Abstract
Objective: Age-related hearing loss is an increasingly important public health problem affecting approximately 40% of 55–74 year olds. The primary clinical management intervention for people with hearing loss is hearing aids, however, the majority (80%) of adults aged 55–74 years who would benefit from a hearing aid, do not use them. Furthermore, many people given a hearing aid do not wear it. The aim was to collate the available evidence as to the potential reasons for non-use of hearing aids among people who have been fitted with at least one. Design: Data were gathered via the use of a scoping study. Study sample: A comprehensive search strategy identified 10 articles reporting reasons for non-use of hearing aids. Results: A number of reasons were given, including hearing aid value, fit and comfort and maintenance of the hearing aid, attitude, device factors, financial reasons, psycho-social/situational factors, healthcare professionals attitudes, ear problems, and appearance. Conclusions: The most important issues were around hearing aid value, i.e. the hearing aid not providing enough benefit, and comfort related to wearing the hearing aid. Identifying factors that affect hearing aid usage are necessary for devising appropriate rehabilitation strategies to ensure greater use of hearing aids.
Key Words::
Age-related hearing loss is the most common form of sensorineural hearing loss (Gratton & Vazquez, Citation2003). A review of the prevalence of age-related hearing loss in Europe (Roth et al, Citation2011) found that by age 70 years approximately 30% of men and 20% of women have a pure-tone average (PTA) hearing loss of 30 dB or more in the better ear, and 55% of men and 45% of women by age 80 years. Problems with hearing and communicating are frustrating, and impact on the affected individuals as well as other people in their environment (Arlinger, Citation2003). It has been firmly established that hearing loss is associated with poor quality of life among older people (Chia et al, Citation2007; Heine & Browning, Citation2004), and may even lead to poor general health and mood disorders such as depression and anxiety (Gopinath et al, Citation2009), as well as increased mortality risk (Karpa et al, Citation2010).
The primary clinical management intervention for people with hearing loss is hearing aids but not all people with some measurable form of hearing loss are candidates for hearing aids (Kochkin, Citation2009). There are a number of interventions for people with hearing loss, such as auditory rehabilitation, counselling, education, and assistive listening devices. For those who are candidates, the average age of a first time hearing aid user is 74 years old, with many having suffered a significant hearing loss for an average of 10 years before receiving a hearing aid (Davis et al, Citation2007). Despite the negative consequences associated with hearing loss, only one out of five people who could benefit from a hearing aid actually wears one (World Health Organization, Citation2006). Based on data from the 1999–2006 cycles of the National Health and Nutritional Examination Surveys (NHANES) in the United States, Chien and Lin (Citation2012) report that one in seven individuals aged 50 years or older with a hearing loss uses a hearing aid. Overall, the prevalence of hearing aid use increases with every age decade from 4.3% for adults aged 50–59 years, to 22.1% for adults aged 80 years and older. Chien and Lin (Citation2012) estimate that nearly 23 million adults in the United States have a hearing loss (PTA 25 dB hearing level or greater in both ears) but do not use hearing aids.
Numerous studies have examined hearing aid usage, including a recent systematic review of studies measuring and reporting hearing aid usage in older adults since 1999 (Perez & Edmonds, Citation2012). They found there was a lack of consistency and robustness in the way that usage of hearing aids was assessed and categorized. Fifteen different methods were identified for assessing the usage of hearing aids, so it is clear that there is no standard tool for evaluating hearing aid usage. Furthermore, historically, hearing aid ownership and regular use of hearing aids has been found to be low (Popelka et al, Citation1998; Upfold & Wilson, Citation1980; Weiss, Citation1973) and the numbers of people given a hearing aid who do not wear it/them ranges from 4.7% (Hougaard & Ruf, Citation2011) to 24% (Hartley et al, Citation2010).
In the 1980s, (pre-digital hearing aid era) in a follow up study of 150 people fitted with a hearing aid in Finland, 23% reported never wearing their hearing aid two years after they had been fitted (Sorri et al, Citation1984). The reasons given included trouble handling the aid and little opportunity to converse with others. Brooks (Citation1985) also found that reasons given for non-use of hearing aids included difficulty inserting the ear mould, difficulty coping with signals in noise, lack of recognition of hearing loss, advanced age and poor health, and less than ideal matching of the aid to the loss of hearing. It might be expected that nearly three decades later, reasons for non-use of hearing aids might be quite different, especially given the improvements in hearing aids typically available. Digital hearing aids now offer a number of advantages over analogue hearing aids including increased comfort; digital feedback reduction; digital noise reduction; digital speech enhancement, automatically switching listening programmes, directional microphones, and remote controls, as well as smaller size and open fit design. Benefits of digital hearing aids also include improved sound quality, multiple listening programs for different listening environments, compatibility with remote control options, and flexibility in manipulation of the frequency, compression, and gain (Davis, Citation2001). As such, audiologists now have greater flexibility in choosing appropriate technology for the needs of older adults.
