Abstract
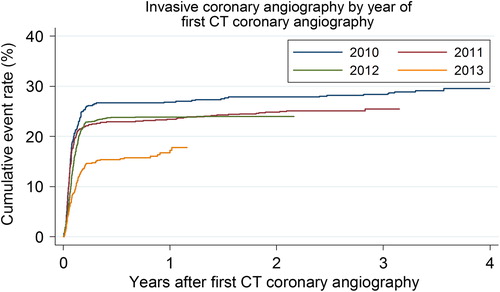
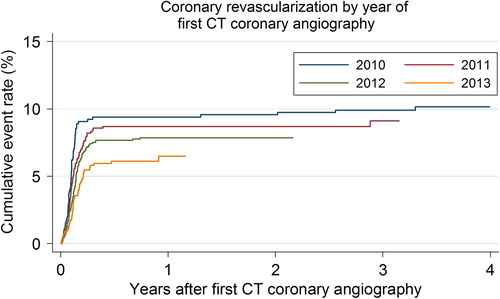
Objectives. We investigated whether any change in the use of invasive coronary angiography and coronary revascularisation after CT coronary angiography in patients with a low to intermediate pre-test probability of coronary artery disease could be explained from alterations in patient characteristics. Design. A cohort study based on data samples from the Western Denmark Heart Registry. Follow-up ended on 11 March 2014. Results. A total of 3541 persons were examined during the period of January 2010–December 2013. The median radiation dose was reduced from 4.2 to 2.2 mSv (p < 0.001) due to improved technology. The immediate referral rate for subsequent myocardial perfusion scans was increased from 2.8% to 10.0% (p < 0.001), while the immediate referral rate for invasive coronary angiography decreased from 25.3% to 10.8% (p < 0.001). The revascularisation rate diminished from 10.4% to 6.3%. The multivariable adjusted hazard ratio (95% confidence interval) for invasive coronary angiography during follow-up after CT coronary angiography was 0.59 (0.47–0.74) and that for coronary revascularisation was 0.66 (0.45–0.97) in 2013 compared to that in 2010. Conclusions: The radiation dose diminished considerably. The reductions in the use of invasive coronary angiography and coronary revascularisation could not be explained by changes in patient characteristics but are driven by an increased use of perfusion scans in combination with increasing use of measurement of functional coronary flow reserve.
Key words::
Introduction
Non-invasive visualisation of the coronary arteries has been compromised by heart motion, respirations and the small diameters of the vessels. However, the evolution of fast CT scanners with ECG synchronisation has made it possible to visualise the coronary arteries (Citation1). Studies have documented a better sensitivity and specificity of CT angiography compared to exercise ECG and myocardial perfusion scintigraphy when related to diameter stenosis as evaluated by invasive coronary angiography (Citation2,Citation3). CT coronary angiography has a high negative predictive value (Citation4–6). CT coronary angiography is therefore a useful diagnostic modality for excluding coronary heart disease in patients with a low to intermediate pre-test probability of coronary heart disease. CT coronary angiography is also useful in risk stratification by means of the coronary artery calcium score (Citation7). The finding of a high coronary calcium score always leads to supplementary investigations of the myocardial perfusion by nuclear or MR techniques or invasive coronary angiography depending on local practice and availability of diagnostic modalities (Citation8).
Because of difficulties in assessing whether coronary stenoses observed on CT scans are haemodynamically significant, it is often necessary to perform a supplementary diagnostic work up. Myocardial perfusion scintigraphy with pharmacological or exercise stress testing, MR perfusion with adenosine infusion, or invasive coronary angiography with measurement of functional coronary flow reserve are all valuable tools for adjudicating whether a stenosis should be treated with mechanical revascularisation to benefit the patient (Citation9,Citation10).
We examined the characteristics, radiation dose and subsequent use of perfusion scans, invasive coronary angiography, and revascularisation in persons who underwent a CT coronary angiography at our diagnostic centre. We also investigated whether any change in the use of invasive coronary angiography and coronary revascularisation after CT coronary angiography could be explained by the alterations in the patient characteristics.
