Abstract
Objective. To determine the risk in administering β-blockers, contrast-induced nephropathy (CIN) and the trend in X-ray use, during coronary computed tomography angiography (CCTA). Methods. A total of 416 patients were referred for elective CCTA. To achieve a resting heart rate below 60 beats per minute, oral and/or intravenous β-blockers were administered. Using questionnaires, information on the adverse effects of β-blockers was collected from the patients. The levels of s-creatinine and estimated GFR (eGFR) were measured before and after contrast enhanced CCTA. Radiation exposure was compared with the exposure 3 years earlier. Results. There was no significant difference in the symptoms (dizziness, lipothymia and palpitations) between patients with and patients without β-blocker pretreatment. Compared to baseline values, the decrease in s-creatinine was not significant (75.2 vs. 74.6 μmol/L, p = 0.09), while the increase in eGFR was not significant (78 vs. 79 mL/min, p = 0.17). Also, subgroups of patients with hypertension, hypercholesterolemia, diabetes or pre-existing slight impairment in renal function did not develop CIN. The mean radiation exposure decreased from 17.5 to 6.7 mSv, p < 0.0001. Conclusions. In terms of the side effects of β-blockers and contrast media, there were no short term complications to CCTA. Furthermore, the radiation dose has been dramatically diminished over the last three years.
Introduction
Coronary computed tomography angiography (CCTA) is commonly used to assess the anatomy of the coronary arteries in relation to atherosclerosis and the diagnostic workup of angina pectoris (Citation1). The ability of CCTA to rule out coronary artery stenosis with a high negative predictive value is very good in patients with atypical symptoms of angina pectoris (Citation2), and the patients prefer CCTA over invasive coronary angiography (ICA) (Citation3). However, the positive predictive value is rather low (Citation1). Presently, ICA is the gold standard in investigation for the diagnosis and description of the coronary arteries. However, it is an expensive and resource consuming procedure, associated with rare but serious adverse events (Citation1,Citation4).
The use of intravenously administered contrast media may cause contrast-induced nephropathy (CIN). It is commonly accepted that patients with a pre-existing normal renal function are less likely to develop CIN but concerns exist regarding patients with comorbidities and pre-existing renal impairment, especially in relation to diabetic nephropathy (Citation5,Citation6). To avoid motion artifacts and obtain the best image quality for CCTA, the resting heart rate can be lowered with the administration of β-blockers, either orally or intravenously (Citation7). β-blockers have a number of well documented adverse effects. Finally, concerns do exist regarding the axiomatic effects on the DNA from radiation exposure (Citation8), giving rise to worries regarding radiation-induced cancer.
This study assesses the short and long term risks associated with CCTA, in relation to 1) the development of CIN, 2) the side effects from β-blocker treatment and 3) the proportion of radiation exposure.
Material and methods
Patient selection
A total of 416 consecutive ambulatory patients who presented between September 2010 and September 2011, and were scheduled for CCTA due to symptoms of angina pectoris and without known CAD were included; patients with irregular heart rhythm (including atrial fibrillation), dyspnea at the time of the CCTA, left ventricular ejection fraction below 30% or s-creatinine above 140 μmol/L were excluded from this study. Diabetes mellitus was defined as the use of anti-diabetic medication and a slightly impaired renal function was present in case of an estimated GFR (eGFR) < 60 mL/L.
Patient preparation
If the patients were thirsty before the scanning procedure, they were asked to drink a glass of water. To achieve a resting heart rate below 60 beats per minute (bpm), most patients were pretreated with an oral dose of metoprolol tartrate: two days before the scan, the patients received 50 mg, the day before and on the day of the CCTA the patients received 100 mg of metoprolol. If the heart rate before the scan remained above 60 bpm, metoprolol tartrate was intravenously given in increments of 5 mg, repeated every minute (a maximum of 50 mg) until the heart rate was appropriate. The day after CCTA, the patients received an oral dose of metoprolol tartrate 50 mg.