Despite the improvements in hearing aids, usage is still low and the underuse of hearing aids among older adults is still of significant concern. Hearing aid usage has been found to improve quality of life issues, specifically improving communication in relationships; intimacy and warmth in family relationships; emotional stability; sense of control over life events; perception of mental functioning and physical health (Kochkin, Citation2012). If a patient does not wear their hearing aid then it could impact on their quality of life as well as others around them, and may also increase their risk of depression and anxiety (Gopinath et al, Citation2009). In countries where there is access to quality audiological services, it is imperative to resolve why people fail to use their hearing aids (Goulios & Patuzzi, Citation2008). Identifying factors that affect hearing aid usage is necessary for devising appropriate rehabilitation strategies to ensure greater use of hearing aids.
The majority of literature on the reasons for non-use of hearing aids was published before the introduction of digital hearing aids in the NHS in the UK. Given that digital hearing aids were designed to offer practical and clinical advantages over analogue hearing aids it might therefore be reasonable to expect an increase in the numbers of people wearing their hearing aids over this period. Yet this has not happened. The reasons are not clear as to why some people who need hearing aids and possess them do not use them. Therefore there is a need to look at the literature over the past decade examining the reasons for non-use of hearing aids. We might also expect a difference in reasons for non-use between gender and age, considering that women report a higher prevalence of daily and regular use of hearing aids (Staehelin et al, Citation2011), and Kochkin (Citation1993) found that adults aged 35 to 44 were twice as likely to cite stigma as a reason to reject a hearing aid, compared to adults aged 75 to 84 years old. This review attempts to collate the available evidence as to the potential reasons for non-use of hearing aids among people who have been fitted with them and suggests priority areas for future research based on these findings.
Method
Design
Data were gathered via the use of a scoping study. Scoping studies are becoming an increasingly popular way of reviewing health research evidence (Davis et al, Citation2009), particularly where an area has not been reviewed comprehensively before (Arksey & O’Malley, Citation2005). The purpose is to both map a wide range of literature and to envisage where gaps and innovative approaches may lie (Ehrich et al, Citation2002). Arksey and O’Malley (Citation2005) argue that scoping studies can be undertaken as stand-alone projects in their own right. They differ from a systematic review in that they tend to address broader topics where many different study designs might be applicable, rather than focusing on a well-defined research question. A scoping study also does not attempt to address the quality of the research reviewed (Arksey & O’Malley, Citation2005). However, these features do not mean that scoping studies should be seen as ‘second’ or ‘third best’ to systematic and narrative reviews. They offer the advantage of wider coverage and must still be methodologically rigorous and transparent (Stalker et al, Citation2006). Compared to systematic reviews and meta-analysis, the scoping method is different because the studies included in the review may involve more than one intervention, different types of people, and/or a range of outcome measures. This is particularly important for the aims of our study as it was likely that many studies reporting reasons for non-use of hearing aids may have included this as a secondary or tertiary aim of the paper. Scoping reviews aim to indicate where knowledge has been established and where findings are suggestive but not definitive (Rushton, Citation2004). Furthermore, Arksey & O’Malley (Citation2005) suggest that aims of scoping studies include ‘to summarize and disseminate research findings’, and ‘identifying gaps in the existing research literature’. A scoping study was deemed the most appropriate method for this review as the objective was to list and describe all the possible reasons for non-use of hearing aids among individuals with hearing loss who have been fitted with a hearing aid. The primary aim was to present a summarized overview of all the reasons identified in the literature to inform future research.