Material and methods
Patient population, data source and study period
The patient population consists of all individuals with a low to intermediate pre-test probability of coronary artery disease admitted for their first CT coronary angiography at the Silkeborg Diagnostic Centre between 1 January 2010 and 31 December 2013, and reported to The Western Denmark Heart Registry. Demographics, vital status, clinical data as well as data related to the CT coronary angiography were sampled from the Western Denmark Heart Registry on 11 March 2014, which is also the date for end of follow-up. The study was approved by the Danish Data Protection Agency.
The Silkeborg Diagnostic Centre performed its first CT coronary angiography in 2007, and in that year, the first MR examination of the heart was performed in our centre. Both diagnostic modalities are implemented in close collaboration between radiologists and cardiologists. The present study period was chosen because of near-complete reporting to the Western Denmark Heart Registry from 1 January 2010 and because of a change from a 64-slice CT scanner to a 320-slice scanner in 2010.
CT technique
Patients were informed not to eat at least 2 hours before the examination and to avoid coffee, tea and tobacco. Patients were asked to take 50–100 mg of atenolol in the morning on the day of the examination. For those with contraindications against beta blockers, we used ivabradine 5–7.5 mg. If the heart rate exceeded 65 beats per minute during the examination, we added 2.5–20 mg metoprolol intravenously.
We used a 64 multislice spiral CT scanner (Philips Brilliance 64, Philips Medical System, Netherlands) until June 2010, and thereafter, a 320 multislice dynamisk volume CT scanner (Aquillion One, Toshiba Medical Systems, Japan) was used. This resulted in a shortening of the scan time. The new scanner also uses ECG-synchronised data sampling, which further reduces the radiation dose. The Toshiba scanner was upgraded from filtered back projection to iterative reconstruction and dose modulation in the summer of 2010. This resulted in a reduction in the radiation dose from a mean of 3.1 mSv to 2.7 mSv, which is a 14% reduction. In total, the shift in the CT scanner together with the mentioned upgrade resulted in a 50% reduction of the median radiation dose from 4.2 mSv to 2.2 mSv.
The CT coronary examination started with a calcium scan without contrast. This resulted in a coronary calcium score. Then, 800 μg of nitro-glycerine was administered sublingually to dilate the coronary arteries 2 min before the next scan. Then, a bolus of 60–90 ml of non-ionic contrast (Iomeron 350 mg/ml, Bracco Imaging Scandianavia AB) was administered at an infusion rate of 5–6 ml/sec via a cubical vein. CT recordings with and without contrast were obtained during breath holds of 10 s with simultaneous recording of the ECG. Subsequently, data were transferred to a Vitrea Advanced Workstation (Vital Images, USA). Coronary calcium was defined as an attenuation ≥ 130 Hounsfield Units. The coronary calcium score was estimated using the Vitrea Workstation using a calcium analysis program. A summed calcium score based on data from all coronary arteries, the Agatston score, was calculated in each patient. Contrast infusion was omitted when the Agatston score exceeded 1000. In that case, the patients were admitted for a perfusion scan or invasive coronary angiography.
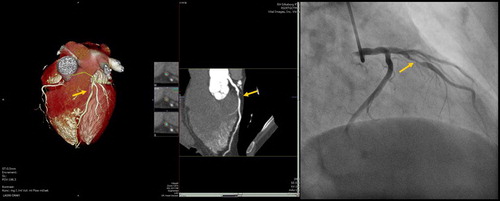
After a completed CT scan with contrast infusion, all coronary artery segments were reconstructed on a Vitrea Workstation (). The coronary arteries were classified as normal, non-obstructive (stenosis < 50%) or obstructive, if a stenosis was ≥ 50%.
Figure 1. Stenosis in the left anterior descending branch (arrow) diagnosed on CT coronary angiography (left) and invasive coronary angiography (right).
The CT coronary angiograms were analysed by cardiologists with level 2 certification (American Society of Cardiovascular CT Accreditation).