CCTA scanning
All scans were performed with a 64-slice CT-scanner (Discovery VCT, GE Healthcare). The scan was performed with the following parameters: gantry rotation time 350 ms, 64 × 0.625 mm collimation, prospective or retrospective gating depending on heart rate, 120 kV tube voltage and max 600 mA tube current. The scanner's field of view was adjusted to include the heart, from the carina to just below the diaphragm. The scan was divided into two phases: initially, a non-contrast scan was performed to measure the Agatston score (Citation9). Secondly, a contrast-enhanced scan was obtained by injecting a dose of 90 ml of iopromide 370 mg/mL (Ultravist, Bayer HealthCare) in the antecubital vein at a flow rate of 5 mL/s. The scan data was acquired when contrast appeared in the aortic root, while the patient was asked to hold an inspiratory breath. The radiation exposure was estimated using dedicated software (GE Healthcare), and translated to mSv (conversion factor of 0.014) (Citation10). Two experienced observers independently evaluated the CCTA dataset using dedicated software (CardiQ Xpress, GE) and an offline workstation (AW4.3, GE). Coronary stenosis was defined as significant with a luminal diameter reduction of ≥ 50%.
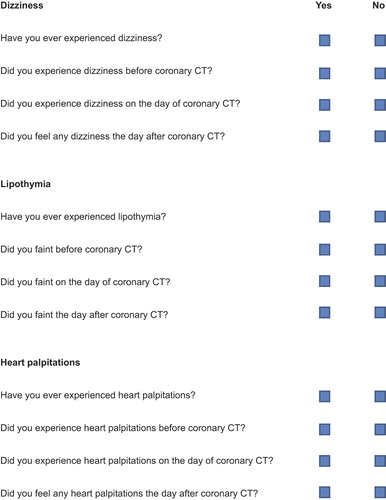
Adverse effects of β-blockers
On the day of CCTA, a written questionnaire regarding the adverse effects of β-blockers was handed to the patients (). In this questionnaire, the patients were asked whether they had ever experienced dizziness, lipothymia and palpitations. The patients were questioned on whether they had experienced any of these symptoms the day before CCTA, the day of CCTA or the day after CCTA. The patients were requested to return the questionnaires to the department within 14 days after CCTA. No reminder was sent to non-responders. Patients reporting dizziness, lipothymia or palpitations prior to pretreatment with β-blockers were excluded, since these symptoms were considered habitual rather than adverse effects of β-blockers.
Contrast-induced nephropathy
Patients suffering from acute CIN within 48 h after CCTA were not the target in this study. The intention was to obtain s-creatinine and eGFR within one month before and two months after CCTA. If the follow-up blood samples were not obtained within two months after the CCTA, the patients were not reminded. In the statistical analyses, values of s-creatinine and eGFR obtained within 30 days before and 60 days after CCTA were compared. CIN was defined as a post-procedural increase above 25% of baseline s-creatinine (Citation11).
Radiation exposure
To evaluate changes in the radiation dose, a total of 109 stable patients scheduled for elective CCTA at clinical indication from August 2007 until January 2008, were included for comparison (Citation12). In this first period, 120 kV was used and retrospective gating was applied in all examinations. The patients’ mean BMI was 27.4 kg/m2 and the mean heart rate was 64 bpm.
Follow-up
In September and October 2012, all 416 patient files were studied independently by two observers gathering data regarding admissions due to any cardiac conditions (including lipothymia, acute coronary syndrome, ICA, percutaneous coronary intervention or coronary artery bypass graft), development of nephropathy, or death.
Statistical analysis
Data was presented according to type, that is descriptive statistics for continuous variables comprised of mean and standard deviation (SD), whereas categorical variables were displayed by frequencies and the corresponding percentages. Comparisons were carried out using the two-sample t-test, Pearson's x2 test or Fisher's Exact test, as appropriate. All computer entries were performed by two observers and validated with additional random sampling. Analyses were performed in STATA 13.0 (StataCorp, Texas, USA).
Results
Initially, 416 subjects were enrolled into the study, of which 201 (48%) were male. The average age of the patients was 57 (SD ± 11; min-max 29–87) years. The mean body mass index was 26.7 (± 4; 17.8–42.1) kg/m2, and prior to the CCTA, the mean heart rate was 65 (± 12; 30–141) bpm (). In total, 289 (69%) had medically treated hypertension or systolic blood pressure above 140 mmHg on the day of examination. Due to a high Agatston score (n = 30), an increased or irregular heart rate (n = 7) or the lack of intravenous access (n = 1), a total of 38 (9%) patients were excluded. A contrast CCTA was performed in 378 (91%) patients. In 38 patients the CCTA showed significant stenosis.
Table I. Characteristics of participants.
β-blocker
In total, 355 (85%) patients had pretreatment with β-blockers. In 258 (62%) patients, pretreatment with oral metoprolol tartrate was given and in 118 of these, additional intravenous metoprolol tartrate was administrated immediately before the CCTA. In 97 (22%) patients, only intravenous metoprolol tartrate was administered as pretreatment. A total of 58 (14%) patients did not receive any pretreatment with β-blockers at all. Information regarding the β-blocker pretreatment was missing in three patients (1%). After pretreatment, the mean heart rate during CCTA was significantly lower in the pretreated patients (60 (± 8) bpm vs. 63 (± 16) bpm; p = 0.02).