Procedure
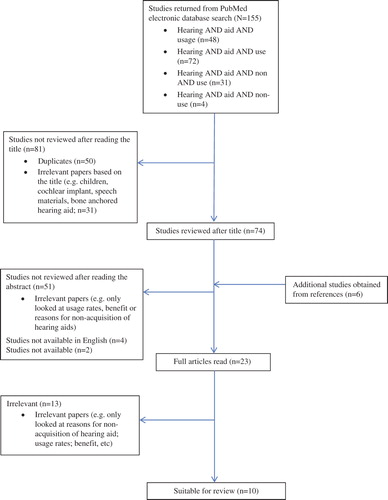
A comprehensive strategy was adopted that involved searching for evidence, both quantitative and qualitative, from various sources. A systematic search of PubMed was conducted using the following search terms in the title:
– Hearing AND aid AND usage
– Hearing AND aid AND use
– Hearing AND aid AND non AND use
– Hearing AND aid AND non-use
This approach was deemed suitable to identify the relevant reasons for non-use of hearing aids that have been reported in studies looking at hearing aid usage. Only studies published since the year 2000 were included. An additional search of Web of Science was carried out which resulted in no further articles. shows the articles identified in the review process. The systematic search of the electronic database PubMed produced 155 articles, of which 74 were deemed potentially suitable after reading the title. An additional six studies were obtained from reference lists and after reading the 80 abstracts, 23 articles were considered for review. Of these 23 articles, only 10 actually reported any reasons for non-use of hearing aids; (the other papers only looked at usage rates, benefit, or reasons for non-acquisition of hearing aids). These were not identified earlier because after reading the abstracts it was still unclear whether the papers reported any information on reasons for non-use of hearing aids, therefore it was considered worthwhile to read the full article. Nine out of the final ten papers were also found in Web of Science. The one that was not found in Web of Science (Kochkin, Citation2000) was also not found in the PubMed search (it was obtained from a reference list). The researchers feel confident that they covered the majority of recent academic journals of interest by searching PubMed and Web of Science.
Results
The final 10 articles are considered here. lists all the papers reviewed and the reasons they identified for non-use of hearing aids. The number of each article also corresponds with the articles listed in .
Table 1. Key characteristics of included articles (in date order).
Table 2. Reasons for non-use of hearing aids as identified in all studies.
Of the ten studies, one was from the UK, three were from the US, two from Australia, two from Finland, one from Sweden, and one from Switzerland. Of all the studies, only three specifically aimed to address the reasons for non-use of hearing aids (Cohen-Mansfield & Taylor, Citation2004; Kochkin, Citation2000; Lupsakko et al, Citation2005). The other studies had different primary aims but mentioned the reasons for non-use of hearing aids as a secondary issue. Primary aims included prevalence rates of hearing aid use (Hartley et al, Citation2010; Gopinath et al, Citation2011; Oberg et al, Citation2012); usage rates of hearing aids (Hartley et al, Citation2010; Gianopoulos et al, Citation2002; Vuorialho et al, Citation2006); a comparison of elderly people with hearing loss and elderly people without hearing loss on a range of demographic, health, and functional factors (Tomita et al, Citation2001); and an investigation of the efficiency of the Swiss hearing aid dispensing system (Bertoli et al, Citation2009).
The sample size in the studies ranged from 76 (Vuorialho et al, Citation2006) to 8707 (Bertoli et al, Citation2009), and the numbers of HA non-users ranged from four (Vuorialho et al, Citation2006) to 348 (Kochkin, Citation2000). However, the sample size of hearing aid users or the numbers of people not using the hearing aid was not always clear. Not all studies reported the numbers of non-users. Additionally, in almost half of the studies (Bertoli et al, Citation2009; Cohen-Mansfield & Taylor, Citation2004; Tomita et al, Citation2001; Vuorialho et al, Citation2006) non-users were grouped together with low-use/occasional-use hearing aid users to examine the reasons for non-use of hearing aids. The studies also differed in whether participants responded to predetermined reasons for non-use of hearing aids or whether they gave their own answer. Six studies (Gianopolous et al, 2002; Hartley et al, Citation2010; Kochkin, Citation2000; Lupsakko et al, Citation2005; Tomita et al, Citation2001; Vuorialho et al, Citation2006) had open ended questions relating to reasons for non-use of hearing aids. The remaining studies (Bertoli et al, Citation2009; Cohen-Mansfield & Taylor, Citation2004; Gopinath et al, Citation2011; Oberg et al, Citation2012) all had fixed choices and the option of ‘other’ to write in their own reason.
The age range in the studies varied considerably (from 18 to 99 years). Two studies did not report the age (Cohen-Mansfield & Taylor, Citation2004; Kochkin, Citation2000) and one study recruited people aged 18 years and over (Bertoli et al, Citation2009), with 54.2% over 75 years. The age of the participants in the remaining studies ranged from 49 years and above. The gender ratio was only reported in four of the studies. In two of the studies just over half of the sample were female (Oberg et al, Citation2012; Vuorialho et al, Citation2006) and in the other two studies nearly three-quarters of the sample were female (74.1%, Lupsakko et al, Citation2005; 71.4%, Tomita et al, Citation2001). None of the studies reported whether there were differences between gender or age in terms of reasons for non-use of the hearing aids.
