, Landmark K, Moen S, Aarsland T, Woie L. Effect of a high-dose concentrate of n-3 fatty acids or corn oil introduced early after an acute myocardial infarction on serum triacylglycerol and HDL cholesterol. Am J Clin Nutr. 2001;74:50–6.
- León De La Fuente R, Naesgaard P, Nilsen ST, Woie L, Aarsland T, Gallo P, et al. B-type natriuretic peptide and high sensitive C-reactive protein predict 2-year all cause mortality in chest pain patients: a prospective observational study from Salta, Argentina. BMC Cardiovasc Disord. 2011;11:57. Available:http://www.biomedcentral.com/1471-–2261/11/57. Accessed 2011 Sep 29.
- Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–63.
- Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, et al. ESC Committee for Practice Guidelines (CPG). Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–45.
- Aarsetoey H, Pönitz V, Grundt H, Staines H, Harris WS, Nilsen DW. (n-3) Fatty acid content of red blood cells does not predict risk of future cardiovascular events following an acute coronary syndrome. J Nutr. 2009;139:507–13.
- Glaser C, Demmelmair H, Koletzko B. High-throughput analysis of fatty acid composition of plasma glycerophospholipids. J Lipid Res. 2010;51:216–21.
- Block RC, Harris WS, Reid KJ, Sand SA, Spertus JA. EPA and DHA in blood cell membranes from acute coronary syndrome patients and controls. Atherosclerosis. 2008;197:821–8.
- Mozzafarian D, Rimm EB. Fish intake, contaminants and human health: evaluating the risks and benefits. JAMA. 2006; 296:1885–99.
- Kromhout D, Giltay EJ, Geleijnse JM; Alpha Omega Trial Group. n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med. 2010;363:2015–26.
- Marik PE, Varon J. Omega-3 dietary supplements and the risk of cardiovascular events: a systematic review. Clin Cardiol. 2009;32:365–72.
- Leaf A, Albert CM, Josephson M, Steinhaus D, Kluger J, Kang JX, et al. Prevention of fatal arrhythmias in high-risk subjects by fish oil n-3 fatty acid intake. Circulation. 2005;112:2762–8.
- Albert CM, Hennekens CH, O’Donnell CJ, Ajani UA, Carey VJ, Willett WC, et al. Fish consumption and risk of sudden cardiac death. JAMA. 1998;279:23–8.
- Aarsetoey H, Aarsetoey R, Lindner T, Staines H, Harris WS, Nilsen DW. Low levels of omega-3 index are associated with sudden cardiac arrest and remain stable in survivors in the subacute phase. Lipids. 2011;46:151–61.
- Burdge GC, Calder PC. Conversion of a-linolenic acid to longer-chain polyunsaturated fatty acids in human adults. Reprod Nutr Dev. 2005;45:581–97.
- Ness AR, Ashfield-Watt PAL, Whiting JM, Smith GD, Hughess J, Burr ML. The long-term effect of dietary advice on the diet of men with angina: the diet and angina randomized trial. J Hum Nutr Diet. 2004;17:117–9.