Questionnaires addressing potential adverse effects to β-blocker pretreatment were available in 248 patients (216 pretreated and 32 non-pretreated) corresponding to a response rate of 60%. The response rate among patients with diabetes mellitus, hypertension or hypercholesterolemia was 65%. Of the 216 pretreated patients, 26 (12%) reported dizziness, lipothymia or palpitations, while five (16%) of the 32 patients who did not receive β-blocker therapy experienced these symptoms (p = 0.4). With respect to the individual adverse effects (dizziness, lipothymia or palpitations), no significant differences were observed between treated and non-treated patients (). Also, none of the 416 patients scheduled for CCTA were readmitted to hospital due to side effects of β-blocker pretreatment.
Table II. Possible side effects of β-blocker pretreatment.
Renal function
The contrast media were administered in 378 patients and the median dose was 94 mL (SD ± 17; min-max 90–190) mL. The values of s-creatinine and eGFR within one month prior to the CCTA and 2 months after the CCTA were available in 319 patients and 279 patients respectively, and 273 patients had both measurements. There was a non-significant decrease in the s-creatinine level and a non-significant increase in eGFR (). CIN was observed in only one patient, with an increase in s-creatinine from 79 to 100 μmol/L, and a decrease in eGFR from 87 to 66 mL/min. This patient did not have diabetes mellitus, but was undergoing lipid-lowering and antihypertensive treatment with a statin and a calcium-channel-inhibitor. Patients with diabetes mellitus (n = 20) and patients with pre-existing impaired renal function (n = 16) had a significant decrease in s-creatinine level and an improvement in eGFR. None of the 378 patients were hospitalized after CCTA or during the follow-up due to allergic reactions to contrast, nephropathy or the need for hemodialysis.
Table III. Baseline post-procedural levels of s-creatinine and eGFR.
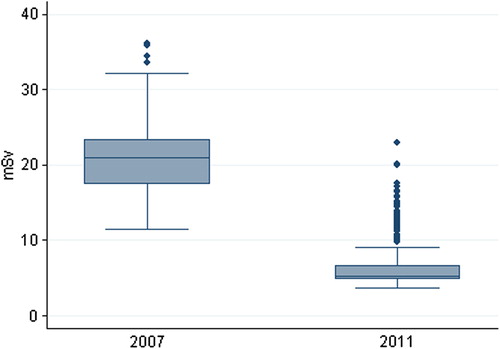
Radiation exposure
The mean radiation exposure was 6.7 (SD ± 3.3; min-max 3.7–22.9) mSv, and 12 (3%) patients were exposed to doses > 15 mSv. In 302 of the 378 patients, a prospective gating was applied with a mean dose of 5.3 mSv, while 13.1 mSv was used in the retrospective examinations. The mean radiation dose in the 109 patients examined in August 2007 until January 2008 was significantly higher, 17.5 mSv (± 5.0; 8.6–32.4) (p < 0.0001), .
Figure 2. Box plot of radiation exposure. The box represents the 25th and 75th percentile; the middle line represents the median and the peripheral lines extend to the outer fences which are 1.5 times the interquartile range below and above the 25th and 75th percentile, respectively. The dots are outliers.
Discussion
In this study, CCTA, including contrast media and pretreatment with β-blocker, was well tolerated. There were no significant differences between baseline and post CCTA levels of s-creatinine and eGFR-also in the subgroup of patients with diabetes and impaired renal function, and β-blockers were not associated with any adverse effects. Our data indicate that over time, the radiation doses used for contrast CCTA have been reduced.
β-blocker
Prior CCTA pretreatment with β-blockers is recommended if the heart rate is too high (Citation7). However, the consequences of this pretreatment, in particular intravenously administered β-blockers, are not well documented (Citation13–15). In these three studies, metoprolol (5–15 mg), metoprolol (5–20 mg) and atenolol (5–10 mg) were well tolerated. In our study, the administration of a higher dose of metoprolol (a maximum of 50 mg) was tolerated and showed no signs of immediate harm or any side effects the following day. In agreement with the prior studies, we found no significant difference in the symptoms (dizziness, lipothymia and palpitations) between patients with β-blocker pretreatment and patients without β-blocker pretreatment. The β-blockers have a well-known negative inotropic effect and might be contraindicated. In this case, an alternative is Ivabradine, and several studies have demonstrated Ivabradine to be effective in reducing the heart rate before CCTA with no significant effect on the depression of blood pressure (Citation16,Citation17).