Not all studies reported the length of time since people were fitted with a hearing aid. Among the studies that did report this, the length of time ranged from six months (Vuorialho et al, Citation2006) to between eight and 16 years (Gianopoulos et al, Citation2002). Considering that experienced hearing aid users are more likely to be satisfied with their hearing aid than new hearing aid users (Kochkin et al, Citation2010), the length of time since fitted with a hearing aid may have implications in terms of the reasons for non-use.
In terms of the reasons for non-use of hearing aids, these can be separated into different categories. shows the full list of reasons identified in the 10 studies. These have been listed in order of importance (based on the percentages and numbers given in each of study); however this is not necessarily a definitive order of importance.
A number of different reasons were identified as to why people do not wear their hearing aid(s) when they have been fitted with them. These reasons have been grouped into different categories depending on whether it relates to hearing; the device itself (wearing or handling the aid, and effectiveness of aid); attitudes; personal, situational, and financial factors; appearance; health care professionals' attitudes; ear problems; or recommendations from others. Although the highest response was for the ‘lack of situations necessary for a hearing aid’ with 62.5% reporting this as a reason in Vuorialho et al, (Citation2006) study, this was the only study to report this as a reason. The most significant reasons appear to be associated with ‘hearing aid value/speech clarity’, and ‘fit and comfort of the hearing aid’. Seven studies reported that participants had problems relating to ‘hearing aid value’, the most significant being that the hearing aid does not help or provides poor benefit (Bertoli et al, Citation2009; Gianopoulos et al, Citation2002; Gopinath et al, Citation2011; Hartley et al, Citation2010; Kochkin, Citation2000; Tomita et al, Citation2001; Vuorialho et al, Citation2006). The next most common reason in this category was ‘difficulty in noisy situations/background noise’ with five studies mentioning this . Other reasons include ‘poor sound quality’ (mentioned in two studies) and ‘not suitable for the type of hearing loss’ (mentioned in one study). Eight studies reported that participants found the device uncomfortable (Vuorialho et al, Citation2006; Hartley et al, Citation2010; Cohen-Mansfield & Taylor, Citation2004; Kochkin, Citation2000; Oberg et al, Citation2012; Tomita et al, Citation2001; Bertoli et al, Citation2009; Gopinath et al, Citation2011), and five studies reported that participants indicated needing help putting the device in (Cohen-Mansfield & Taylor, Citation2004; Vuorialho et al, Citation2006; Tomita et al, Citation2001; Hartley et al, Citation2010; Gopinath et al, Citation2011).
Issues to do with care and maintenance of the hearing aid were reported in eight studies, for example, ‘handling problems/manual dexterity’ (Bertoli et al, Citation2009; Gianopoulos et al, Citation2002; Kochkin, Citation2000; Lupsakko et al, Citation2005; Oberg et al, Citation2012); ‘need help changing the batteries’ (Cohen-Mansfield & Taylor, Citation2004; Tomita et al, Citation2001; Vuorialho et al, Citation2006), and problems with ‘volume control adjustment’ (Kochkin, Citation2000; Tomita et al, Citation2001).
Issues relating to the device itself were mentioned in six studies and included ‘hearing aid not working properly/broken’ (Cohen-Mansfield & Taylor, Citation2004; Hartley et al, Citation2010; Kochkin, Citation2000; Lupsakko et al, Citation2005); ‘feedback and whistling’ (Gianopoulos et al, Citation2002; Hartley et al, Citation2010; Kochkin, Citation2000; Tomita et al, Citation2001; Vuorialho et al, Citation2006); ‘disappointment with the hearing aid’ (Oberg et al, Citation2012); ‘hearing aid needs servicing’ (Cohen-Mansfield & Taylor, Citation2004); ‘battery life is too short’ (Kochkin, Citation2000); and ‘poor directivity’ (Kochkin, Citation2000).
Attitude was mentioned in four studies, as participants reported they had no need for a hearing aid or can hear well enough without a hearing aid (Bertoli et al, Citation2009; Kochkin, Citation2000; Lupsakko et al, Citation2005; Oberg et al, Citation2012). Financial reasons were reported in five studies and related to ‘cost of repairs’ (Cohen-Mansfield & Taylor, Citation2004; Kochkin, Citation2000) or ‘cost of batteries’ (Hartley et al, Citation2010; Lupsakko et al, Citation2005; Tomita et al, Citation2001).