Statistical analysis
We used trend tests to examine any changes in demographics, clinical characteristics, CT angiographic, and follow-up data. Categorical variables are presented as percentages, and continuous variables are presented as the medians with 10th and 90th percentiles in brackets. For categorical data, we used tests for trends in a 2*c or r*c table and for continuous variables non-parametric correlation analysis. Data were analysed in Cox's proportional hazards regression models. The observation time was ended with an invasive coronary angiography or a coronary revascularisation, and observation time was censored by death, or end of follow-up, March 11th, 2014. The proportionality assumptions of the models were evaluated using Schoenfeld residuals and graphically. We considered p < 0.05 as statistically significant. All analyses were performed using Stata version 12.0, College Station, TX, USA.
Results
During the study period, 3541 patients with a median age of 60 years underwent a CT scan (). Fewer had diabetes mellitus and fewer had cholesterol lowering treatment during the study period. The proportion with a family history of ischaemic heart disease increased ().
Table I. Characteristics in relation to demographics, clinical data, CT coronary angiography, and follow-up.
Table II. Cox proportional hazard ratios with 95% confidence interval in brackets for the associations between year of CT coronary angiography and use of invasive coronary angiography and coronary revascularisation.
The radiation dose was halved. The use of perfusion scans increased, and fewer were submitted for invasive coronary angiography. We observed a decreasing revascularisation rate ().
and shows that the cumulative use of invasive coronary angiography and coronary revascularisation after CT coronary angiography decreased during the study period. The multivariable adjusted hazard ratio (95% confidence interval) for invasive coronary angiography after CT coronary angiography was 0.59 (0.47–0.74) and that for coronary revascularisation was 0.66 (0.45–0.97) in 2013 compared to 2010 ().
Discussion
Among the 3541 patients examined using CT coronary angiography in the period from 1 January 2010 and 31 December 2013, we found less diabetes mellitus, less use of cholesterol lowering treatment, but a higher proportion with a family history of ischaemic heart disease. The radiation dose was halved, the use of perfusion scans increased, and the use of invasive coronary angiography and revascularisation diminished considerably.
CT coronary angiography is a good diagnostic tool to exclude ischaemic heart disease in patients with a low to intermediate pre-test probability of ischaemic heart disease (Citation11–13). When severe proximally located stenosis is found, the patient is submitted to coronary angiography in an invasive centre that can deliver ad hoc revascularisation. When less severe coronary artery disease is found, a stress perfusion scan is recommended.
During the study period, functional diagnostics during coronary angiography in the form of measurement of fractional flow reserve for the classification of the haemodynamic significance of a coronary stenosis was implemented to determine the need for revascularisation (Citation14). This explains the increase in the use of perfusion scans, the reduced use of invasive coronary angiography and, as a consequence, the reduction in the revascularisation rate. This occurred late in the study period because the clinical significance of fractional flow reserve measurement was first recognised and published during the third year of our study period (Citation14). This lead to a gradual shift towards an increased use of perfusion scans and also a greater availability of such scans for diagnostic purposes.
The total radiation exposure for a complete diagnostic work up may increase as a consequence of the increased use of perfusion scans before an invasive coronary angiography. The radiation dose may also increase during invasive coronary angiography because of the measurement of fractional flow reserve, which depends on fluoroscopic guiding of the catheter position. However, in our institution, we prefer the use of MR perfusion scans when possible to avoid radiation exposure.
It is still unknown whether the sequence of diagnostic evaluation is optimal. A MR perfusion scan could be used as the first line investigation because the MR technique does not expose patients to X-rays. MR perfusion puts demands on resources and could therefore be restricted to very young patients where radiation is a concern. Perfusion tests should also be considered the first-line diagnostic evaluation in patients with revascularised coronary heart disease and uncharacteristic symptoms suggestive of recurrent angina (Citation15).
Strengths and weaknesses
When using the Danish National Registry of Patients as a reference, the completeness of reporting to The Western Denmark Heart Registry is high (personal communication, Linda Aagaard Rasmussen, daily leader of Western Denmark Heart Registry). A high patient volume yields good statistical power for the detection of even minor trends over time.
We cannot exclude selective admission to our centre. Truncation of observation time leads to an underestimation of the revascularisation rate among those examined late in the study period.
We have not examined economic impact on the health care system or society of the implementation of CT coronary angiography. However, a recent systematic review showed that CT coronary angiography may be cost-effective in chest pain patients with a low to intermediate risk of coronary heart disease (Citation16). Furthermore, patients who can be evaluated non-invasively have fewer complications than seen with invasive coronary angiography (Citation16).
