Introduction
A scar is a mark that remains after the healing of a wound or other morbid processes. In the past, treatment was mainly focused on severe scarring, such as the hypertrophic and burn scars. However, scars from relatively minor wounds can also be stressful. In a recent survey, patients were found to be highly concerned about scars that follow routine surgical procedures, with many expressing their strong desire for scar prevention (Citation1).
Despite the wide interest in surgical scar prevention, there is as yet no universal consensus on optimal treatment. In this pilot study, we examined the effect of the 595-nm pulsed dye laser (PDL) and ablative 2940-nm Er:YAG fractional laser (EYFL) on fresh surgical scars using analysis of clinical photographs and patients’ rate of satisfaction.
Methods
Our case series included 12 patients (four men, eight women; aged 27–65 years; Fitzpatrick skin types III and IV) with post-thyroidectomy scars performed by one surgeon using the same surgical procedures (). Two patients had a history of keloids. The study was approved by the Institutional Review Board of the Catholic Medical Center, and the patients gave written informed consent before enrollment.
Table I. Patients’ characteristics and scar assessment.
Treatment consisted of three sessions of 595-nm PDL (Vbeam®; Candela Corp., Wayland, MA, USA) every month, starting from suture removal day (7–10 days after the operation). This was followed by three sessions of ablative 2940-nm EYFL (ProFractional Therapy™; Sciton Inc., Palo Alto, CA, USA), each 4 weeks apart. The PDL operated at a fluence of 4.0 J/cm2, 10-mm spot size, pulse duration of 450 μs, and 30-millisecond spray and 20-millisecond delay of dynamic cooling. The round laser spots were overlapped 10%. The EYFL was set at a depth of 150 μm with 5.5% coverage, coagulation 1 and a scanning area of 8 × 8 mm (spot 2). Two passes of EYFL were made over the entire scar.
Photographic documentation under identical camera settings (Sony DSC-H9, 8.1 megapixels, high resolution setting, 3253 × 2448; Sony Corp., Tokyo, Japan) were obtained at baseline, before each treatment session, and 1 month after the final treatment. Two blinded dermatologists assessed the degree of pigmentation, vascularity, height, and pliability of scars using the Vancouver Scar Scale (VSS) (Citation2). The post-treatment VSS scores (one measured after three sessions of PDL and the other after three sessions of EYFL) were compared with the VSS measurements made at baseline and those following three sessions of PDL, respectively, to determine whether PDL and EYFL improved, made no changes, or worsened the scar (). Patients were asked about their overall rates of satisfaction along a 4-point scale (4 = very satisfied, 3 = satisfied, 2 = slightly satisfied, and 1 = unsatisfied).
Results
After three sessions of PDL, 10 patients showed improvement in their VSS scores compared to baseline (83.3%). The VSS scores worsened in the remaining two patients (16.7%), who experienced slight elevation and widening of the initially flat scar. Following treatment with EYFL, there was further improvement in the clinical appearance of the scars in eight patients (66.7%), no change in three patients (25%), and worsening of the scar in one patient (8.3%) ().
The patients’ degree of satisfaction, determined by the surveys, showed that three patients were very satisfied (25%), six were satisfied (50%), one was slightly satisfied (8.3%), and two were unsatisfied (16.7%) following three sessions of PDL. With EYFL, four patients were very satisfied (33.3%), four were satisfied (33.3%), three were slightly satisfied (25%), and one was unsatisfied (8.3%) ().
Side effects observed were pain during treatment, post-treatment erythema, edema and pin-point crusting, which were mostly related to EYFL.
Discussion
Recently, focus has been made on laser scar prevention. Fresh surgical scars have been treated with PDLs with success (Citation3,Citation4) and, in a study by Choe et al., a non-ablative, 1550-nm fractional erbium-glass laser (NAFL) was used on new thyroidectomy scars with positive results (Citation5). However, the effect of an ablative fractional laser on scar prevention has not been studied yet.
In this pilot study, a combined approach of PDL and ablative fractional laser (EYFL) was made on fresh surgical scars. Unlike NAFL, EYFL produces mico-columns of skin ablation, which has raised concerns of additional scarring if performed at an early stage of scar remodeling. Therefore, instead of initiating EYFL treatment directly on fresh surgical scars, EYFL treatment was designed to follow three full sessions of PDL, allowing time for the wound to heal. Three sessions of PDL, each 1 month apart, have been necessary to improve the appearance of surgical scars in previous reports, and was also adopted in our study (Citation3,Citation4,Citation6). We operated EYFL at a depth of 150 μm, which is one-third to one-quarter of the depth used for atrophic acne scars, to minimize the risk of secondary scarring. With EYFL set at a shallow ablation depth, we thought that it would be necessary to perform multiple sessions of treatment to achieve a beneficial effect. Therefore, three sessions of EYFL were planned, each 1 month apart.