Other less common reasons reported for the non-use of hearing aids related to psychosocial factors (hearing aid is a nuisance/hassle; forget to use it; lost it); healthcare professionals attitudes (poor service from dispenser; oversold expectations); appearance; infection/ear problems; and pressure from others to get a hearing aid.
Discussion
The aim of this review was to gather the available evidence on the potential reasons for non-use of hearing aids among people who have been fitted with at least one. This was achieved by means of a scoping study by reviewing previous literature which may have looked at reasons for non-use of hearing aids as either a primary or secondary aim. The results show that there were many different reasons given, with factors relating to hearing aid value and/or fit and comfort of the hearing aid the most commonly reported reasons. More specifically these reasons include the hearing aid not being effective in noisy situations, providing poor benefit or poor sound quality, and not suitable for the type of hearing loss. Factors relating to fit and comfort of the hearing aid include needing help putting the hearing aid in and taking it out, feeling uncomfortable, or experiencing side effects (e.g rashes, itching).
One important issue seems to relate to the care and maintenance of the hearing aid and manual dexterity. The majority of people with a hearing aid are older adults and consequently may have problems handling the device due to limitations in manual dexterity (Erber, Citation2003). Hearing aids are quite small and fiddly devices (to make the device less noticeable and reduce the concern over the appearance of the aid), however this has been to a detriment of the manual dexterity. If the hearing aid user cannot properly insert, remove, and manipulate their hearing aids, they are less likely to wear them. Many people need help changing the batteries or adjusting the volume control because the dials are so awkward. Even experienced hearing aid users have been found to have a poor understanding of how to use their hearing aid (Desjardins & Doherty, Citation2009). Therefore it is important to assess a patient's ability to use their hearing aids.
A major reason why people do not wear their hearing aids when prescribed them seems to be because of discomfort or they do not know how to put them in correctly. These reasons should be relatively straightforward for clinicians to deal with by ensuring the hearing aid fitting process is accompanied by counselling and support from the audiologist in case of problems (Bertoli et al, Citation2009). Some researchers have begun to address this. Ferguson et al (Citation2011), through a participatory approach, found that healthcare professionals and hearing aid users identified practical topics such as hearing aid insertion and removal, hearing aid functions and maintenance as key to aid the new hearing aid users experience. As a consequence they have developed an interactive video tutorial with the aim of enabling patients to assimilate relevant information at their convenience in their own home. This could prove invaluable to first-time hearing aid users as Gianopoulos et al (Citation2002) found that the majority of non-users rejected their aids for reasons amenable to better training in use of the aid. Further rehabilitation could focus on the problems hearing aid users have to develop individual management plans, and it has been suggested that one-year follow up appointments after hearing aid fitting are appropriate to cover rehabilitation issues and improve usage rates (Goggins & Day, Citation2009). It would seem that, in terms of increasing hearing aid usage, support and counselling may be more important than expensive modern technology (Gianopoulos et al, Citation2002). Vuorialho et al (Citation2006) found that follow up counselling on hearing aid use can significantly increase the benefit obtained from a hearing aid. What is interesting to note is that one study (Kochkin, Citation2000) reported that people had concerns with healthcare professionals in that they had received poor service from their dispenser or they had been oversold expectations of the hearing aid. The best practices employed by hearing healthcare professionals play a significant role in the success of the patient's hearing aid experience and journey (Kochkin et al, Citation2010). Therefore it is important that the right support, information, and counselling is given at the time of hearing aid fitting.
Financial reasons for not wearing a hearing aid were reported in half of the studies. Only one study was from the UK, where healthcare is free at point of delivery and this study did not report financial reasons. Interestingly, appearance of the hearing aid was only noted in three studies as a reason for non-use of the hearing aid and was reported by a small percentage of participants in each of these three studies. This low incidence is noteworthy as stigma has often been thought of as a major reason why people do not wear their hearing aids. However in this review ‘appearance’ was one of the least important reasons. Instead it may be more likely that appearance is a significant barrier to acquisition of a hearing aid because people who are concerned about what it looks like may be less inclined to get their hearing checked and subsequently be fitted with a hearing aid. Stigma has been found to be a predictor of hearing aid uptake (Meister et al, Citation2008), however, a recent systematic review (Jenstad & Moon, Citation2011) reported that stigma is inconsistent in terms of its predictability power, as some studies report stigma as the highest concern (Franks & Beckmann, Citation1985), while others found that stigma only accounted for a small amount of the variability (Meister et al, Citation2008). The age of these studies is likely to have some influence on the findings. Hearing aid designs have changed considerably since 1985 and are much more discrete and unnoticeable so it could be that the appearance and stigma of the hearing aids is not as great as it once was.