In Central Region Denmark, we observed an increasing use of all diagnostic modalities such as CT coronary angiography, invasive coronary angiography, and myocardial perfusion scans during the study period, but a decreasing revascularisation rate per invasive coronary angiography (unpublished data, The Western Denmark Heart Registry). Our single centre findings oppose these finding, because the use of invasive coronary angiography decreased. We expect to see a drop in use of invasive coronary angiography in our region in the near future because of the implementation of guideline recommended use of non-invasive testing as gatekeeper to invasive coronary angiography in patients with a low to intermediate pre-test probability of having stable coronary artery disease.
Our findings can be of value for diagnostic centres that already have CT coronary angiography or plan to incorporate it into their diagnostic armamentarium.
Acknowledgments
Leif Spange Mortensen M.Sc., is thanked for critical evaluation of the manuscript.
Declaration of interest: The authors report no declarations of interest. The authors alone are responsible for the content and writing of the paper.
References
- Hassan A, Nazir SA, Alkadhi H. Technical challenges of coronary CT angiography: today and tomorrow. Eur J Radiol. 2011;79:161–71.
- Abdulla J, Abildstrom SZ, Gotzsche O, Christensen E, Kober L, Torp-Pedersen C. 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J. 2007;28:3042–50.
- Gaudio C, Pelliccia F, Evangelista A, Tanzilli G, Paravati V, Pannarale G, et al. 320-row computed tomography coronary angiography vs. conventional coronary angiography in patients with suspected coronary artery disease: a systematic review and meta-analysis. Int J Cardiol. 2013;168:1562–4.
- Mowatt G, Cook JA, Hillis GS, Walker S, Fraser C, Jia X, Waugh N. 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. Heart. 2008;94:1386–93.
- Stein PD, Yaekoub AY, Matta F, Sostman HD. 64-slice CT for diagnosis of coronary artery disease: a systematic review. Am J Med. 2008;121:715–25.
- Ko BS, Wong DT, Cameron JD, Leong DP, Leung M, Meredith IT, et al. 320-row CT coronary angiography predicts freedom from revascularisation and acts as a gatekeeper to defer invasive angiography in stable coronary artery disease: a fractional flow reserve-correlated study. Eur Radiol. 2014;24:738–47.
- Sharma RK, Sharma RK, Voelker DJ, Singh VN, Pahuja D, Nash T, Reddy HK. Cardiac risk stratification: role of the coronary calcium score. Vasc Health Risk Manag. 2010;6:603–11.
- Youssef G, Kalia N, Darabian S, Budoff MJ. Coronary calcium: new insights, recent data, and clinical role. Curr Cardiol Rep. 2013;15:325.
- Rochitte CE, George RT, Chen MY, Arbab-Zadeh A, Dewey M, Miller JM, et al. Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J Epub. 2014;35:1120–30.
- Donati OF, Scheffel H, Stolzmann P, Baumüller S, Plass A, Leschka S, Alkadhi H. Combined cardiac CT and MRI for the comprehensive workup of hemodynamically relevant coronary stenoses. AJR Am J Roentgenol. 2010;194:920–6.
- Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003.
- Nasis A, Leung MC, Antonis PR, Cameron JD, Lehman SJ, Hope SA, et al. Diagnostic accuracy of noninvasive coronary angiography with 320-detector row computed tomography. Am J Cardiol. 2010;106:1429–35.
- Pelliccia F, Pasceri V, Evangelista A, Pergolini A, Barillà F, Viceconte N, et al. Diagnostic accuracy of 320-row computed tomography as compared with invasive coronary angiography in unselected, consecutive patients with suspected coronary artery disease. Int J Cardiovasc Imaging. 2013;29:443–52.
- De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991–1001.
- Kohsaka S, Makaryus AN. Coronary angiography using noninvasive imaging techniques of cardiac CT and MRI. Curr Cardiol Rev. 2008;4:323–30.
- Zeb I, Abbas N, Nasir K, Budoff MJ. Coronary computed tomography as a cost-effective test strategy for coronary artery disease assessment - a systematic review. Atherosclerosis. 2014;234:426–35.