In our small number of cases, both PDL and EYFL were found to have positive effects on fresh surgical scars. PDL, in general, improved the erythema of scars greatly (). However, there were a few cases where PDL alone was not sufficient in preventing the volume increase (the height and width) of the scar. The volume increase of the scar seems to be largely dependent on the individual's skin characteristics, and in such cases a combined therapy with topical gel sheets and intralesional injection should be recommended at an early stage.
Figure 1. Clinical photographs of the fresh surgical scar at (A) baseline, (B) 1 month after three sessions of PDL, and (C) 1 month after three sessions of EYFL in patient 9 (left) and patient 6 (right).
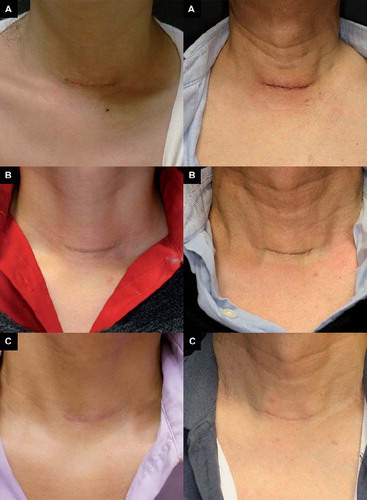
EYFL scheduled after PDL, and set at a shallow ablation depth, resulted in further improvement of scars, especially in terms of ‘pliability’. Also, the incision lines became less prominent after EYFL (). However, there was persistence of erythema in many cases, which was the major drawback associated with EYFL. We did not experience secondary scarring following EYFL, except for one patient who noticed further elevation of the scar. In this particular patient, the volume increase started during PDL therapy, so it is unlikely that EYFL was the sole cause of scar elevation. One of the main concerns with ablative fractional laser in scar treatment has been the trigger of an overzealous healing response resulting in a hypertrophic scar. But from our experience, we feel that the ablative fractional laser can be safely used in fresh surgical scars with control of depth.
A limitation of this uncontrolled study is that all patients had fresh surgical scars. One could argue that these scars would have improved on their own because scars undergo remodeling for up to 6 plus months (Citation7). Future controlled studies are needed, but in our small number of pilot cases, both PDL and EYFL proved to have some positive effect on operation scars when compared to random patients who received no treatment (). In addition, we observed that EYFL, with control of its ablation depth, could be safely used on surgical scars. However, patients with a history of hypertrophic scarring or keloids were excluded from our study and caution should be made with the use of EYFL in this population.
Figure 2. Clinical photographs of random patients with thyroid operation scars (< 1 year) who did not receive any treatment.

Since EYFL causes prolonged erythema, a comparative trial starting with EYFL followed by PDL may be performed in future on fresh surgical scars. In addition, controlled studies with both or either PDLs and ablative fractional lasers at various settings should be conducted to better understand the efficacy of the lasers in scar prevention.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Young VL, Hutchison J. Insights into patient and clinician concerns about scar appearance: Semiquantitative structured surveys. Plast Reconstr Surg. 2009;124:256–265.
- Baryza MJ, Baryza GA. The Vancouver Scar Scale: An administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16:535–538.
- Nouri K, Rivas MP, Stevens M, . Comparison of the effectiveness of the pulsed dye laser 585 nm versus 595 nm in the treatment of new surgical scars. Lasers Med Sci. 2009;24:801–810.
- Nouri K, Jimenez GP, Harrison-Balestra C, Elgart GW. 585 nm pulsed dye laser in the treatment of surgical scars starting on the suture removal day. Dermatol Surg. 2003;29:65–73.
- Choe JH, Park YL, Kim BJ, . Prevention of thyroidectomy scar using a new 1550 nm fractional erbium-glass laser. Dermatol Surg. 2009;35:1199–1205.
- Alam M, Pon K, Van Laborde S, Kaminer MS, Arndt KA, Dover JS. Clinical effect of a single pulsed dye laser treatment of fresh surgical scars: Randomized controlled trial. Dermatol Surg. 2006;32:21–25.
- Kunishige JH, Katz TM, Goldberg LH, Friedman PM. Fractional photothermolysis for the treatment of surgical scars. Dermatol Surg. 2010;36:538–541.