One possible approach could have been a meta-analysis, as this is an accepted method of reducing heterogeneous research to an integrated overview (Swanson & Deshler, Citation2003), involving statistical analysis of a large collection of analysis results from individual studies. However, in the majority of the studies the reasons reported for not wearing a hearing aid was a minor section and not the primary aim of the paper. Additionally, the fact we were not concentrating on a single outcome variable or intervention made the statistical techniques of meta-analysis inappropriate. The systematic review methodology is also limited in its guidelines for appraising and extracting data from qualitative studies (Dixon Woods & Fitzpatrick, Citation2001). Since the majority of the studies used a qualitative approach to find out why people do not wear their hearing aids, a systematic review was not considered appropriate. The scoping method is appropriate to identify gaps and was deemed the most appropriate method for our particular aims. One of the strengths of a scoping study is that it provides a thorough overview of areas of research (Arskey & O’Malley, 2005). However, there are a number of limitations of this study to consider: First of all there was no critical review of the individual studies themselves, and assessment of the quality of the data was not possible. However, scoping studies are exploratory and they differ from systematic and meta-analysis reviews in that the criteria for exclusion and inclusion are not based on quality of the studies, but on relevance. The studies varied considerably in the total sample size, number of hearing aid owners, number of hearing aid users and non-users, and length of time owning a hearing aid, as well as methodologically in how the data on reasons for non-use of hearing aids was acquired. As such this is a descriptive account of the reasons why people do not wear their hearing aid(s) after they have been fitted with at least one; it is not to be taken as a critical analysis of the current research. However, such limitations are in the nature of scoping studies. Arskey and O’Malley (2005, p.27) report that ‘the scoping study does not seek to assess quality of evidence and consequently cannot determine whether particular studies provide robust or generalizable findings’. Research into the reasons for non-use of hearing aids when fitted with at least one is essential if appropriate intervention programmes are to be designed to increase hearing aid usage. Because of the broad inclusion criteria compared to a meta-analysis or systematic review, the search strategy can help researchers identify gaps in the existing research.
It is also worth pointing out that the studies in this review were international, and different countries will vary in their provision of hearing aids. For example, in countries where hearing aids and batteries are free, the financial reasons identified may not apply but may carry more importance in countries where this is not free.
We also searched the major medical science databases and identified no additional articles in Web of Science after initially searching PubMed. We are confident that all relevant articles were identified and we are confident that this review has highlighted the most common reasons as to why people fitted with hearing aids choose not to wear them.
Interestingly, it is worth noting that none of the studies reported whether there were differences between gender or age in terms of reasons for non-use of the hearing aids. To date, there has been very little research examining the differences between men and women in the use of hearing aids. The underlying reasons for not using hearing aids may differ between males and females, and a consideration of such factors could potentially increase hearing aid use. Furthermore, not all the studies reported the length of time since people were fitted with a hearing aid. This may have implications in terms of the reasons for non-use, i.e. whether people give up straight away or whether people persevere for a few months/years before giving up with the hearing aid. There is some research to suggest that if people are still using their hearing aids after one year, they remain a hearing aid user (Schumacher & Carruth, Citation1997), however this information does need updating.
Conclusions
The use of a scoping study allowed the inclusion of a broad range of literature and at the same time identified priority areas to explore further, and possible topics for both meta-analysis and systematic reviews that require a more narrowly defined research question. As a result of this scoping study, we recommend that areas for future research on reasons for non-use of hearing aids should focus on hearing aid value; fit and comfort of the hearing aid; care and maintenance of the hearing aid; attitudes and device factors. Researchers interested in hearing aid usage should conduct empirical research to examine specifically what it is about each of these five areas that could be improved to increase hearing aid usage rates among patients. Researchers should also look at how non-use of hearing aids and reasons for non-use vary between gender and age. Gender and/or age differences may have important implications for hearing care and rehabilitative intervention and, as such, require further study. The same can be applied to differences in the length of time a person was fitted with a hearing aid before stopping using it. It is hoped that this study suggests ways forward and can help researchers set agendas for future research looking at the non-use of hearing aids.
Declaration of interest: The authors report no confl icts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Arlinger S. 2003. Negative consequences of uncorrected hearing loss: A review. Int J Audiol, 42(Suppl. 2), 2S17–2S20.