Contrast induced nephropathy
In previous studies, the need for dialysis due to CIN ranged from 30 days and at least up until 45 days after contrast media infusion (Citation18,Citation19). Therefore, we evaluated s-creatinine and eGFR levels measured within two months after CCTA. In patients receiving contrast media, with both baseline and follow-up measurements available, there were no significant changes in s-creatinine and eGFR in the tests prior to and post CCTA. These observations support the results of older as well as more recent studies and meta-analysis(Citation5,Citation6,Citation20–22). Recent studies indicate that patients developing serious renal failure and death often have comorbidity such as hypertension and diabetes (Citation23). In our study, none of the patients developed renal failure, despite comorbidities such as diabetes (n = 20), pre-existing slightly impaired renal function (n = 16), hypertension (n = 169) or hypercholesterolemia (n = 108) within a follow-up period of more than two years. The improvement in renal function in patients with diabetes and pre- existing slightly impaired renal function may be of limited clinical relevance and could be “change finding” or “regression towards the mean” (if a variable is extreme on its first measurement, it will tend to be closer to the average on its second measurement). Nevertheless contrast media did not impair the renal function in these patients.
Radiation exposure
No extensive studies are available involving medically exposed adult cohorts, but a commonly quoted estimate for excess cancer mortality from radiation exposure is 1 death per 2000 scans (Citation24). Children and young women are especially vulnerable to radiation exposure since they have many years left to accumulate further radiation doses and develop cancer (Citation8,Citation25). Patients in this study were middle-aged (mean 57 years) and therefore did not have a particularly high risk of developing radiation-induced cancer. Nevertheless, radiation exposure at our centre has been reduced vigorously with the ongoing development of CT technology like the use of prospective ECG-gating. This is in agreement with a recent study in which prospective ECG-gating reduced the radiation dose by 69% compared to the formerly used retrospective ECG-triggered scan (Citation26). Further progress due to fast acquisition and iterative reconstruction has been made (Citation2,Citation27) and recent studies conclude that CCTA can be performed at an ultra-low radiation dose < 1 mSv without compromising the diagnostic image quality (Citation28,Citation29).
Limitations
There was a lack of compliance or motivation from the patients regarding blood tests and the questionnaires. Only in 273 (72%) patients were sufficient data on s-creatinine and eGFR prior to and after the contrast CCTA available. However, a comprehensive audit of all patient files unveiled no cases of renal failures. Also, the response rate of the questionnaires was only 60%, thus the data might not be representative due to a selection bias. Responders may have been motivated if they were suffering from dizziness, lipothymia or palpitations, thus leading to an overestimation of adverse effects of β-blockers.
Conclusion
CCTA has become a very useful non-invasive imaging modality in the diagnostic workup of angina pectoris. The administration of β-blockers in relation to CCTA seems to be harmless, both in relation to oral administration days before and intravenous administration as bolus immediately prior to CCTA. Comparable with recent studies, our data suggest that the risk of CIN in relation to CCTA might have been exaggerated and our study demonstrated no increased risk of CIN despite comorbidities such as diabetes, hypertension or hypercholesterolemia. Radiation exposure in relation to CCTA has been reduced remarkably during the last decade and further reduction is to be expected.
Declaration of interest: The authors report no declarations of interest. The authors alone are responsible for the content and writing of the paper.
References
- Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34: 2949–3003.
- Soon K, Wong C. Coronary computed tomography angiography: a new wave of cardiac imaging. Intern Med J. 2012; 42:22–9.
- Sandgaard NC, Diederichsen AC, Petersen H, Hoilund-Carlsen PF, Mickley H. Patients’ views of cardiac computed tomography angiography compared with conventional coronary angiography. J Thorac Imaging. 2012;27: 36–9.
- Arora N, Matheny ME, Sepke C, Resnic FS. A propensity analysis of the risk of vascular complications after cardiac catheterization procedures with the use of vascular closure devices. Am Heart J. 2007;153:606–11.
- Katzberg RW, Newhouse JH. Intravenous contrast medium-induced nephrotoxicity: is the medical risk really as great as we have come to believe? Radiology. 2010;256:21–8.
- McDonald JS, McDonald RJ, Comin J, Williamson EE, Katzberg RW, Murad MH, Kallmes DF. Frequency of acute kidney injury following intravenous contrast medium administration: a systematic review and meta-analysis. Radiology. 2013;267:119–28.
- Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010;121:2509–43.
- Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med. 2007;357: 2277–84.
- Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32.
- Khan A, Khosa F, Nasir K, Yassin A, Clouse ME. Comparison of radiation dose and image quality: 320-MDCT versus 64-MDCT coronary angiography. AJR Am J Roentgenol. 2011;197:163–8.
- Slocum NK, Grossman PM, Moscucci M, Smith DE, Aronow HD, Dixon SR, et al. The changing definition of contrast-induced nephropathy and its clinical implications: insights from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2). Am Heart J. 2012; 163:829–34.
- Diederichsen AC, Petersen H, Jensen LO, Thayssen P, Gerke O, Sandgaard NC, et al. Diagnostic value of cardiac 64-slice computed tomography: importance of coronary calcium. Scand Cardiovasc J. 2009;43:337–44.
- Roberts WT, Wright AR, Timmis JB, Timmis AD. Safety and efficacy of a rate control protocol for cardiac CT. Br J Radiol. 2009;82:267–71.
- Jimenez-Juan L, Nguyen ET, Wintersperger BJ, Moshonov H, Crean AM, Deva DP, et al. Failed heart rate control with oral metoprolol prior to coronary CT angiography: effect of additional intravenous metoprolol on heart rate, image quality and radiation dose. Int J Cardiovasc Imaging. 2013;29:199–206.
- Maffei E, Palumbo AA, Martini C, Tedeschi C, Tarantini G, Seitun S, et al. “In-house” pharmacological management for computed tomography coronary angiography: heart rate reduction, timing and safety of different drugs used during patient preparation. Eur Radiol. 2009;19:2931–40.
- Pichler P, Pichler-Cetin E, Vertesich M, Mendel H, Sochor H, Dock W, Syeda B. Ivabradine versus metoprolol for heart rate reduction before coronary computed tomography angiography. Am J Cardiol. 2012;109:169–73.
- Celik O, Atasoy MM, Erturk M, Yalcin AA, Aksu HU, Diker M, et al. Comparison of different strategies of ivabradine premedication for heart rate reduction before coronary computed tomography angiography. J Cardiovasc Comput Tomogr. 2014;8:77–82.
- Liss P, Persson PB, Hansell P, Lagerqvist B. Renal failure in 57 925 patients undergoing coronary procedures using iso-osmolar or low-osmolar contrast media. Kidney Int. 2006;70:1811–7.
- Mitchell AM, Jones AE, Tumlin JA, Kline JA. Incidence of contrast-induced nephropathy after contrast-enhanced computed tomography in the outpatient setting. Clin J Am Soc Nephrol. 2010;5:4–9.
- Cramer BC, Parfrey PS, Hutchinson TA, Baran D, Melanson DM, Ethier RE, Seely JF. Renal function following infusion of radiologic contrast material. A prospective controlled study. Arch Intern Med. 1985;145:87–9.
- Heller CA, Knapp J, Halliday J, O’Connell D, Heller RF. Failure to demonstrate contrast nephrotoxicity. Med J Aust. 1991;155:329–32.
- Bansal GJ, Darby M. Measurement of change in estimated glomerular filtration rate in patients with renal insufficiency after contrast-enhanced computed tomography: a case- control study. J Comput Assist Tomogr. 2009;33:455–9.
- Mitchell AM, Kline JA. Contrast-induced nephropathy: doubts and certainties. Acad Emerg Med. 2012;19: 1294–6.
- Berrington de GA, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, et al. Projected cancer risks from computed tomographic scans performed in the United States in2007. Arch Intern Med.2009;169:2071–7.
- Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007; 298:317–23.
- Hausleiter J, Meyer TS, Martuscelli E, Spagnolo P, Yamamoto H, Carrascosa P, et al. Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography: the multicenter, multivendor, randomized PROTECTION-III study. JACC Cardiovasc Imaging. 2012;5:484–93.
- Achenbach S, Marwan M, Ropers D, Schepis T, Pflederer T, Anders K, et al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J. 2010;31:340–6.
- Chen MY, Shanbhag SM, Arai AE. Submillisievert median radiation dose for coronary angiography with a second- generation 320-detector row CT scanner in 107 consecutive patients. Radiology. 2013;267:76–85.
- Fuchs TA, Stehli J, Bull S, Dougoud S, Clerc OF, Herzog BA, et al. Coronary computed tomography angiography with model-based iterative reconstruction using a radiation exposure similar to chest X-ray examination. Eur Heart J. 2014;35:1131–6.