- Arksey H. & O’Malley L. 2005 Scoping studies: Towards a methodological framework. Int J Soc Res Meth, 8, 19–32.
- Bertoli S., Staehelin K., Zemp E., Schindler C., Bodmer D. et al. 2009. Survey on hearing-aid use and satisfaction in Switzerland and their determinants. Int J Audiol, 48, 183–195.
- Brooks D.N. 1985. Factors relating to the under-use of postaural hearing aids. Br J Audiol, 19, 211–217.
- Chia E.M., Wang J.J., Rochtchina E., Cumming R.R., Newall P. et al. 2007. Hearing impairment and health-related quality of life: the Blue Mountains Hearing Study. Ear Hear, 28, 187–195.
- Chien W. & Lin F.R. 2012. Prevalence of hearing-aid use among older adults in the United States. Arch Intern Med, 172, 292–293.
- Cohen-Mansfield J. & Taylor J.W. 2004. Hearing aid use in nursing homes, Part 2: Barriers to effective utilization of hearing aids. J Am Med Direct Assoc, 5, 289–296.
- Davis K., Drey N. & Gould D. 2009. What are scoping studies? A review of the nursing literature. Int J Nurs Stud, 46, 1386–1400.
- Davis A., Smith P., Ferguson M., Stephens D., Gianopoulos I. 2007. Acceptability, benefit, and costs of early screening for hearing disability: A study of potential screening tests and models. Health Technol Assess, 11, 1–294.
- Davis W.E. 2001. Proportional frequency compression in hearing instruments. The Hearing Review, Feb, 34–42.
- Desjardins J.L. & Doherty K.A. 2009. Do experienced hearing-aid users know how to use their hearing aids correctly? Am J Audiol, 18, 69–76.
- Dixon Woods M. & Fitzpatrick R. 2001. Qualitative research in systematic reviews. BMJ, 323, 765–66.
- Ehrich K., Freeman G., Richards S., Robinson I. & Shepperd S. 2002. How to do a scoping exercise: Continuity of care. Res Pol Plan, 20, 25–29.
- Erber N.P. 2003. Use of hearing aids by older people: Influence of non-auditory factors (vision, manual dexterity). Int J Audiol, 42, S21–S25.
- Ferguson M., Leighton P.A., Brandreth M.E. & Wharrad H.J. 2011. Development of evidence-based interactive videos for first-time hearing-aid users. Presented at the British Society of Audiology Conference, Nottingham, September 2011.
- Franks J.R. & Beckman N.J. 1985. Rejection of hearing aids: Attitudes of a geriatric sample. Ear Hear, 6, 161–166.
- Gianopoulos I., Stephens D. & Davis A. 2002. Follow up of people fitted with hearing aids after adults hearing screening: The need for support after fitting. BMJ, 325, 471.
- Goggins S. & Day J. 2009. Pilot study: Efficacy of recalling adult hearing-aid users for reassessment after three years within a publicly-funded audiology service. Int J Audiol, 48, 204–210.
- Gopinath B., Schneider J., Hartley D., Teber E., McMahon C.M. et al. 2011. Incidence and predictors of hearing-aid use and ownership among older adults with hearing loss. Annals of Epidemiology, 21, 497–506.
- Gopinath B., Wang J.J., Schneider J., Burlutsky G., Snowdon J. et al. 2009. Depressive symptoms among older hearing-impaired adults: the Blue Mountains Study. J Am Geriatr Soc, 57, 1306–1308.
- Goulios H. & Patuzzi R.B. 2008. Audiology education and practice from an international perspective. Int J Audiol, 47, 647–664.
- Gratton M.A. & Vazquez A.E. 2003. Age-related hearing loss: Current research. Curr Opin Otolaryngol Head Neck Surg, 11, 367–371.
- Hartley D., Rochtchina E., Newall P., Golding M. & Mitchell P. 2010. Use of hearing aids and assistive listening devices in an older Australian population. J Am Acad Audiol, 21, 642–653.
- Heine C. & Browning C. 2004. The communication and psychosocial perceptions of older adults with sensory loss: A qualitative study. Ageing & Society, 24, 113–130.
- Hougaard S. & Ruf S. 2011. EuroTrak 1: A consumer survey about hearing aids in Germany, France, and the UK. Hearing Review, 18, 12–28.
- Jenstad L. & Moon J. 2011. Systematic review of barriers and facilitators to hearing-aid uptake in older adults. Audiol Res, 1, e25, 91–96.
- Karpa M.J., Gopinath B., Beath K., Rochtchina E., Cumming R.G. et al. 2010. Associations between hearing impairment and mortality risk in older persons: The Blue Mountains Hearing Study. Ann Epidemiol, 20, 452–459.
- Kochkin S. 2012. Hearing loss treatment. Better Hearing Institute. Available at: http://www.betterhearing.org/hearing_loss_treatment/index.cfm (accessed on 30th October 2012).
- Kochkin S. 1993. MarkeTrak III: Why 20 million in US don't use hearing aids for their hearing loss. The Hearing Journal, 46, 28–31.
- Kochkin S. 2000. MarkeTrak V: ʽWhy my hearing aids are in the drawer': The consumers’ perspective. The Hearing Journal, 53, 34–41.
- Kochkin S. 2009. MarkeTrak VIII: 25-year trends in the hearing health market. Hearing Review, October, 12–31.
- Kochkin S., Beck D.L., Christensen L.A., Compton-Conley C., Fligor et al. 2010. MarkeTrak VIII: The impact of the hearing healthcare professional on hearing-aid user success. Hearing Review, 17, 12–34.
- Lupsakko T.A., Kautiainen H.J. & Sulkava R. 2005. The non-use of hearing aids in people aged 75 years and over in the city of Kuopio in Finland. Europ Arch Otorhinolaryngol, 262, 165–169.
- Meister H., Walger M., Brehmer D., von Wedel U. & von Wedel H. 2008. The relationship between pre-fitting expectations and willingness to use hearing aids. Int J Audiol, 47, 153–159.
- Oberg M., Marcusson J., Nagga K. & Wressle E. 2012. Hearing difficulties, uptake and outcomes of hearing aids in people 85 years of age. Int J Audiol, 51, 108–115.
- Perez E. & Edmonds B.A. 2012. A systematic review of studies measuring and reporting hearing-aid usage in older adults since 1999: A descriptive summary of measurement tools. PLoS ONE, 7, e31831. doi:10.1371/journal.pone.0031831
- Popelka M.M., Cruickshanks K.J., Wiley T.L., Tweed T.S., Klein B.E. et al. 1998. Low prevalence of hearing-aid use among older adults with hearing loss: The Epidemiology of Hearing Loss Study. J Am Geriatr Soc, 46, 1075–1078.
- Roth T.N., Hanebuth D. & Probst R. 2011. Prevalence of age-related hearing loss in Europe: A review. Euro Arch Otorhinolaryngol, 268, 1101–1107.
- Rushton A. 2004. A scoping and scanning review of research on the adoption of children placed from public care. Clin Child Psychol Psychiatry, 9, 89–106.
- Schumacher D.U. & Carruth J.A. 1997. Long-term use of hearing aids in patients with presbycusis. Clin Otolaryngol Allied Sci, 22, 430–433.
- Sorri M., Luotonen M. & Laitakari K. 1984. Use and non-use of hearing aids. Br J Audiol, 18, 169–172.
- Staehelin K., Bertoli S., Probst R., Schindler C., Dratva J. et al. 2011. Gender and hearing aids: Patterns of use and determinants of nonregular use. Ear Hear, 32, e26–e37.
- Stalker K., Davidson J., MacDonald C. & Innes A. 2006. A scoping study on the needs of, and services to, younger disabled people including those with early onset dementia in Scotland. Scottish Executive Social Research. Social Work Research Centre, Department of Applied Social Science, University of Stirling.
- Swanson H.L. & Deshler D. 2003. Instructing adolescents with learning disabilities: Converting meta-analysis to practice. Journal of Learning Disabilities, 36, 124–135.
- Tomita M., Mann W.C. & Welch T.R. 2001. Use of assistive devices to address hearing impairment by older persons with disabilities. Int J Rehab Res, 24, 279–289.
- Upfold L.J. & Wilson D.A. 1980. Hearing-aid distribution and use in Australia. The Australian Bureau of Statistics 1978 Survey. Aust J Audiol, 2, 31–36.
- Vuorialho A., Karinen P. & Sorri M. 2006. Counselling of hearing-aid users is highly cost-effective. Euro Arch Otorhinolaryngol, 263, 988–995.
- Weiss C.E. 1973. Why more of the aged with auditory deficits do not wear hearing aids. J Am Geriatr Soc, 21, 139–141.
- World Health Organization. Deafness and hearing impairment. Fact sheet No. 300, 2006 from http://www.who.int/mediacentre/factsheets/fs300/en/index.html